Abstract
Background
Socioeconomic determinants of health (SDOH) are often unvalued during surgery risk stratification; hence, they might be a major source of disparity that can jeopardize outcomes related to urological surgery. The aim of our study is to evaluate the impact of SDOH on postoperative outcomes following minimally invasive radical prostatectomy (MIRP).
Methods
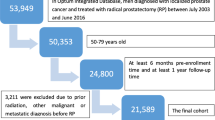
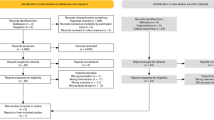
Patients who underwent MIRP between 2011 and 2021 were retrospectively analyzed by using PearlDiver-Mariner, an all-payer insurance claims database. International Classification of Diseases diagnosis and procedure codes were used to identify patient’s characteristics, postoperative complications and SDOH. Outcomes were compared using multivariable regression models.
Results
Overall, 100,035 patients (mean age = 63.24 ± 7.07) underwent MIRP. The 60-day postoperative complication rate was 18%. Approximately 6% of patients reported at least one SDOH at baseline. SDOH were associated with higher odds of 60-day postoperative complications (OR:1.24, 95% CI:1.15–1.34), including urinary tract infection (OR:1.32, 95% CI:1.20–1.45) and acute kidney injury (OR:1.31, 95% CI:1.00–1.39). Postoperative urethral stricture (OR:1.37, 95% CI:0.92–1.98) did not reach statistical significance at multivariable analysis.
Conclusions
Patients with SDOH have a significantly higher risk of postoperative complications following MIRP, especially urinary infection and acute kidney injury. These findings are multifactorial and should prompt identifying measures that might help prevent this large-scale phenomenon.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data presented in this study are available on request from the corresponding author due to privacy policies.
References
Eastham JA, Boorjian SA, Kirkby E. Clinically Localized Prostate Cancer: AUA/ASTRO Guideline. J Urol. 2022;208:505–7.
Tyson MD, Andrews PE, Ferrigni RF, Humphreys MR, Parker AS, Castle EP. Radical Prostatectomy Trends in the United States: 1998 to 2011. Mayo Clin Proc. 2016;91:10–6.
Mao J, Genkinger JM, Rundle AG, Wright JD, Aryal S, Liebeskind AY, et al. Racial and Ethnic Disparities in the Use of Robot-Assisted Surgery and Minimally Invasive Surgery in Pelvic Cancer Treatment: A Systematic Review. Cancer Epidemiol Biomark Prev. 2024;33:20–32.
Morris AM, Rhoads KF, Stain SC, Birkmeyer JD. Understanding Racial Disparities in Cancer Treatment and Outcomes. J Am Coll Surg. 2010;211:105–13.
Hoffman RM, Gilliland FD, Eley JW, Harlan LC, Stephenson RA, Stanford JL, et al. Racial and Ethnic Differences in Advanced-Stage Prostate Cancer: the Prostate Cancer Outcomes Study. JNCI J Natl Cancer Inst. 2001;93:388–95.
Friedlander DF, Trinh Q-D, Krasnova A, Lipsitz SR, Sun M, Nguyen PL, et al. Racial Disparity in Delivering Definitive Therapy for Intermediate/High-risk Localized Prostate Cancer: The Impact of Facility Features and Socioeconomic Characteristics. Eur Urol. 2018;73:445–51.
Nemirovsky DR, Klose C, Wynne M, McSweeney B, Luu J, Chen J, et al. Role of Race and Insurance Status in Prostate Cancer Diagnosis-to-Treatment Interval. Clin Genitourin Cancer. 2023;21:e198–203.
U.S. Department of Health and Human Services O of DP and HP. Healthy People 2030. 2024.
Marmot M, Friel S, Bell R, Houweling TA, Taylor S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372:1661–9.
Graham NJ, Souter LH, Salami SS. A Systematic Review of Family History, Race/Ethnicity, and Genetic Risk on Prostate Cancer Detection and Outcomes: Considerations in PSA-based Screening. Urologic Oncol. 2024;S1078143924005040. Epub ahead of print.
Chestang J, Wang S, Yu JB. Prostate cancer in New York City: impact of neighborhood level social determinants of care. Prostate Cancer Prostatic Dis. 2023;26:628–30.
Pollak YLE, Lee JY, Khalid SI, Aquina CT, Hayden DM, Becerra AZ. Social determinants of health Z-codes and postoperative outcomes after colorectal surgery: A national population-based study. Am J Surg. 2022;224:1301–7.
Dos Santos Marques IC, Theiss LM, Wood LN, Gunnells DJ, Hollis RH, Hardiman KM, et al. Racial disparities exist in surgical outcomes for patients with inflammatory bowel disease. Am J Surg. 2021;221:668–74.
