Abstract
Study design
Level-, age-, and gender-matched controlled cross-sectional cohort study.
Objectives
To investigate alterations of spinal cord (SC) motion within cervical spondylotic myelopathy (CSM) across the cervical spinal segments and its relation to cerebrospinal fluid (CSF)-flow, anatomic conditions, and clinical parameters.
Setting
University Hospital Balgrist, Zurich, Switzerland.
Methods
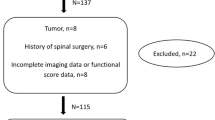
Overall, 12 patients suffering from CSM at level C5 and 12 controls underwent cardiac-gated 2D phase-contrast-MRI at level C2 and C5 and standard MRI sequences. Parameters of interest: Velocity measurements of SC and CSF (area under the curve = total displacement (normalization for duration of the heart cycle), total displacement ratio (C5/C2; intraindividual normalization for confounders)), spinal canal diameters, clinical motor- and sensory scores, and performance measures.
Results
Interrater reliability was excellent for SC motion at both levels and for CSF flow at C2, but not reliable for CSF flow at C5. Within controls, SC motion at C2 positively correlated with SC motion at C5 (p = 0.000); this correlation diminished in patients (p = 0.860). SC total displacement ratio was significantly increased in patients (p = 0.029) and correlated with clinical impairment (p = 0.017). Morphometric measures of the extent of stenosis were not related to SC motion or clinical symptoms.
Conclusion
The findings revealed physiological interactions of CSF flow and SC motion across the cervical spine in healthy controls while being diminished in CSM patients. Findings of focally increased SC motion at the level of stenosis were related to clinical impairment and might be promising as a diagnostic and prognostic marker in CSM.
Sponsorship
CRPP Neurorehab of the University of Zurich, Switzerland.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Yamada A, Tsuchiya K, Bradley WG, Law M, Winkler ML, Borzage MR, et al. Current and emerging MR imaging techniques for the diagnosis ad management of CSF flow disorders: a review of phase-contrast and time-spatial labeling inversion pulse. Am J Neuroradiol. 2015;36:623–30.
Bradley WG, Haughton V, Mardal KA. Cerebrospinal fluid flow in adults. Hand Clin Neurol. 2016;135:591–601.
Vavasour IM, Meyers SM, MacMillan EL, Mädler B, Li DK, Rauscher A, et al. Increased spinal cord movements in cervical spondylotic myelopathy. Spine J. 2013;14:2344–54.
Shibuya R, Yonenobu K, Koizumi T, Kato Y, Mitta M, Yoshikawa H. Pulsatile cerebrospinal fluid flow measurement using phase-contrast magnetic resonance imaging in patients with cervical myelopathy. Spine. 2002;27:1087–93.
Chang HS, Nejo T, Yoshida S, Oya S, Matsui T. Increased flow signal in compressed segments of the spinal cord in patients with cervical spondylotoc myelopathy. Spine. 2014;39:2136–42.
Kalsi-Ryan S, Karadimas SK, Fehlings MG. Cervical spondylotic myelopathy: the clinical phenomenon and the current pathobiology of an increasingly prevalent and devastating disorder. Neuroscientist. 2013;19:409–21.
Schmid Daners M, Knoblich V, Soellinger M, Boesinger P, Seifert B, Guzzella L, et al. Age-specific characteristic and coupling of cerebral arterial inflow and cerebrospinal fluid dynamics. PLoS ONE. 2012;7:e37502.
Oner Z, Kahraman AS, Kose AO, Kavakli A, Cay M, Ozbag D. Quantitative evaluation of normal aqueductal cerebrospinal fluid flow using phase-contrast cine MRI according to age and sex. Anat Rec. 2017;300:549–55.
Dreha-Kulaczewski S, Joseph AA, Merboldt KD, Ludwig HC, Gärtner J, Frahm J. Identification of the upward movement of human cerebrospinal fluid in vivo and its relation to the brain venous system. J Neurosci. 2017;37:2395–402.
Yildiz S, Thyagaraj S, Jin N, Zhong X, Plavian SH, Marin BA, et al. Quantifying the influence of respiration and cardiac pulsations on cerebrospoinal fluid dynamics using real-time phase-contrast MRI. J Magn Reson Imaging. 2017;46:431–9.
Baron EM, Young WF. Cervical spondylotic myelopathy: a brief review of its pathophysiology, clinical course, and diagnosis. Neurosurgery. 2007;60:35–41.
Kato S, Shima A, Oka H, Chikuda H, Takeshida Y, Miyoshi K, et al. Comparison of the Japanese Orthopaedic Association (JOA) Score and Modified JOA (mJOA) Score for the assessment of cervical myelopathy: a multi-center observational study. PLoS ONE. 2015;10:e0123022. https://doi.org/10.1371/journal.pone.0123022.
