Abstract
Study design
A prospective single arm study.
Objectives
Previously we have demonstrated that magnetic resonance (MR) defecography is feasible in participants with complete spinal cord injury (SCI). The main aim of this study is to evaluate whether MR defecography can provide objective parameters correlating with the clinical manifestations of neurogenic bowel dysfunction (NBD) in participants with SCI.
Setting
A monocentric study in a comprehensive care university hospital Spinal Cord Injury Center.
Methods
Previously published MR defecography parameters (anorectal angle (ARA), hiatal descent (M-line) and hiatal width (H-line)) of twenty participants with SCI were now compared to a standardized clinical assessment of NBD. Descriptive statistics, correlations and t-tests for independent samples were calculated.
Results
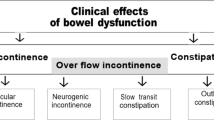
The significantly higher values for the ARA at rest and M-line at rest in participants with SCI correlated with the clinical assessment of bowel incontinence. Furthermore, in nearly half of the investigated SCI cohort the normally positive difference between ARA, M-line and H-line at rest and during defecation became negative suggesting pelvic floor dyssynergia as a potential mechanism underlying constipation in people with complete SCI. In fact, these participants showed a more severe clinical presentation of NBD according to the total NBD score.
Conclusions
MR defecography provides objective parameters correlating with clinical signs of NBD, such as constipation and bowel incontinence. Therefore, MR defecography can support pathophysiology-based decision-making with respect to specific therapeutic interventions, which should help to improve the management of NBD.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Faaborg PM, Christensen P, Finnerup N, Laurberg S, Krogh K. The pattern of colorectal dysfunction changes with time since spinal cord injury. Spinal Cord. 2008;46:234–8.
Kirk PM, King RB, Temple R, Bourjaily J, Thomas P. Long-term follow-up of bowel management after spinal cord injury. SCI Nurs. 1997;14:56–63.
Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004;21:1371–83.
Chung EA, Emmanuel AV. Gastrointestinal symptoms related to autonomic dysfunction following spinal cord injury. Prog Brain Res. 2006;152:317–33.
Valles M, Vidal J, Clave P, Mearin F. Bowel dysfunction in patients with motor complete spinal cord injury: clinical, neurological, and pathophysiological associations. Am J Gastroenterol. 2006;101:2290–9.
Krassioukov A, Eng JJ, Claxton G, Sakakibara BM, Shum S. Neurogenic bowel management after spinal cord injury: a systematic review of the evidence. Spinal Cord. 2010;48:718–33.
Spinal Cord Medicine Consortium. Clinical practice guidelines: neurogenic bowel management in adults with spinal cord injury. J Spinal Cord Med. 1998;21:248–93.
Harari D, Minaker KL. Megacolon in patients with chronic spinal cord injury. Spinal Cord. 2000;38:331–9.
Harari D, Sarkarati M, Gurwitz JH, McGlinchey-Berroth G, Minaker KL. Constipation-related symptoms and bowel program concerning individuals with spinal cord injury. Spinal Cord. 1997;35:394–401.
Furlan JC, Urbach DR, Fehlings MG. Optimal treatment for severe neurogenic bowel dysfunction after chronic spinal cord injury: a decision analysis. Br J Surg. 2007;94:1139–50.
Nielsen SD, Faaborg PM, Finnerup NB, Christensen P, Krogh K. Ageing with neurogenic bowel dysfunction. Spinal Cord. 2017;55:769–73.
Stone JM, Nino-Murcia M, Wolfe VA, Perkash I. Chronic gastrointestinal problems in spinal cord injury patients: a prospective analysis. Am J Gastroenterol. 1990;85:1114–9.
Liu CW, Huang CC, Chen CH, Yang YH, Chen TW, Huang MH. Prediction of severe neurogenic bowel dysfunction in persons with spinal cord injury. Spinal Cord. 2010;48:554–9.
Lynch AC, Antony A, Dobbs BR, Frizelle FA. Bowel dysfunction following spinal cord injury. Spinal Cord. 2001;39:193–203.
Lynch AC, Wong C, Anthony A, Dobbs BR, Frizelle FA. Bowel dysfunction following spinal cord injury: a description of bowel function in a spinal cord-injured population and comparison with age and gender matched controls. Spinal Cord. 2000;38:717–23.
Piloni V, Tosi P, Vernelli M. MR-defecography in obstructed defecation syndrome (ODS): technique, diagnostic criteria and grading. Tech Coloproctol. 2013;17:501–10.
Reiner CS, Tutuian R, Solopova AE, Pohl D, Marincek B, Weishaupt D. MR defecography in patients with dyssynergic defecation: spectrum of imaging findings and diagnostic value. Br J Radiol. 2011;84:136–44.
Bharucha AE, Wald A, Enck P, Rao S. Functional anorectal disorders. Gastroenterology. 2006;130:1510–8.
Putz C, Alt CD, Hensel C, Wagner B, Gantz S, Gerner HJ, et al. 3T MR-defecography-A feasibility study in sensorimotor complete spinal cord injured patients with neurogenic bowel dysfunction. Eur J Radiol. 2017;91:15–21.
