Abstract
Study design
Cohort study.
Objectives
It is widely accepted that the prediction of long-term neurologic outcome after traumatic spinal cord injury (SCI) can be done more accurately with neurological examinations conducted days to weeks post injury. However, modern clinical trials of neuroprotective interventions often require patients be examined and enrolled within hours. Our objective was to determine whether variability in timing of neurological examinations within 48 h after SCI is associated with differences in observations of follow-up neurologic recovery.
Setting
Level I trauma hospital.
Methods
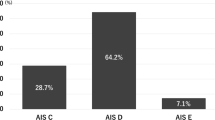
An observational analysis testing for differences in AIS conversion rates and changes in total motor scores by neurological examination timing, controlling for potential confounders with multivariate stepwise regression.
Results
We included 85 patients, whose mean times from injury to baseline and follow-up examinations were 11.8 h (SD 9.8) and 208.2 days (SD 75.2), respectively. AIS conversion by 1+ grade was significantly more likely in patients examined at ≤4 h in comparison with later examination (78% versus 47%, RR = 1.66, p = 0.04), even after controlling for timing of surgery, age, and sex (OR 5.0, 95% CI 1.1–10, p = 0.04). We failed to identify any statistically significant associations for total motor score recovery in unadjusted or adjusted analyses.
Conclusions
AIS grade conversion was significantly more likely in those examined ≤4 h of injury; the effect of timing on motor scores remains uncertain. Variability in neurological examination timing within hours after acute traumatic SCI may influence observations of long-term neurological recovery, which could introduce bias or lead to errors in interpretation of studies of therapeutic interventions.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The raw data analyzed in this study are not publicly available due to stipulations about their use with the participating hospital facility and the participants themselves, but an application for data access can be made to the Rick Hansen Institute’s Data Steward, via the corresponding author, and data may be available on reasonable request with permission from the participating hospital facility’s principal investigator.
Change history
09 January 2020
A Correction to this paper has been published: https://doi.org/10.1038/s41393-020-0413-y
References
Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D, et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord. 2007;45:190–205.
Grossman RG, Fehlings MG, Frankowski RF, Burau KD, Chow DSL, Tator C et al. A prospective, multicenter, phase I matched-comparison group trial of safety, pharmacokinetics, and preliminary efficacy of riluzole in patients with traumatic spinal cord injury. J Neurotrauma. 2014;31:239–55.
Casha S, Zygun D, McGowan MD, Bains I, Yong VW, John Hurlbert R. Results of a phase II placebo-controlled randomized trial of minocycline in acute spinal cord injury. Brain. 2012;135:1224–36.
Refinement P, Kwon BK, Roy J, Lee JHT, Okon E, Zhang H, et al. Magnesium chloride in a polyethylene glycol formulation as a neuroprotective therapy for acute spinal cord injury. J Neurotrauma. 2009;26:1379–93.
Evaniew N, Noonan VK, Fallah N, Kwon BK, Rivers CS, Ahn H, et al. Methylprednisolone for the treatment of patients with acute spinal cord injuries: a propensity score-matched cohort study from a Canadian multi-center spinal cord injury registry. J Neurotrauma. 2015;32:1674–83.
Dvorak MF, Noonan VK, Fallah N, Fisher CG, Rivers CS, Ahn H, et al. Minimizing errors in acute traumatic spinal cord injury trials by acknowledging the heterogeneity of spinal cord anatomy and injury severity: an observational Canadian cohort analysis. J Neurotrauma. 2014;31:1540–7.
Ahn H, Bailey CS, Rivers CS, Noonan VK, Tsai EC, Fourney DR, et al. Effect of older age on treatment decisions and outcomes among patients with traumatic spinal cord injury. CMAJ. 2015;187:873–80.
Dvorak MF, Noonan VK, Fallah N, Fisher CG, Finkelstein J, Kwon BK, et al. The influence of time from injury to surgery on motor recovery and length of hospital stay in acute traumatic spinal cord injury: an observational Canadian cohort study. J Neurotrauma. 2015;32:645–54.
Paquet J, Rivers CS, Kurban D, Finkelstein J, Tee JW, Noonan VK, et al. The impact of spine stability on cervical spinal cord injury with respect to demographics, management, and outcome: a prospective cohort from a national spinal cord injury registry. Spine J. 2018;18:88–98.
Holtz KA, Szefer E, Noonan VK, Kwon BK, Mills PB. Treatment patterns of in-patient spasticity medication use after traumatic spinal cord injury: a prospective cohort study. Spinal Cord. https://doi.org/10.1038/s41393-018-0165-0.
