Abstract
Background
to date, no standardized, evidence-based follow-up schemes exist for the monitoring of patients who underwent focal therapy (FT) and expert centers rely mainly on their own experience and/or institutional protocols. We aimed to perform a comprehensive review of the most advantageous follow-up strategies and their rationale after FT for prostate cancer (PCa).
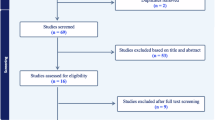
Methods
a narrative review of the literature was conducted to investigate different follow-up protocols of FT for PCa. Outcomes of interest were post-ablation oncological and functional outcomes and complications.
Results
Oncological success after FT was generally defined as the biopsy-confirmed absence of clinically significant PCa in the treated zone. De novo PCa in the untreated area usually reflects an inaccurate patient selection and should be treated as primary PCa. During follow-up, oncological outcomes should be evaluated with periodic PSA, multiparametric MRI and prostate biopsy. The use of PSA derivatives and new biomarkers is still controversial and therefore not recommended. The first MRI after FT should be performed between 6-12 months to avoid ablation-related artifacts and diagnostic delay in case of FT failure. Other imaging modalities, such as PSMA PET/CT scan, are promising but still need to be validated in the post-FT setting. A 12-month “for-protocol” prostate biopsy, including targeted and systematic biopsy, was generally considered the preferred biopsy method to rule out tumor persistence/recurrence. Subsequent mpMRIs and biopsies should follow a risk-adapted approach depending on the clinical scenario. Functional outcomes should be periodically assessed using validated questionnaires within the first year, when typically recover to a new baseline. Complications, despite uncommon, should be strictly monitored mainly in the first month.
Conclusions
FT follow-up is a multifaceted process involving clinical, radiological, and histological assessment. Studies evaluating the impact of different follow-up strategies and ideal timings are needed to produce standardized protocols following FT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Shah TT, Peters M, Eldred-Evans D, Miah S, Yap T, Faure-Walker NA, et al. Early-medium-term outcomes of primary focal cryotherapy to treat nonmetastatic clinically significant prostate cancer from a prospective multicentre registry. Eur Urol. 2019;76:98–105.
Reddy D, Peters M, Shah TT, van Son M, Tanaka MB, Huber PM, et al. Cancer control outcomes following focal therapy using high-intensity focused ultrasound in 1379 men with nonmetastatic prostate cancer: a multi-institute 15-year experience. Eur Urol. 2022;81:407–13. https://doi.org/10.1016/j.eururo.2022.01.005.
Hamdy FC, Donovan JL, Lane JA, Metcalfe C, Davis M, Turner EL, et al. Fifteen-year outcomes after monitoring, surgery, or radiotherapy for prostate cancer. N. Engl J Med. 2023;388:1547–58. https://doi.org/10.1056/NEJMoa2214122.
Connor MJ, Gorin MA, Ahmed HU, Nigam R. Focal therapy for localized prostate cancer in the era of routine multi-parametric MRI. Prostate Cancer Prostat Dis. 2020;23:232–43. https://doi.org/10.1038/s41391-020-0206-6.
Tay KJ, Amin MB, Ghai S, Jimenez RE, Kench JG, Klotz L, et al. Surveillance after prostate focal therapy. World J Urol. 2019;37:397–407. https://doi.org/10.1007/s00345-018-2363-y.
Postema AW, De Reijke TM, Ukimura O, Van den Bos W, Azzouzi AR, Barret E, et al. Standardization of definitions in focal therapy of prostate cancer: report from a Delphi consensus project. World J Urol. 2016;34:1373–82. https://doi.org/10.1007/s00345-016-1782-x.
Lebastchi AH, George AK, Polascik TJ, Coleman J, de la Rosette J, Turkbey B, et al. Standardized nomenclature and surveillance methodologies after focal therapy and partial gland ablation for localized prostate cancer: an international multidisciplinary consensus. Eur Urol. 2020;78:371–8. https://doi.org/10.1016/j.eururo.2020.05.018.
van den Bos W, Muller BG, Ahmed H, Bangma CH, Barret E, Crouzet S, et al. Focal therapy in prostate cancer: international multidisciplinary consensus on trial design. Eur Urol. 2014;65:1078–83. https://doi.org/10.1016/j.eururo.2014.01.001.