Kirshblum SF, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M, et al. Reference for the 2011 revision of the International Standard for Neurological Classification of Spinal Cord Injury. J Spinal Cord Med. 2011;34:547–54.
Kalsi-Ryan S, Curt A, Verrier MC, Fehlings MG. Development of the graded redefined assessment of strength, sensibility and prehension (GRASSP): reviewing measurement specific to the upper limb in tetraplegia. J Neurosurg Spine. 2012;17:65–76.
Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC, et al. The spinal cord independence measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil. 2007;29:1926–33.
Witoszynskyj S, Rauscher A, Reichenbach JR, Barth M. Phase unwrapping of MR images using Phi UN—a fast and robust region growing algorith. Med Image Anal. 2009;13:257–68.
Haughton V, Mardal KA. Spinal fluid biomechanics and imaging: an update for neuropradiologists. Am J Neuroradiol. 2014;35:1864–9.
Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing intra rater reliability. Psych Bull. 1979;86:420–38.
Shin JJ, Jin BH, Kim KS, Cho YE, Xho WH. Intramedullary high signal intensity and neurological status as prognostic factors in cervical spondylotic myelopathy. Acta Neurochir. 2010;152:1678–94.
Bunck AC, Kroger JP, Juttner A, Brentrup A, Fiedler B, Schaarschmidt F, et al. Magnetic resonance 4D flow characteristics of cerebrospinal fluid at the craniocervical junction and the cervical spinal canal. Eur Radiol. 2011;21:1788–1796. 29
Yamada S, Kelly E. Cerebrospinal fluid dynamics and the pathophysiology of hydrocephalus: new concepts. Semin Ultrasound CT MR. 2016;37:84–91.
Feinberg DA, Mark AS. Human brain motion and cerebrospinal fluid circulation demonstrated with MR velocity imaging. Radiology. 1987;163:793–9.
Enzmann DR, Pelc NJ. Brain motion: measurement with phase-contrast MR imaging. Radiology. 1992;185:653–60.
Matsuzaki H, Wakabayashi K, Ishihara K, Ishikawa H, Kawabata H, Onomura T. The origin and significance of spinal cord pulsation. Spinal Cord. 1996;34:422–8.
Tanaka H, Sakurai K, Kashiwagi N, Fujita N, Hirabuki N, INaba F, et al. Transition of the craniocaudal velocity of the spinal cord: from cervical segment to lumbar enlargement. Invest Radiol. 1998;33:141–5.
Winklhofer S, Schroth F, Stolzmann P, Krings T, Mull M, Wiesmann M, et al. Spinal cord motion: influence of respiration and cardiac cycle. Rofo. 2014;136:1016–21.
Schaller B, Graf R. Different compartments of intracranial pressure and its relationship to cerebral blood flow. J Trauma. 2005;59:1521–31.
Greitz D, Wirestam R, Franck A, Nordell B, Thomsen C, Sthalberg F. Pulsatil brain movement and associated hydrondynamics studies by magnetix resonance phase imaging. The Monro-Kellie doctrine revisited. Neuroradiology. 1992;34:370–80.
Jokich PM, Rubin JM, Dohrmann GJ. Intraoperative ultrasonic evaluation of spinal cord motion. J Neurosurg. 1984;60:707–11.
Uftring SJ, Chu D, Alperin N, Levin DN. The mechanical state of intracranial tissues in elderly subjects studied by imaging CSF and brain pulsation. Magn Reson Imaging. 2000;18:991–6.
Acknowledgements
We would like to thank PD Dr. Martin Schubert and the staff of the Neurophysiology Lab, Spinal Cord Injury Center, Balgrist University Hospital Zürich, Switzerland and Alexandra Naef and Barbara Wagner, Department of Radiology, University Hospital Balgrist, Zürich, Switzerland.
Funding
The study was supported by the CRPP Neurorehab of the University of Zurich, Switzerland. The study was approved by the ethics committee of the University of Zurich, KEK-ZH 2012-0343; written informed consent off all participants for publication was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MK is employed by Siemens Healthcare AG, Zürich, Switzerland. The remaining authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Wolf, K., Hupp, M., Friedl, S. et al. In cervical spondylotic myelopathy spinal cord motion is focally increased at the level of stenosis: a controlled cross-sectional study. Spinal Cord 56, 769–776 (2018). https://doi.org/10.1038/s41393-018-0075-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-018-0075-1
This article is cited by
-
T2-weighted MRI high signal in cervical spondylotic myelopathy is associated with dynamic change
Journal of Orthopaedic Surgery and Research (2025)
-
Finite element modeling and analysis of effect of preexisting cervical degenerative disease on the spinal cord during flexion and extension
Medical & Biological Engineering & Computing (2024)
-
Degenerative cervical myelopathy — update and future directions
Nature Reviews Neurology (2020)
-
Segmental differences of cervical spinal cord motion: advancing from confounders to a diagnostic tool
Scientific Reports (2019)