Kelly BD, Perera M, Bolton DM, Papa N. Social determinants of health: does socioeconomic status affect access to staging imaging for men with prostate cancer. Prostate Cancer Prostatic Dis. 2023;26:429–31.
Mahal BA, Chen Y-W, Muralidhar V, Mahal AR, Choueiri TK, Hoffman KE, et al. Racial disparities in prostate cancer outcome among prostate-specific antigen screening eligible populations in the United States. Ann Oncol. 2017;28:1098–104.
Li X, Sundquist K, Sundquist J. Neighborhood deprivation and prostate cancer mortality: a multilevel analysis from Sweden. Prostate Cancer Prostatic Dis. 2012;15:128–34.
Presley CJ, Raldow AC, Cramer LD, Soulos PR, Long JB, Yu JB, et al. A new approach to understanding racial disparities in prostate cancer treatment. J Geriatr Oncol. 2013;4:1–8.
Halbert CH, Weathers B, Delmoor E, Mahler B, Coyne J, Thompson HS, et al. Racial differences in medical mistrust among men diagnosed with prostate cancer. Cancer. 2009;115:2553–61.
Pessoa RR, Maroni P, Kukreja J, Kim SP. Comparative effectiveness of robotic and open radical prostatectomy. Transl Androl Urol. 2021;10:2158–70.
Chandramohan D, Konda R, Pujari A, Avula S, Palleti SK, Jena N, et al. Acute kidney injury after robot‐assisted laparoscopic prostatectomy: A meta‐analysis. Robot Comput Surg. 2024;20:e2630.
Ghazi L, Parcha V, Takeuchi T, Butler CR, Baker E, Oates GR et al. Association of Neighborhood Social Determinants of Health with Acute Kidney Injury during Hospitalization. CJASN. 2024. https://doi.org/10.2215/CJN.0000000000000528.
Siegel DA, O’Neil ME, Richards TB, Dowling NF, Weir HK. Prostate Cancer Incidence and Survival, by Stage and Race/Ethnicity — United States, 2001-2017. MMWR Morb Mortal Wkly Rep. 2020;69:1473–80.
Negoita S, Feuer EJ, Mariotto A, Cronin KA, Petkov VI, Hussey SK, et al. Annual Report to the Nation on the Status of Cancer, part II: Recent changes in prostate cancer trends and disease characteristics. Cancer. 2018;124:2801–14.
Liadi Y, Campbell T, Dike P, Harlemon M, Elliott B, Odero-Marah V. Prostate cancer metastasis and health disparities: a systematic review. Prostate Cancer Prostatic Dis. 2024;27:183–91.
Riviere P, Luterstein E, Kumar A, Vitzthum LK, Deka R, Sarkar RR, et al. Survival of African American and non‐Hispanic white men with prostate cancer in an equal‐access health care system. Cancer. 2020;126:1683–90.
Dess RT, Hartman HE, Mahal BA, Soni PD, Jackson WC, Cooperberg MR, et al. Association of Black Race With Prostate Cancer–Specific and Other-Cause Mortality. JAMA Oncol. 2019;5:975.
Crumley D, Lloyd J, Pucciarello M, Stapelfeld B. Addressing Social Determinants of Health via Medicaid Managed Care Contracts and Section 1115 Demonstrations. December 2018 – Prepared by the Center for Health Care Strategies. 1–48
Author information
Authors and Affiliations
Contributions
Conception and design: Autorino, Franco; Acquisition of data: Franco, Orsini, Bignante, Lasorsa; Statistical analysis: Mossack, Roadman; Interpretation of the data: Sturgis, Bignante, Roadman, Coogan, Cherullo; Drafting of the manuscript: Mossack; Critical revision of the manuscript for important intellectual content: Franco, De Nunzio, Autorino; Supervision: Autorino; Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: Mossack, Sturgis, Orsini, Lasorsa, De Nunzio, Coogan, Autorino; All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
As a secondary analysis of deidentified data, the study was granted exempt status from institutional board review.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mossack, S.M., Franco, A., Roadman, D.F. et al. Social determinants of health and surgical outcomes of minimally invasive radical prostatectomy: a national population-based study. Prostate Cancer Prostatic Dis 28, 767–772 (2025). https://doi.org/10.1038/s41391-024-00913-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41391-024-00913-0
This article is cited by
-
Best of 2024 in Prostate Cancer and Prostatic diseases
Prostate Cancer and Prostatic Diseases (2025)
-
From association to action: strengthening research on social determinants of health
Prostate Cancer and Prostatic Diseases (2025)
-
MISTs for benign prostatic hyperplasia as first line interventional treatment: Alea iacta est?
Prostate Cancer and Prostatic Diseases (2025)
-
Impact of Social Determinants of Health on Post-operative Outcomes Following Robotic Radical Prostatectomy
Current Oncology Reports (2025)