Mottet N, Cornford P, van den Bergh RCN, Briers E, Eberli D, De Meerleer G, et al. EAU-EANM-ESTRO-ESUR-ISUP-SIOG Guidelines on Prostate Cancer 2023. Edn. presented at the EAU Annual Congress Milan 2023. ISBN 978-94-92671-19-6. Available from: https://uroweb.org/guidelines/prostate-cancer
Eastham JA, Auffenberg GB, Barocas DA, Chou R, Crispino T, Davis JW, et al. Clinically localized prostate cancer: AUA/ASTRO guideline, part II: principles of active surveillance, principles of surgery, and follow-up. J Urol. 2022;208:19–25.
Donaldson IA, Alonzi R, Barratt D, Barret E, Berge V, Bott S, et al. Focal therapy: patients, interventions, and outcomes-a report from a consensus meeting. Eur Urol. 2015;67:771–7. https://doi.org/10.1016/j.eururo.2014.09.018.
van Luijtelaar A, Greenwood BM, Ahmed HU, Barqawi AB, Barret E, Bomers JGR, et al. Focal laser ablation as clinical treatment of prostate cancer: report from a Delphi consensus project. World J Urol. 2019;37:2147–53. https://doi.org/10.1007/s00345-019-02636-7.
Marra G, Soeterik T, Oreggia D, Tourinho-Barbosa R, Moschini M, Filippini C, et al. Long-term Outcomes of Focal Cryotherapy for Low- to Intermediate-risk Prostate Cancer: Results and Matched Pair Analysis with Active Surveillance. Eur Urol Focus. 2022;8:701–9. https://doi.org/10.1016/j.euf.2021.04.008.
Kayano PP, Klotz L. Current evidence for focal therapy and partial gland ablation for organ-confined prostate cancer: systematic review of literature published in the last 2 years. Curr Opin Urol. 2021;31:49–57. https://doi.org/10.1097/MOU.0000000000000838.
Breda A, Anterasian C, Belldegrun A. Management and outcomes of tumor recurrence after focal ablation renal therapy. J Endourol. 2010;24:749–52. https://doi.org/10.1089/end.2009.0658.
Scheltema MJ, Geboers B, Blazevski A, Doan P, Katelaris A, Agrawal S, et al. Median 5-year outcomes of primary focal irreversible electroporation for localised prostate cancer. BJU Int. 2023;131:6–13. https://doi.org/10.1111/bju.15946.
Marconi L, Stonier T, Tourinho-Barbosa R, Moore C, Ahmed HU, Cathelineau X, et al. Robot-assisted radical prostatectomy after focal therapy: oncological, functional outcomes and predictors of recurrence. Eur Urol. 2019;76:27–30. https://doi.org/10.1016/j.eururo.2019.03.007.
Van Hemelrijck M, Ji X, Helleman J, Roobol MJ, van der Linden W, Nieboer D, et al. Reasons for discontinuing active surveillance: assessment of 21 centres in 12 countries in the Movember GAP3 Consortium. Eur Urol. 2019;75:523–31. https://doi.org/10.1016/j.eururo.2018.10.025.
Jansen BHE, van Leeuwen PJ, Wondergem M, van der Sluis TM, Nieuwenhuijzen JA, Knol RJJ, et al. Detection of recurrent prostate cancer using prostate-specific membrane antigen positron emission tomography in patients not meeting the Phoenix criteria for biochemical recurrence after curative radiotherapy. Eur Urol Oncol. 2021;4:821–5. https://doi.org/10.1016/j.euo.2020.01.002.
Tourinho-Barbosa RR, Wood BJ, Abreu AL, Nahar B, Shin T, Guven S, et al. Current state of image-guided focal therapy for prostate cancer. World J Urol. 2021;39:701–17. https://doi.org/10.1007/s00345-020-03254-4.
Andolfi C, Vickers AJ, Cooperberg MR, Carroll PR, Cowan JE, Paner GP, et al. Blood prostate-specific antigen by volume of benign, Gleason Pattern 3 and 4 Prostate tissue. Urology. 2022;170:154–60. https://doi.org/10.1016/j.urology.2022.08.014.
Kotamarti S, Séguier D, Arcot R, Polascik TJ. Assessment after focal therapy: what is the latest? Curr Opin Urol. 2022;32:260–6. https://doi.org/10.1097/MOU.0000000000000988.