Weishaupt, DR & Reiner, CS MR-Defäkographie aus Gastrointestinale MRT Theorie und Praxis, Herausgeber: M.G. Thomas C. Lauenstein. Wissenschaftsverlag (2009).
Schreyer AG, Paetzel C, Fürst A, Dendl LM, Hutzel E, Müller-Wille R, et al. Dynamic magnetic resonance defecography in 10 asymptomatic volunteers. World J Gastroenterol. 2012;18:6836–42.
Bharucha AE, Fletcher JG, Harper CM, Hough D, Daube JR, Stevens C, et al. Relationship between symptoms and disordered continence mechanisms in women with idiopathic faecal incontinence. Gut. 2005;54:546–55.
Comiter CV, Vasavada SP, Barbaric ZL, Gousse AE, Raz S. Grading pelvic prolapse and pelvic floor relaxation using dynamic magnetic resonance imaging. Urology. 1999;54:454–7.
Maynard FM Jr., Bracen MB, Creasey G, Ditunno JF Jr., Donovan WH, Ducker TB, et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord. 1997;35:266–74.
Krogh K, Christensen P, Sabroe S, Laurberg S. Neurogenic bowel dysfunction score. Spinal Cord. 2006;44:625–31.
Pannu HK, Kaufmann HS, Cundiff GW, Gendary R, Bluemke DA, Fishman EK. Dynamic MR imaging of pelvic organ prolapse: spectrum of abnormalities. Radiographics. 2000;20:1567–82.
Sprenger D, Lienemann A, Anthuber C, Reiser M. [Functional MRI of the pelvic floor: its normal anatomy and pathological findings]. Radiologe. 2000;40:451–7.
Kuijpers HC, Bleijenberg G. The spastic pelvic floor syndrome. A cause of constipation. Dis Colon Rectum. 1985;28:669–72.
Quint EH, Smith YR, Bowerman RA, DeLancey JO. Spasticity of the pelvic floor mimicking an obstructive anomaly. J Pediatr Adolesc Gynecol. 2003;16:83–85.
Altomare DF, Spazzafumo L, Rinaldi M, Dodi G, Ghiselli R, Piloni V. Set-up and statistical validation of a new scoring system for obstructed defaecation syndrome. Colorectal Dis. 2008;10:84–88.
Bitti GT, Argiolas GA, Ballicu N, Caddeo E, Cecconi M, Demurtas G, et al. Pelvic floor failure: MR imaging evaluation of anatomic and functional abnormalities. RadioGraphics. 2014;34:429–48.
Kamradt T, Rasch C, Schuld C, Böttinger M, Mürle B, Hensel C, et al. Spinal cord injury: association with axonal peripheral neuropathy in severely paralysed limbs. Eur J Neurol. 2013;20:843–8.
Hughes M. Bowel management in spinal cord injury patients. Clin Colon Rectal Surg. 2014;27:113–5.
Jost WH, Schrank B, Herold A, Leiss O. Functional outlet obstruction: anismus, spastic pelvic floor syndrome, and dyscoordination of the voluntary sphincter muscles. Definition, diagnosis, and treatment from the neurologic point of view. Scand J Gastroenterol. 1999;34:449–53.
Broens PM, Penninckx FM, Ochoa JB. Fecal continence revisited: the anal external sphincter continence reflex. Dis Colon Rectum. 2013;56:1273–81.
Morren GL, et al. Triphasic MRI of pelvic organ descent: sources of measurement error. Eur J Radiol. 2005;54:276–83.
Acknowledgements
The authors thank Radhika Puttagunta for proof reading the manuscript.
Funding
This study was financially supported by “Stiftung Orthopedic University Hospital Heidelberg”.
Author information
Authors and Affiliations
Contributions
Cornelia Putz, MD: Design, participant examinations, manuscript, analysis of data. Celine D Alt, MD: Evaluation of radiological parameters, correction of the manuscript. Bjoern Wagner, MD: Participant examinations, data acquisition. Simone Gantz: Statistic analysis. Hans J Gerner, MD: Design, correction of the manuscript. Nobert Weidner, MD: Analysis and interpretation of data, correction of the manuscript. Lars Grenacher, MD: Design, evaluation of radiological parameters, Cornelia Hensel, MD: Particpants examinations, analysis of data, manuscript.
Corresponding author
Ethics declarations
Statement of Ethics
The MR defecography study including the clinical evaluation (trial number S-274/2008) has been proofed by the ethics committee Heidelberg University Hospital, Germany. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Putz, C., Alt, C.D., Wagner, B. et al. MR defecography detects pelvic floor dysfunction in participants with chronic complete spinal cord injury. Spinal Cord 58, 203–210 (2020). https://doi.org/10.1038/s41393-019-0351-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-019-0351-8
This article is cited by
-
Role of MRI radiomics in deep learning-based prediction of intestinal diseases
International Journal of Colorectal Disease (2026)
-
The effects of virtual soccer game on balance, gait function, and kick speed in chronic incomplete spinal cord injury: a randomized controlled trial
Spinal Cord (2022)
-
The Role of MRI in the Diagnosis of Pelvic Floor Disorders
Current Urology Reports (2020)