Abstract
Study design
A prospective observational study.
Objectives
To determine the incidence of deep venous thrombosis (DVT) and to evaluate the risk factors for DVT development associated with degenerative cervical spine disease.
Setting
Hokkaido Spinal Cord Injury Center, Japan.
Methods
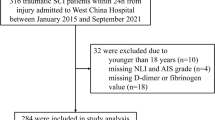
Between April 2008 and March 2015, patients with degenerative cervical spine disease, such as compressive myelopathy or radiculopathy, who underwent surgical treatment were prospectively assessed. Leg vein ultrasonography and D-dimer tests were performed preoperatively and at 4 days after surgery. All patients received treatment with intermittent pneumatic compression and elastic stockings for primary DVT prophylaxis. No anticoagulation medications were used for DVT prophylaxis.
Results
A total of 289 patients (203 males, 86 females; median age: 67 years (interquartile range, 58–76)) were included. Nine patients (3.1%) exhibited DVT during the perioperative period. All 9 cases were women who had distal DVT. The incidences of preoperative and postoperative DVT were 1.1% and 2.1%, respectively. The univariate analysis showed that statistically significant risk factors for perioperative DVT included female gender (P < 0.01), advanced age (P = 0.04), a low Japanese Orthopaedic Association score (P = 0.03), rapidly progressive myelopathy (P < 0.01), and inability to walk (P = 0.01). The multivariate analysis showed that rapidly progressive myelopathy (P = 0.04) was the most important risk factor.
Conclusion
Female gender and rapidly progressive myelopathy are high-risk factors that predict the development of DVT during the perioperative period of cervical spine surgery. This result indicates that screening and treatment for DVT are needed in such high-risk patients.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Freedman KB, Brookenthal KR, Fitzgerald RH Jr, Williams S, Lonner JH. A meta-analysis of thromboembolic prophylaxis following elective total hip arthroplasty. J Bone Jt Surg Am. 2000;82-A:929–38.
Zhou X, Qian W, Li J, Zhang P, Yang Z, Chen W, et al. Who are at risk for thromboembolism after arthroplasty? A systematic review and meta-analysis. Thromb Res. 2013;132:531–6.
Matsumoto S, Suda K, Iimoto S, Yasui K, Komatsu M, Ushiku C, et al. Prospective study of deep vein thrombosis in patients with spinal cord injury not receiving anticoagulant therapy. Spinal Cord. 2015;53:306–9.
Hamidi S, Riazi M. Cutoff values of plasma d-dimer level in patients with diagnosis of the venous thromboembolism after elective spinal surgery. Asian Spine J. 2015;9:232–8.
Glotzbecker MP, Bono CM, Wood KB, Harris MB. Thromboembolic disease in spinal surgery: a systematic review. Spine. 2009;34:291–303.
Yoshioka K, Murakami H, Demura S, Kato S, Tsuchiya H. Prevalence and risk factors for development of venous thromboembolism after degenerative spinal surgery. Spine. 2015;40:E301–6.
Oglesby M, Fineberg SJ, Patel AA, Pelton MA, Singh K. The incidence and mortality of thromboembolic events in cervical spine surgery. Spine. 2013;38:E521–7.
Akeda K, Matsunaga H, Imanishi T, Hasegawa M, Sakakibara T, Kasai Y, et al. Prevalence and countermeasures for venous thromboembolic diseases associated with spinal surgery: a follow-up study of an institutional protocol in 209 patients. Spine. 2014;39:791–7.
Sikorski JM, Hampson WG, Staddon GE. The natural history and aetiology of deep vein thrombosis after total hip replacement. J Bone Jt Surg Br. 1981;63-B:171–7.
Yamaguchi T, Hasegawa M, Niimi R, Sudo A. Incidence and time course of asymptomatic deep vein thrombosis with fondaparinux in patients undergoing total joint arthroplasty. Thromb Res. 2010;126:e323–6.
Masaki Y, Yamazaki M, Okawa A, Aramomi M, Hashimoto M, Koda M, et al. An analysis of factors causing poor surgical outcome in patients with cervical myelopathy due to ossification of the posterior longitudinal ligament: anterior decompression with spinal fusion versus laminoplasty. J Spinal Disord Tech. 2007;20:7–13.
Maynard FM Jr, Bracken MB, Creasey G, Ditunno JF Jr, Donovan WH, Ducker TB, et al. International standards for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Spinal Cord. 1997;3:266–74.