Oishi M, Gill IS, Tafuri A, Shakir A, Cacciamani GE, Iwata T, et al. Hemigland cryoablation of localized low, intermediate and high risk prostate cancer: oncologic and functional outcomes at 5 years. J Urol. 2019;202:1188–98. https://doi.org/10.1097/JU.0000000000000456.
Kongnyuy M, Islam S, Mbah AK, Halpern DM, Werneburg GT, Kosinski KE, et al. PSA kinetics following primary focal cryotherapy (hemiablation) in organ-confined prostate cancer patients. World J Urol. 2018;36:209–13. https://doi.org/10.1007/s00345-017-2130-5.
Stabile A, Orczyk C, Giganti F, Moschini M, Allen C, Punwani S, et al. The role of percentage of prostate-specific antigen reduction after focal therapy using high-intensity focused ultrasound for primary localised prostate cancer. results from a large multi-institutional series. Eur Urol. 2020;78:155–60. https://doi.org/10.1016/j.eururo.2020.04.068.
Huber PM, Afzal N, Arya M, Boxler S, Dudderidge T, Emberton M, et al. Prostate specific antigen criteria to diagnose failure of cancer control following focal therapy of nonmetastatic prostate cancer using high intensity focused ultrasound. J Urol. 2020;203:734–42. https://doi.org/10.1097/JU.0000000000000747.
Dickinson L, Ahmed HU, Hindley RG, McCartan N, Freeman A, Allen C, et al. Prostate-specific antigen vs. magnetic resonance imaging parameters for assessing oncological outcomes after high intensity-focused ultrasound focal therapy for localized prostate cancer. Urol Oncol. 2017;35:30.e9–30.e15. https://doi.org/10.1016/j.urolonc.2016.07.015.
Khandwala YS, Morisetty S, Ghanouni P, Fan RE, Soerensen SJC, Rusu M, et al. Evaluation of post-ablation mpMRI as a predictor of residual prostate cancer after focal high intensity focused ultrasound (HIFU) ablation. Urol Oncol. 2022;40:489.e9–489.e17. https://doi.org/10.1016/j.urolonc.2022.07.017.
Elshafei A, Tay KJ, Kara O, Malkoc E, Nyame Y, Arora H, et al. Associations between prostate volume and oncologic outcomes in men undergoing focal cryoablation of the prostate. Clin Genitourin Cancer. 2018;16:e477–e482. https://doi.org/10.1016/j.clgc.2017.10.009.
Marra G, Laguna MP, Walz J, Pavlovich CP, Bianco F, Gregg J, et al. Molecular biomarkers in the context of focal therapy for prostate cancer: recommendations of a Delphi Consensus from the Focal Therapy Society. Minerva Urol Nephrol. 2022;74:581–9. https://doi.org/10.23736/S2724-6051.20.04160-0.
Deivasigamani S, Polascik TJ. Personal communication, currently under peer review. May 15, 2024.
Ghafoor S, Becker AS, Stocker D, Barth BK, Eberli D, Donati OF, et al. Magnetic resonance imaging of the prostate after focal therapy with high-intensity focused ultrasound. Abdom Radiol. 2020;45:3882–95. https://doi.org/10.1007/s00261-020-02577-5.
Kulik M, Nedelcu C, Martin F, Lebdai S, Rousselet MC, Azzouzi AR, et al. Post-treatment MRI aspects of photodynamic therapy for prostate cancer. Insights Imaging. 2014;5:697–713. https://doi.org/10.1007/s13244-014-0359-8.
van den Bos W, Scheltema MJ, Siriwardana AR, Kalsbeek AMF, Thompson JE, Ting F, et al. Focal irreversible electroporation as primary treatment for localized prostate cancer. BJU Int. 2018;121:716–24. https://doi.org/10.1111/bju.13983.
Kirkham AP, Emberton M, Hoh IM, Illing RO, Freeman AA, Allen C. MR imaging of prostate after treatment with high-intensity focused ultrasound. Radiology. 2008;246:833–44. https://doi.org/10.1148/radiol.2463062080.
Koopman AGMM, Jenniskens SFM, Fütterer JJ. Magnetic resonance imaging assessment after therapy in prostate cancer. Top Magn Reson Imaging. 2020;29:47–58. https://doi.org/10.1097/RMR.0000000000000231.
