Abstract
Background
For men with low-risk prostate cancer (PCa) on active surveillance (AS), there remain limited and conflicting data regarding whether physical activity may influence disease progression evidenced by grade reclassification (GR). Furthermore, it is unclear whether physical activity affects the risk independently of other lifestyle factors such as diet and smoking.
Methods
This is a prospective cohort study of men diagnosed with Grade Group (GG) 1 PCa undergoing AS. Patients completed diet and physical activity questionnaires upon AS enrollment. Physical activity level was evaluated as metabolic equivalent of task hours per week (MET-h/wk), and diet quality as energy-adjusted Healthy Eating Index (E-HEI) score. Multivariable competing risk regressions were utilized to examine the association of baseline physical activity level with GR to ≥GG2 and to ≥GG3, adjusting for established clinicopathological risk factors, diet quality, and smoking history.
Results
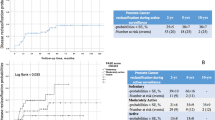
We included 828 men with a median follow up of 6.4 years (quartiles: 4.0–9.1). In multivariable regression models adjusted for covariates, increased baseline physical activity levels (3 to <9 MET-h/wk versus <3: subdistribution hazard ratio [SHR] 0.18, 95% confidence interval [CI] 0.05–0.61; 9 to <18 MET-h/wk versus <3: SHR 0.26, 95% CI 0.10–0.68; ≥18 MET-h/wk versus <3: SHR 0.31, 95% CI 0.12–0.80) were associated with significantly decreased risks of GR to ≥GG3. Increased physical activity levels were associated with non-significant decreases in GR to ≥GG2. An increased E-HEI score was also significantly associated with decreased GR to ≥GG3, and non-significant reduction in GR to ≥GG2. Smoking history was not associated with either GR outcome.
Conclusions
In a large prospective cohort with longitudinal follow-up of men pursuing AS for GG1 PCa, increased baseline physical activity levels, compared to a sedentary lifestyle defined as <3 MET-h/wk, was independently associated with a lower risk of progression to ≥GG3 disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request. The data are not publicly available due to institutional policies and the need to protect participant privacy.
References
Su ZT, Mamawala M, Landis PK, De La Calle CM, Shivappa N, Wirth M, et al. Diet quality, dietary inflammatory potential, and risk of prostate cancer grade reclassification. JAMA Oncol. 2024;10:1702.
Ungvari Z, Fekete M, Varga P, Munkácsy G, Fekete JT, Lehoczki A, et al. Exercise and survival benefit in cancer patients: evidence from a comprehensive meta-analysis. GeroScience [Internet]. 2025 [cited 2025 May 6]; Available from: https://link.springer.com/10.1007/s11357-025-01647-0
Azar AM Physical Activity Guidelines for Americans. 2nd edition. US Dep Health Hum Serv; 2018.
Patel AV, Friedenreich CM, Moore SC, Hayes SC, Silver JK, Campbell KL, et al. American college of sports medicine roundtable report on physical activity, sedentary behavior, and cancer prevention and control. Med Sci Sports Exerc. 2019;51:2391–402.
Kang DW, Fairey AS, Boulé NG, Field CJ, Wharton SA, Courneya KS. Effects of exercise on cardiorespiratory fitness and biochemical progression in men with localized prostate cancer under active surveillance: the ERASE randomized clinical trial. JAMA Oncol. 2021;7:1487.
Guy DE, Vandersluis A, Klotz LH, Fleshner N, Kiss A, Parker C, et al. Total energy expenditure and vigorous-intensity physical activity are associated with reduced odds of reclassification among men on active surveillance. Prostate Cancer Prostatic Dis. 2018;21:187–95.
Papadopoulos E, Alibhai SMH, Tomlinson GA, Matthew AG, Nesbitt M, Finelli A, et al. Influence of physical activity on active surveillance discontinuation in men with low-risk prostate cancer. Cancer Causes Control. 2019;30:1009–12.
Brassetti A, Ferriero M, Napodano G, Sanseverino R, Badenchini F, Tuderti G, et al. Physical activity decreases the risk of cancer reclassification in patients on active surveillance: a multicenter retrospective study. Prostate Cancer Prostatic Dis. 2021;24:1151–7.
Tosoian JJ, Mamawala M, Epstein JI, Landis P, Macura KJ, Simopoulos DN, et al. Active surveillance of grade group 1 prostate cancer: long-term outcomes from a large prospective cohort. Eur Urol. 2020;77:675–82.
Basiotis P, Carlson A, Gerrior S, Juan W, Lino M. The Healthy Eating Index: 1999-2000 [Internet]. US Dept of Agriculture, Center for Nutrition Policy and Promotion; [cited 2025 Jan 31]. Available from: https://fns-prod.azureedge.us/sites/default/files/healthy_eating_index/HEI99-00report.pdf
Boucher B, Cotterchio M, Kreiger N, Nadalin V, Block T, Block G. Validity and reliability of the Block98 food-frequency questionnaire in a sample of Canadian women. Public Health Nutr. 2006;9:84–93.