Noonan V, Kwon B, Soril L, Fehlings M, Hurlbert R, Townson A, et al. The Rick Hansen spinal cord injury registry (RHSCIR): a national patient-registry. Spinal Cord. 2012;50:22–27.
Kirshblum S, Waring W. Updates for the International standards for neurological classification of spinal cord injury. Phys Med Rehabil Clin N Am. 2014;25:505–17.
Furlan JC, Fehlings MG, Tator CH, Davis AM. Motor and sensory assessment of patients in clinical trials for pharmacological therapy of acute spinal cord injury: psychometric properties of the ASIA Standards. J Neurotrauma. 2008;25:1273–301.
Walden K, Bélanger LM, Biering-Sørensen F, Burns SP, Echeverria E, Kirshblum S, et al. Development and validation of a computerized algorithm for International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI). Spinal Cord. 2016;54:197–203.
Kirshblum SC, Burns SP, Biering-Sørensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (Revised 2011). J Spinal Cord Med. 2011;34:535–46.
Fehlings MG, Vaccaro A, Wilson JR, Singh A, W Cadotte D, Harrop JS, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS ONE. 2012;7:e32037.
Evaniew N, Files C, Smith C, Bhandari M, Ghert M, Walsh M, et al. The fragility of statistically significant findings from randomized trials in spine surgery: a systematic survey. Spine J. 2015;15:2188–97.
Bailey CS, Fisher CG, Dvorak MF. Type II error in the spine surgical literature. Spine. 2004;29:1146–9.
Chow S-C. Sample size calculations for clinical trials. Wiley Interdiscip Rev Comput Stat. 2011;3:414–27.
Ko H-Y. Revisit spinal shock: pattern of reflex evolution during spinal shock. Korean J Neurotrauma. 2018;14:47–54.
Schouten R, Albert T, Kwon BK. The spine-injured patient: initial assessment and emergency treatment. J Am Acad Orthop Surg. 2012;20:336–46.
Geisler FH, Coleman WP, Grieco G, Poonian D. The Sygen multicenter acute spinal cord injury study. Spine. 2001;26:S87–S98.
Maynard FM, Reynolds GG, Fountain S, Wilmot C, Hamilton R. Neurological prognosis after traumatic quadriplegia. Three-year experience of California Regional Spinal Cord Injury Care System. J Neurosurg. 1979;50:611–6.
Brown PJ, Marino RJ, Herbison GJ, Ditunno JF. The 72-hour examination as a predictor of recovery in motor complete quadriplegia. Arch Phys Med Rehabil. 1991;72:546–8.
Herbison GJ, Zerby SA, Cohen ME, Marino RJ, Ditunno JF Jr. Motor power differences within the first two weeks post-SCI in cervical spinal cord-injured quadriplegic subjects. J Neurotrauma. 1992;9:373–80.
Marino RJ, Burns S, Graves DE, Leiby BE, Kirshblum S, Lammertse DP. Upper- and lower-extremity motor recovery after traumatic cervical spinal cord injury: an update from the national spinal cord injury database. Arch Phys Med Rehabil. 2011;92:369–75.
Acknowledgements
We would like to thank the Vancouver Spine Research Program team at Vancouver General Hospital for their help in data collection. BKK is the Canada Research Chair in Spinal Cord Injury and Dvorak Chair in Spine Trauma.
Funding
The Rick Hansen Spinal Cord Injury Registry and this work are supported by funding from the Rick Hansen Institute, Health Canada and Western Economic Diversification Canada.
Author information
Authors and Affiliations
Contributions
BKK, NE, NF, VKN, and BS designed the study. TA, RC-M, MD, ND, NE, CF, BKK, VKN, SP, BS, JS, and ZW assisted with the data acquisition. NE, NF, and BS performed the analysis of the data. NE led paper preparation and all authors contributed to the interpretation of the data and helped to write, review and edit the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All local research ethics board approvals were obtained prior to recruitment of participants. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Evaniew, N., Sharifi, B., Waheed, Z. et al. The influence of neurological examination timing within hours after acute traumatic spinal cord injuries: an observational study. Spinal Cord 58, 247–254 (2020). https://doi.org/10.1038/s41393-019-0359-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-019-0359-0
This article is cited by
-
Improving Diagnostic Workup Following Traumatic Spinal Cord Injury: Advances in Biomarkers
Current Neurology and Neuroscience Reports (2021)