Sakuma T, Yamazaki M, Okawa A, Takahashi H, Kato K, Hashimoto M, et al. Neuroprotective therapy using granulocyte colony-stimulating factor for patients with worsening symptoms of compression myelopathy, Part 1: a phase I and IIa clinical trial. Eur Spine J. 2012;21:482–9.
Oda T, Fuji T, Kato Y, Fujita S, Kanemitsu N. Deep venous thrombosis after posterior spinal surgery. Spine. 2000;25:2962–7.
Furlan JC, Fehlings MG. Cardiovascular complications after acute spinal cord injury: pathophysiology, diagnosis, and management. Neurosurg Focus. 2008;25:E13.
Schoenfeld AJ, Herzog JP, Dunn JC, Bader JO, Belmont PJ Jr. Patient-based and surgical characteristics associated with the acute development of deep venous thrombosis and pulmonary embolism after spine surgery. Spine. 2013;38:1892–8.
Tominaga H, Setoguchi T, Tanabe F, Kawamura I, Tsuneyoshi Y, Kawabata N, et al. Risk factors for venous thromboembolism after spine surgery. Medicine (Baltimore). 2015;94:e466.
Takahashi H, Yokoyama Y, Iida Y, Terashima F, Hasegawa K, Saito T, et al. Incidence of venous thromboembolism after spine surgery. J Orthop Sci. 2012;17:114–7.
Yoshiiwa T, Miyazaki M, Takita C, Itonaga I, Tsumura H. Analysis of measured D-dimer levels for detection of deep venous thrombosis and pulmonary embolism after spinal surgery. J Spinal Disord Tech. 2011;24:E35–9.
Yoshioka K, Kitajima I, Kabata T, Tani M, Kawahara N, Murakami H, et al. Venous thromboembolism after spine surgery: changes of the fibrin monomer complex and D-dimer level during the perioperative period. J Neurosurg Spine. 2010;13:594–9.
Yeo DX, Junnarkar S, Balasubramaniam S, Tan YP, Low JK, Woon W, et al. Incidence of venous thromboembolism and its pharmacological prophylaxis in Asian general surgery patients: a systematic review. World J Surg. 2015;39:150–7.
Bin Abd Razak HR, Binte Abd Razak NF, Tan HA. Prevalence of venous thromboembolic events is low in Asians after total knee arthroplasty without chemoprophylaxis. J Arthroplasty. 2017;32:974–9.
Kanchanabat B, Stapanavatr W, Meknavin S, Soorapanth C, Sumanasrethakul C, Kanchanasuttirak P. Systematic review and meta-analysis on the rate of postoperative venous thromboembolism in orthopaedic surgery in Asian patients without thromboprophylaxis. Br J Surg. 2011;98:1356–64.
JCS Joint Working Group. Guidelines for the diagnosis, treatment and prevention of pulmonary thromboembolism and deep vein thrombosis (JCS 2009). Circ J. 2011;75:1258–81.
Shiota N, Sato T, Nishida K, Matsuo M, Takahara Y, Mitani S, et al. Changes in LPIA D-dimer levels after total hip or knee arthroplasty relevant to deep-vein thrombosis diagnosed by bilateral ascending venography. J Orthop Sci. 2002;7:444–50.
Raimondi P, Bongard O, de Moerloose P, Reber G, Waldvogel F, Bounameaux H. D-dimer plasma concentration in various clinical conditions: implication for the use of this test in the diagnostic approach of venous thromboembolism. Thromb Res. 1993;69:125–30.
Author contributions
Conception and design of the study: KS. Analysis and interpretation of data: KY and KS. Collection and assembly of data: KY, KS, SMH, MK, and CU. Drafting of the article: KY. Resource: KS and MK. Supervision: MT, AM, and NI. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Yamada, K., Suda, K., Matsumoto Harmon, S. et al. Rapidly progressive cervical myelopathy had a high risk of developing deep venous thrombosis: a prospective observational study in 289 cases with degenerative cervical spine disease. Spinal Cord 57, 58–64 (2019). https://doi.org/10.1038/s41393-018-0213-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-018-0213-9
This article is cited by
-
Association between age and incidence of deep vein thrombosis in patients with spinal cord injury: an observational cross-sectional study
Spinal Cord (2022)
-
Risk factors of postoperative deep vein thrombosis (DVT) under low molecular weight heparin (LMWH) prophylaxis in patients with thoracolumbar fractures caused by high-energy injuries
Journal of Thrombosis and Thrombolysis (2021)