Muller BG, Fütterer JJ, Gupta RT, Katz A, Kirkham A, Kurhanewicz J, et al. The role of magnetic resonance imaging (MRI) in focal therapy for prostate cancer: recommendations from a consensus panel. BJU Int. 2014;113:218–27. https://doi.org/10.1111/bju.12243.
Light A, Mayor N, Cullen E, Kirkham A, Padhani AR, Arya M, et al. The Transatlantic Recommendations for Prostate Gland Evaluation with Magnetic Resonance Imaging After Focal Therapy (TARGET): A systematic review and international consensus recommendations. Eur Urol. 2024;S0302-2838:00067–8. https://doi.org/10.1016/j.eururo.2024.02.001.
Guillaumier S, Peters M, Arya M, Afzal N, Charman S, Dudderidge T, et al. A multicentre study of 5-year outcomes following focal therapy in treating clinically significant nonmetastatic prostate cancer. Eur Urol. 2018;74:422–9. https://doi.org/10.1016/j.eururo.2018.06.006.
Stabile A, Orczyk C, Hosking-Jervis F, Giganti F, Arya M, Hindley RG, et al. Medium-term oncological outcomes in a large cohort of men treated with either focal or hemi-ablation using high-intensity focused ultrasonography for primary localized prostate cancer. BJU Int. 2019;124:431–40. https://doi.org/10.1111/bju.14710.
Marra G, Soeterik T, Oreggia D, Tourinho-Barbosa R, Moschini M, Stabile A, et al. Focal high-intensity focused ultrasound vs. active surveillance for ISUP Grade 1 prostate cancer: medium-term results of a matched-pair comparison. Clin Genitourin Cancer. 2022;20:592–604. https://doi.org/10.1016/j.clgc.2022.06.009.
O’Connor LP, Lebastchi AH, Horuz R, Rastinehad AR, Siddiqui MM, Grummet J, et al. Role of multiparametric prostate MRI in the management of prostate cancer. World J Urol. 2021;39:651–9. https://doi.org/10.1007/s00345-020-03310-z.
Schaudinn A, Michaelis J, Franz T, Ho-Thi P, Horn LC, Blana A, et al. High-intensity focused ultrasound (HIFU) hemiablation of the prostate: Late follow-up MRI findings in non-recurrent patients. Eur J Radio. 2021;144:109957 https://doi.org/10.1016/j.ejrad.2021.109957.
van den Bos W, de Bruin DM, van Randen A, Engelbrecht MR, Postema AW, Muller BG, et al. MRI and contrast-enhanced ultrasound imaging for evaluation of focal irreversible electroporation treatment: results from a Phase I–II study in patients undergoing IRE followed by radical prostatectomy. Eur Radio. 2016;26:2252–60.
Turkbey B, Rosenkrantz AB, Haider MA, Padhani AR, Villeirs G, Macura KJ, et al. Prostate imaging reporting and data system version 2.1: 2019 update of prostate imaging reporting and data system Version 2. Eur Urol. 2019;76:340–51. https://doi.org/10.1016/j.eururo.2019.02.033.
Giganti F, Dickinson L, Orczyk C, Haider A, Freeman A, Emberton M, et al. Prostate Imaging after Focal Ablation (PI-FAB): A proposal for a scoring system for multiparametric MRI of the prostate after focal therapy. Eur Urol Oncol. 2023;6:629–34. https://doi.org/10.1016/j.euo.2023.04.007.
Wysock JS, Becher E, Gogaj R, Velazquez N, Lepor H. Early oncological control following partial gland cryo-ablation: a prospective experience specifying reflex MRI guided biopsy of the ablation zone. Prostate Cancer Prostat Dis. 2021;24:114–9. https://doi.org/10.1038/s41391-020-0244-0.
Geboers B, Gondoputro W, Thompson JE, Reesink DJ, van Riel LAMJG, Zhang D, et al. Diagnostic accuracy of multiparametric magnetic resonance imaging to detect residual prostate cancer following irreversible electroporation-a multicenter validation study. Eur Urol Focus. 2022;8:1591–8. https://doi.org/10.1016/j.euf.2022.04.010.
Kaufmann B, Raess E, Schmid FA, Bieri U, Scherer TP, Elleisy M, et al. Focal therapy with high-intensity focused ultrasound for prostate cancer: 3-year outcomes from a prospective trial. BJU Int. 2024;133:413–24. https://doi.org/10.1111/bju.16213.
