Abstract
Study design
The Neurogenic Bladder Research Group (NBRG) registry is a multicenter prospective observational study. This manuscript is retrospective based on a cross-sectional survey.
Objectives
To assess patient subjective assessment of urinary tract infection (UTI) frequency and severity are associated with the degree of use of catheters or incontinence products.
Setting
Multiple hospitals across the United States.
Methods
Eligibility included: age > 18 years and acquired SCI. Over 1.5 years, 1479 eligible participants were enrolled. We excluded those with surgical reconstruction or diversion of the bladder. In total, 1282 participants were grouped by bladder management: (1) indwelling catheter (IDC), (2) clean intermittent catheterization (CIC), (3) external devices (pads/condom), and (4) volitional voiding (Void). UTI frequency was classified as 0, 1–3, 4–6, or > 6 over the prior year. UTI severity was determined by hospitalization for UTI in the prior year. Multivariate regression compared these factors across groups.
Results
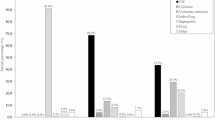
UTIs were least frequent in Void followed by pads/condom, CIC, and IDC (all p ≤ 0.001). UTI severity followed a similar pattern. Controlling for covariates, the adjusted odds of UTI frequency (Void = reference) were 2.28 (1.38–3.76) for pads/condom, 3.42 (2.25–5.18) for CIC, and 4.3 (2.59–6.70) for IDC (all p ≤ 0.001).
Conclusions
Patient subjective assessment of UTI frequency is highest with IDC, followed by CIC, pads/condom, and lowest with spontaneous voiding. The odds of hospitalization for UTI were three times higher for IDC than spontaneous voiding. UTI risk should be considered when counseling patients about bladder management options. These associations do not imply causation but warrant further investigation in a prospective manner.
Sponsorship
Patient-Centered Outcomes Research Institute (PCORI) Award (CER14092138).
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data archiving
The data sets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Spinal Cord Injury (SCI). 2016 facts and figures at a glance. J Spinal Cord Med. 2016;39:493–4.
Ge L, Arul K, Ikpeze T, Baldwin A, Nickels JL, Mesfin A. Demographics and clinical characteristics of traumatic and non-traumatic spinal cord injuries. World Neurosurg. 2017. https://doi.org/10.1016/j.wneu.2017.12.008.
Strauss DJ, DeVivo MJ, Paculdo DR, Shavelle RM. Trends in life expectancy after spinal cord injury. Arch Phys Med Rehabil. 2006;87:1079–85.
Rabadi MH, Mayanna SK, Vincent AS. Predictors of mortality in veterans with traumatic spinal cord injury. Spinal Cord. 2013;51:784–8.
Frankel HL, Coll JR, Charlifue SW, Whiteneck GG, Gardner BP, Jamous MA, et al. Long-term survival in spinal cord injury: a fifty year investigation. Spinal Cord. 1998;36:266–74.
Skelton F, Hoffman JM, Reyes M, Burns SP. Examining health-care utilization in the first year following spinal cord injury. J Spinal Cord Med. 2015;38:690–5.
Craven C, Hitzig SL, Mittmann N. Impact of impairment and secondary health conditions on health preference among Canadians with chronic spinal cord injury. J Spinal Cord Med. 2012;35:361–70.
Zlatev DV, Shem K, Elliott CS. Predictors of long-term bladder management in spinal cord injury patients-Upper extremity function may matter most. Neurourol Urodyn. 2017;36:170.
Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:625–63.
Cameron AP, Wallner LP, Forchheimer MB, Clemens JQ, Dunn RL, Rodriguez G, et al. Medical and psychosocial complications associated with method of bladder management after traumatic spinal cord injury. Arch Phys Med Rehabil. 2011;92:449–56.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Esclarín De Ruz A, García Leoni E, Herruzo Cabrera R. Epidemiology and risk factors for urinary tract infection in patients with spinal cord injury. J Urol. 2000;164:1285–9.
Erickson RP, Merritt JL, Opitz JL, Ilstrup DM. Bacteriuria during follow-up in patients with spinal cord injury: I. Rates of bacteriuria in various bladder-emptying methods. Arch Phys Med Rehabil. 1982;63:409–12.
Singh R, Rohilla RK, Sangwan K, Siwach R, Magu NK, Sangwan SS. Bladder management methods and urological complications in spinal cord injury patients. Indian J Orthop. 2011;45:141–7.
Biering-Sørensen F, Bagi P, Høiby N. Urinary tract infections in patients with spinal cord lesions: treatment and prevention. Drugs. 2001;61:1275–87.