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–516.
Jetté M, Sidney K, Blümchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol. 1990;13:555–65.
Willett W, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Johns Hopkins Univ Sch Hyg Public Health. 1986;124:17–27.
Antonelli JA, Jones LW, Bañez LL, Thomas JA, Anderson K, Taylor LA, et al. Exercise and prostate cancer risk in a cohort of veterans undergoing prostate needle biopsy. J Urol. 2009;182:2226–31.
Giovannucci EL, Liu Y, Leitzmann MF, Stampfer MJ, Willett WC. A prospective study of physical activity and incident and fatal prostate cancer. Arch Intern Med. 2005;165:1005–10.
Kraus WE, Powell KE, Haskell WL, Janz KF, Campbell WW, Jakicic JM, et al. Physical activity, all-cause and cardiovascular mortality, and cardiovascular disease. Med Sci Sports Exerc. 2019;51:1270–81.
How to Measure Physical Activity Intensity [Internet]. U.S. Centers for Disease Control and Prevention; 2023 [cited 2025 Aug 11]. Available from: https://www.cdc.gov/physical-activity-basics/measuring/index.html
Ding D, Nguyen B, Nau T, Luo M, Del Pozo Cruz B, Dempsey PC, et al. Daily steps and health outcomes in adults: a systematic review and dose-response meta-analysis. Lancet Public Health. 2025;10:e668–81.
Richman EL, Kenfield SA, Stampfer MJ, Paciorek A, Carroll PR, Chan JM. Physical activity after diagnosis and risk of prostate cancer progression: data from the cancer of the prostate strategic urologic research endeavor. Cancer Res. 2011;71:3889–95.
Kenfield SA, Stampfer MJ, Giovannucci E, Chan JM. Physical activity and survival after prostate cancer diagnosis in the health professionals follow-up study. J Clin Oncol. 2011;29:726–32.
Wang Y, Jacobs EJ, Gapstur SM, Maliniak ML, Gansler T, McCullough ML, et al. Recreational physical activity in relation to prostate cancer-specific mortality among men with nonmetastatic prostate cancer. Eur Urol. 2017;72:931–9.
Moon C, Gallegos AM, Sheikh B, Kumar P, Liss M, Patel DI. Pilot study on the impact of a home-based exercise program on inflammatory cytokines and quality of life in men with prostate cancer under active surveillance. Cancer Control. 2022;29:10732748221130964.
Ornish D, Magbanua MJM, Weidner G, Weinberg V, Kemp C, Green C, et al. Changes in prostate gene expression in men undergoing an intensive nutrition and lifestyle intervention. Proc Natl Acad Sci. 2008;105:8369–74.
Wright JL, Schenk JM, Gulati R, Beatty SJ, VanDoren M, Lin DW, et al. The prostate cancer active lifestyle study (PALS): a randomized controlled trial of diet and exercise in overweight and obese men on active surveillance. Cancer. 2024;130:2108–19.
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. 2018;320:2020.
Eckel RH, Jakicic JM, Ard JD, De Jesus JM, Houston Miller N, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk. J Am Coll Cardiol. 2014;63:2960–84.
Acknowledgements
We thank constructive comments and helpful suggestions from anonymous reviewers for Prostate Cancer and Prostatic Diseases, which significantly improved the design and interpretations of our study.
Funding
This study was supported by the Patrick C. Walsh Prostate Cancer Research Fund (BJT) and Persky Scholarship (ZTS), a Johns Hopkins intramural scholarship.
Author information
Authors and Affiliations
Contributions
MIH and ZTS contributed equally to this work. MIH and ZTS conceived and designed the study, interpreted the data, and drafted the manuscript. MM and YJ performed the statistical analyses and contributed to data interpretation. PKL coordinated data collection and database management. MNA, AJG, and CARL contributed to data acquisition and critical revision of the manuscript. CPP contributed to study design, clinical interpretation, and manuscript revision. BJT supervised the study, contributed to study conception and design, provided statistical and methodological oversight, and critically revised the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
BJT reported receiving personal fees for consulting from Emmes Inc and Myriad Genetics and grants from MDxHealth outside the submitted work. No other disclosures to report.
Ethics approval and consent to participate
Institutional Review Board approval was obtained from the Johns Hopkins IRB (number NA_00045103). Informed consent was obtained from all participants at the time of active surveillance enrollment. The study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Higgins, M.I., Su, Z.T., Mamawala, M. et al. Physical activity at baseline and risk of prostate cancer grade reclassification on active surveillance: results from a prospective cohort study. Prostate Cancer Prostatic Dis (2026). https://doi.org/10.1038/s41391-026-01085-9
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41391-026-01085-9