Ahmed HU, El-Shater Bosaily A, Brown LC, Gabe R, Kaplan R, Parmar MK, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet. 2017;389:815–22. https://doi.org/10.1016/S0140-6736(16)32401-1.
Light A, Kanthabalan A, Otieno M, Pavlou M, Omar R, Adeleke S, et al. The role of multiparametric MRI and MRI-targeted biopsy in the diagnosis of radiorecurrent prostate cancer: an analysis from the FORECAST trial. Eur Urol. 2024;85:35–46. https://doi.org/10.1016/j.eururo.2023.09.001.
Felker ER, Raman SS, Lu DSK, Tuttle M, Margolis DJ, ElKhoury FF, et al. Utility of multiparametric MRI for predicting residual clinically significant prostate cancer after focal laser ablation. Am J Roentgenol. 2019;213:1253–8. https://doi.org/10.2214/AJR.19.21637.
Scheltema MJ, Chang JI, van den Bos W, Böhm M, Delprado W, Gielchinsky I, et al. Preliminary diagnostic accuracy of multiparametric magnetic resonance imaging to detect residual prostate cancer following focal therapy with irreversible electroporation. Eur Urol Focus. 2019;5:585–91. https://doi.org/10.1016/j.euf.2017.10.007.
Thompson JE, Sridhar AN, Tan WS, Freeman A, Haider A, Allen C, et al. Pathological findings and magnetic resonance imaging concordance at salvage radical prostatectomy for local recurrence following partial ablation using high intensity focused ultrasound. J Urol. 2019;201:1134–43. https://doi.org/10.1097/JU.0000000000000135.
Donato P, Morton A, Yaxley J, Ranasinghe S, Teloken PE, Kyle S, et al. 68Ga-PSMA PET/CT better characterises localised prostate cancer after MRI and transperineal prostate biopsy: Is 68Ga-PSMA PET/CT guided biopsy the future? Eur J Nucl Med Mol Imaging. 2020;47:1843–51. https://doi.org/10.1007/s00259-019-04620-0.
Spohn S, Jaegle C, Fassbender TF, Sprave T, Gkika E, Nicolay NH, et al. Intraindividual comparison between 68Ga-PSMA-PET/CT and mpMRI for intraprostatic tumor delineation in patients with primary prostate cancer: a retrospective analysis in 101 patients. Eur J Nucl Med Mol Imaging. 2020;47:2796–803. https://doi.org/10.1007/s00259-020-04827-6.
Roberts MJ, Morton A, Donato P, Kyle S, Pattison DA, Thomas P, et al. 68Ga-PSMA PET/CT tumour intensity pre-operatively predicts adverse pathological outcomes and progression-free survival in localised prostate cancer. Eur J Nucl Med Mol Imaging. 2021;48:477–82. https://doi.org/10.1007/s00259-020-04944-2.
Raveenthiran S, Yaxley WJ, Franklin T, Coughlin G, Roberts M, Gianduzzo T, et al. Findings in 1,123 men with preoperative 68Ga-prostate-specific membrane antigen positron emission tomography/computerized tomography and multiparametric magnetic resonance imaging compared to totally embedded radical prostatectomy histopathology: implications for the diagnosis and management of prostate cancer. J Urol. 2022;207:573–80. https://doi.org/10.1097/JU.0000000000002293.
Pfister D, Haidl F, Nestler T, Verburg F, Schmidt M, Wittersheim M, et al. 68 Ga-PSMA-PET/CT helps to select patients for salvage radical prostatectomy with local recurrence after primary radiotherapy for prostate cancer. BJU Int. 2020;126:679–83. https://doi.org/10.1111/bju.15135.
Alvim R, Nagar K, Das S, Lebdai S, Wong N, Somma A, et al. Positron Emission Tomography/Computed Tomography with Gallium-68-labeled prostate-specific membrane antigen detects relapse after vascular-targeted photodynamic therapy in a prostate cancer model. Eur Urol Focus. 2021;7:472–8. https://doi.org/10.1016/j.euf.2019.06.008.