Biering-Sørensen F. Urinary tract infection in individuals with spinal cord lesion. Curr Opin Urol. 2002;12:45–49.
Siroky MB. Pathogenesis of bacteriuria and infection in the spinal cord injured patient. Am J Med. 2002;113:67S–79S.
Trautner BW, Darouiche RO. Prevention of urinary tract infection in patients with spinal cord injury. J Spinal Cord Med. 2002;25:277–83.
García Leoni ME, Esclarín De, Ruz A. Management of urinary tract infection in patients with spinal cord injuries. Clin Microbiol Infect. 2003;9:780–5.
D’Hondt F, Everaert K. Urinary tract infections in patients with spinal cord injuries. Curr Infect Dis Rep. 2011;13:544–51.
Skelton F, Grigoryan L, Holmes SA, Poon IO, Trautner B. Routine urine testing at 436 the spinal cord injury annual evaluation leads to unnecessary antibiotic use: a 437 pilot study and future directions. Arch Phys Med Rehabil. 2018;99:219–25.
Weld KJ, Graney MJ, Dmochowski RR. Differences in bladder compliance with time and associations of bladder management with compliance in spinal cord injured patients. J Urol. 2000;163:1228–33.
Vasudeva P, Madersbacher H. Factors implicated in pathogenesis of urinary tract infections in neurogenic bladders: some revered, few forgotten, others ignored. Neurourol Urodyn. 2013;33:95–100.
Cameron AP, Wallner LP, Tate DG, Sarma AV, Rodriguez GM, Clemens JQ. Bladder management after spinal cord injury in the United States 1972 to 2005. J Urol. 2010;184:213–7.
Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Dis Mon. 2003;49:53–70.
Unsal-Delialioglu S, Kaya K, Sahin-Onat S, Kulakli F, Culha C, Ozel S. Fever during rehabilitation in patients with traumatic spinal cord injury: analysis of 392 cases from a national rehabilitation hospital in Turkey. J Spinal Cord Med. 2010;33:243–8.
Failli V, Kopp MA, Gericke C, Martus P, Klingbeil S, Brommer B, et al. Functional neurological recovery after spinal cord injury is impaired in patients with infections. Brain. 2012;135:3238–50.
Consortium for Spinal Cord Medicine. Bladder management for adults with spinal cord injury: a clinical practice guideline for health-care providers. J Spinal Cord Med. 2006;29:527–73.
Urologic Management of the Spinal Cord Injured Patient. 2016.
Ronco E, Denys P, Bernède-Bauduin C, Laffont I, Martel P, Salomon J, et al. Diagnostic criteria of urinary tract infection in male patients with spinal cord injury. Neurorehabil Neural Repair. 2011;25:351–8.
Massa LM, Hoffman JM, Cardenas DD. Validity, accuracy, and predictive value of urinary tract infection signs and symptoms in individuals with spinal cord injury on intermittent catheterization. J Spinal Cord Med. 2009;32:568–73.
Foxman B, Barlow R, D’Arcy H, Gillespie B, Sobel JD. Urinary tract infection: self-reported incidence and associated costs. Ann Epidemiol. 2000;10:509–15.
The prevention and management of urinary tract infections among people with spinal cord injuries. National Institute on Disability and Rehabilitation Research Consensus Statement. January 27-29, 1992. J Am Paraplegia Soc. 1992;15:194–204.
Author information
Authors and Affiliations
Contributions
JDR was responsible for the interpretation of results and manuscript writing. JJP was responsible for data analysis and manuscript revision. JTS, SML, JBM, BW and SPE aided in study design, acquired data, and revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of ethics
I/we certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers/animals were followed during the course of this research.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roth, J.D., Pariser, J.J., Stoffel, J.T. et al. Patient subjective assessment of urinary tract infection frequency and severity is associated with bladder management method in spinal cord injury. Spinal Cord 57, 700–707 (2019). https://doi.org/10.1038/s41393-019-0268-2
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41393-019-0268-2
This article is cited by
-
Scoping review on managing the bladder and preventing urinary tract infections (UTIs) in athletes with spinal cord injuries
Bulletin of Faculty of Physical Therapy (2024)
-
Indwelling catheter vs intermittent catheterization: is there a difference in UTI susceptibility?
BMC Infectious Diseases (2023)
-
Cross-sectional internet survey exploring symptomatic urinary tract infection by type of urinary catheter in persons with spinal cord lesion in Japan
Spinal Cord Series and Cases (2023)
-
Frequency of patient-reported UTIs is associated with poor quality of life after spinal cord injury: a prospective observational study
Spinal Cord (2020)