Blazevski A, Geboers B, Scheltema MJ, Gondoputro W, Doan P, Katelaris A, et al. Salvage irreversible electroporation for radio-recurrent prostate cancer - the prospective FIRE trial. BJU Int. 2023;131:23–31. https://doi.org/10.1111/bju.15947.
Rasing M, van Son M, Moerland M, de Keizer B, Wessels F, Jonges T, et al. Value of targeted biopsies and combined PSMA PET/CT and mp-MRI imaging in locally recurrent prostate cancer after primary radiotherapy. Cancers. 2022;14:781 https://doi.org/10.3390/cancers14030781.
Manfredi C, Fernández-Pascual E, Linares-Espinós E, Couñago F, Martínez-Salamanca JI. New frontiers in focal therapy for prostate cancer: Prostate-specific membrane antigen positron emission tomography/magnetic resonance imaging. World J Clin Oncol. 2021;12:61–68. https://doi.org/10.5306/wjco.v12.i2.61.
Burger IA, Müller J, Donati OF, Ferraro DA, Messerli M, Kranzbühler B, et al. 68Ga-PSMA-11 PET/MR detects local recurrence occult on mpmri in prostate cancer patients after HIFU. J Nucl Med. 2019;60:1118–23. https://doi.org/10.2967/jnumed.118.221564.
Duan H, Ghanouni P, Daniel B, Rosenberg J, Davidzon GA, Aparici CM, et al. A pilot study of 68Ga-PSMA11 and 68Ga-RM2 PET/MRI for evaluation of prostate cancer response to high-intensity focused ultrasound therapy. J Nucl Med. 2023;64:592–7. https://doi.org/10.2967/jnumed.122.264783.
Bacchetta F, Martins M, Regusci S, Jichlinski P, Meuwly JY, Lucca I, et al. The utility of intraoperative contrast-enhanced ultrasound in detecting residual disease after focal HIFU for localized prostate cancer. Urol Oncol. 2020;38:846.e1–846.e7. https://doi.org/10.1016/j.urolonc.2020.05.010.
van den Bos W, de Bruin DM, van Randen A, Engelbrecht MR, Postema AW, Muller BG, et al. MRI and contrast-enhanced ultrasound imaging for evaluation of focal irreversible electroporation treatment: results from a phase I-II study in patients undergoing IRE followed by radical prostatectomy. Eur Radiol. 2016;26:2252–60. https://doi.org/10.1007/s00330-015-4042-3.
van Riel LAMJG, van Kollenburg RAA, Freund JE, Almasian M, Jager A, Engelbrecht MRW, et al. Reliable visualization of the treatment effect of transperineal focal laser ablation in prostate cancer patients by magnetic resonance imaging and contrast-enhanced ultrasound imaging. Eur Urol Open Sci. 2023;54:72–79. https://doi.org/10.1016/j.euros.2023.06.002.
Muller BG, van den Bos W, Brausi M, Fütterer JJ, Ghai S, Pinto PA, et al. Follow-up modalities in focal therapy for prostate cancer: results from a Delphi consensus project. World J Urol. 2015;33:1503–9. https://doi.org/10.1007/s00345-014-1475-2.
Siddiqui MM, Rais-Bahrami S, Turkbey B, George AK, Rothwax J, Shakir N, et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA. 2015;313:390–7. https://doi.org/10.1001/jama.2014.17942.
Tan YG, Law YM, Ngo NT, Khor LY, Tan PH, Ong EHW, et al. Patient-reported functional outcomes and oncological control after primary focal cryotherapy for clinically significant prostate cancer: A Phase II mandatory biopsy-monitored study. Prostate. 2023;83:781–91. https://doi.org/10.1002/pros.24517.
Blazevski A, Scheltema MJ, Yuen B, Masand N, Nguyen TV, Delprado W, et al. Oncological and quality-of-life outcomes following focal irreversible electroporation as primary treatment for localised prostate cancer: a biopsy-monitored prospective cohort. Eur Urol Oncol. 2020;3:283–90. https://doi.org/10.1016/j.euo.2019.04.008.
Ryan P, Finelli A, Lawrentschuk N, Fleshner N, Sweet J, Cheung C, et al. Prostatic needle biopsies following primary high intensity focused ultrasound (HIFU) therapy for prostatic adenocarcinoma: histopathological features in tumour and non-tumour tissue. J Clin Pathol. 2012;65:729–34. https://doi.org/10.1136/jclinpath-2011-200460.
Adams ES, Deivasigamani S, Mottaghi M, Huang J, Gupta RT, Polascik TJ. Evaluation of recurrent disease after radiation therapy for patients considering local salvage therapy: past vs. contemporary management. Cancers. 2023;15:5883 https://doi.org/10.3390/cancers15245883.
Clements MB. How to present quality of life outcomes after focal therapy: using validated instruments and novel statistical methods. Curr Opin Urol. 2022;32:254–9. https://doi.org/10.1097/MOU.0000000000000974.
Shah TT, Peters M, Miah S, Eldred-Evans D, Yap T, Hosking-Jervis F, et al. Assessment of return to baseline urinary and sexual function following primary focal cryotherapy for nonmetastatic prostate cancer. Eur Urol Focus. 2021;7:301–8. https://doi.org/10.1016/j.euf.2019.09.004.
Fallara G, Capogrosso P, Maggio P, Taborelli A, Montorsi F, Dehò F, et al. Erectile function after focal therapy for localized prostate cancer: a systematic review. Int J Impot Res. 2021;33:418–27.
Bakavicius A, Marra G, Macek P, Robertson C, Abreu AL, George AK, et al. Available evidence on HIFU for focal treatment of prostate cancer: a systematic review. Int Braz J Urol. 2022;48:263–74. https://doi.org/10.1590/S1677-5538.IBJU.2021.0091.
Azzouzi AR, Vincendeau S, Barret E, Cicco A, Kleinclauss F, van der Poel HG, et al. Padeliporfin vascular-targeted photodynamic therapy versus active surveillance in men with low-risk prostate cancer (CLIN1001 PCM301): an open-label, phase 3, randomised controlled trial. Lancet Oncol. 2017;18:181–91. https://doi.org/10.1016/S1470-2045(16)30661-1.
Bakavicius A, Sanchez-Salas R, Muttin F, Sivaraman A, Dell’Oglio P, Barret E, et al. Comprehensive evaluation of focal therapy complications in prostate cancer: a standardized methodology. J Endourol. 2019;33:509–15. https://doi.org/10.1089/end.2018.0809.
Schmid FA, Schindele D, Mortezavi A, Spitznagel T, Sulser T, Schostak M, et al. Prospective multicentre study using high intensity focused ultrasound (HIFU) for the focal treatment of prostate cancer: Safety outcomes and complications. Urol Oncol. 2020;38:225–30. https://doi.org/10.1016/j.urolonc.2019.09.001.
Rakauskas A, Marra G, Heidegger I, Kasivisvanathan V, Kretschmer A, Zattoni F, et al. Focal therapy for prostate cancer: complications and their treatment. Front Surg. 2021;8:696242 https://doi.org/10.3389/fsurg.2021.696242.
Fiorella D, Marenco JL, Mascarós JM, Borque-Fernando Á, Esteban LM, Calatrava A, et al. Role of PCA3 and SelectMDx in the optimization of active surveillance in prostate cancer. Actas Urol Esp (Engl Ed) 2021;45:439–46.
Herlemann A, Huang HC, Alam R, Tosoian JJ, Kim HL, Klein EA, et al. Decipher identifies men with otherwise clinically favorable-intermediate risk disease who may not be good candidates for active surveillance. Prostate Cancer Prostat Dis. 2020;23:136–43. https://doi.org/10.1038/s41391-019-0167-9.
Meeks JJ, Kern SQ, Dalbagni G, Eastham JA, Sandhu JS. The prevalence of persistent prostate cancer after radiotherapy detected at radical cystoprostatectomy for bladder cancer. J Urol. 2014;191:1760–3. https://doi.org/10.1016/j.juro.2013.12.037.
Author information
Authors and Affiliations
Contributions
Study concept and design: Marra, Marquis, Polascik. Acquisition of data and reviewing journal articles: Marra, Marquis. Analysis and interpretation of data: All authors. Manuscript Draft: Marra, Marquis. Creating tables and images: All authors. Critical revision/editing of the manuscript: All authors. Supervision: Polascik.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marra, G., Marquis, A., Suberville, M. et al. Surveillance after Focal Therapy – a Comprehensive Review. Prostate Cancer Prostatic Dis 28, 662–671 (2025). https://doi.org/10.1038/s41391-024-00905-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41391-024-00905-0