Abstract
Study design
Cohort study.
Objectives
Long-term urological outcomes in patients with spinal lipoma after prophylactic tethered cord release (TCR) in infancy were investigated.
Setting
Children’s hospital in Yokohama, Japan.
Methods
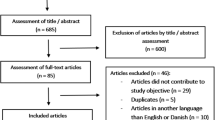
Children under one year of age with spinal lipoma who underwent TCR between 1990 and 2010 were investigated. According to Arai’s classification, lipomas other than filar lipoma were classified into four types: caudal, dorsal, transitional, and lipomyelomeningocele. The level of the conus medullaris was divided into three categories: L3-5, L5/S1, and sacral. Urological outcomes, including the need for clean intermittent catheterization (CIC), urinary incontinence, presence of renal deterioration, and the need for bladder augmentation, were investigated by both lipoma type and level of the conus medullaris.
Results
Fifty-three patients met the inclusion criteria. The median follow-up period was 14.2 years (interquartile range 9.6–17.6 years). Of the 53 patients, ten (19%) were on CIC, and six (11%) were incontinent. Overall, two patients (4%) had renal deterioration detected by DMSA renal scan, and two (4%) needed augmentation cystoplasty. Of the lipoma types, transitional type showed the worst outcomes with respect to need for CIC (54%) and urinary incontinence (38%). There were no significant differences in renal deterioration and the rate of bladder augmentation by lipoma type. No urological outcomes were significantly associated with conus level.
Conclusions
Even after prophylactic TCR in infancy in children with spinal lipoma, 19% of patients needed CIC in long-term follow-up. Of the lipoma types, transitional type showed the worst outcomes with respect to need for CIC and urinary incontinence.
Similar content being viewed by others

Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated and analyzed in the current study are available from the corresponding author on request.
References
Satar N, Bauer SB, Scott RM, Shefner J, Kelly M, Darbey M. Late effects of early surgery on lipoma and lipomeningocele in children less than 1 year old. J Urol. 1997;157:1434–7.
Wu HY, Kogan BA, Baskin LS, Edwards MS. Long-term benefits of early neurosurgery for lipomyelomeningocele. J Urol. 1998;160:511–4.
Pang D, Zovickian J, Oviedo A. Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode, part II: outcome analysis and preoperative profiling. Neurosurgery. 2010;66:253–72. discussion 272-3
White JT, Samples DC, Prieto JC, Tarasiewicz I. Systematic review of urologic outcomes from tethered cord release in occult spinal dysraphism in children. Curr Urol Rep. 2015;16:78.
Yerkes EB, Halline C, Yoshiba G, Meyer TA, Rosoklija I, Bowman R, et al. Lipomyelomeningocele for the urologist: should we view it the same as myelomeningocele? J Pediatr Urol. 2017;13:371.e1–371.e8.
Chapman PH. Congenital intraspinal lipomas: anatomic considerations and surgical treatment. Child’s Brain. 1982;9:37–47.
Arai H, Sato K, Okuda O, Miyajima M, Hishii M, Nakanishi H, et al. Surgical experience of 120 patients with lumbosacral lipomas. Acta Neurochir. 2001;143:857–64.
Hoffman HJ, Taecholarn C, Hendrick EB, Humphreys RP. Management of lipomyelomeningoceles. Experience at the Hospital for Sick Children, Toronto. J Neurosurg. 1985;62:1–8.
Kanev PM, Lemire RJ, Loeser JD, Berger MS. Management and long-term follow-up review of children with lipomyelomeningocele, 1952–1987. J Neurosurg. 1990;73:48–52.
Sawin KJ, Liu T, Ward E, Thibadeau J, Schechter MS, Soe MM, et al. The National Spina Bifida Patient Registry: profile of a large cohort of participants from the first 10 clinics. J Pediatr. 2015;166:444–50.e1.
Atala A, Bauer SB, Dyro FM, Shefner J, Shillito J, Sathi S, et al. Bladder functional changes resulting from lipomyelomeningocele repair. J Urol. 1992;148(2 Pt 2):592–4.
Nogueira M, Greenfield SP, Wan J, Santana A, Li V. Tethered cord in children: a clinical classification with urodynamic correlation. J Urol. 2004;172(4 Pt 2):1677–80.
Macejko AM, Cheng EY, Yerkes EB, Meyer T, Bowman RM, Kaplan WE. Clinical urological outcomes following primary tethered cord release in children younger than 3 years. J Urol. 2007;178(4 Pt 2):1738–42. discussion 1742-3
Guerra LA, Pike J, Milks J, Barrowman N, Leonard M. Outcome in patients who underwent tethered cord release for occult spinal dysraphism. J Urol. 2006;176(4 Pt 2):1729–32.
Woo J, Palazzi K, Dwek J, Kaplan G, Chiang G. Early clean intermittent catheterization may not prevent dimercaptosuccinic acid renal scan abnormalities in children with spinal dysraphism. J Pediatr Urol. 2014;10:274–7.
Pang D, Zovickian J, Oviedo A. Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode: part I-surgical technique. Neurosurgery. 2009;65:511–28. discussion 528-9
McGuire EJ, Woodside JR, Borden TA, Weiss RM. Prognostic value of urodynamic testing in myelodysplastic patients. J Urol. 1981;126:205–9.
Shiroyanagi Y, Suzuki M, Matsuno D, Yamazaki Y. The significance of 99mtechnetium dimercapto-succinic acid renal scan in children with spina bifida during long-term followup. J Urol. 2009;181:2262–6.
Routh JC, Joseph DB, Liu T, Schechter MS, Thibadeau JK, Wallis MC, et al. Bladder reconstruction rates differ among centers participating in National Spina Bifida Patient Registry. J Urol. 2018;199:268–73.
Wang HH, Lloyd JC, Wiener JS, Routh JC. Nationwide trends and variations in urological surgical interventions and renal outcome in patients with spina bifida. J Urol. 2016;195(4 Pt 2):1189–94.
Dudley AG, Adams MC, Brock JW 3rd, Clayton DB, Joseph DB, Koh CJ, et al. Interrater reliability in interpretation of neuropathic pediatric urodynamic tracings: an expanded multicenter study. J Urol. 2018;199:1337–43.
Guerra L, Leonard M, Castagnetti M. Best practice in the assessment of bladder function in infants. Ther Adv Urol. 2014;6:148–64.
Author information
Authors and Affiliations
Contributions
CH and YY initiated the research question and the protocol for data analysis. CH was responsible for the data analysis and interpretation, under the supervision of YY. CH wrote the manuscript, under the supervision of YY. YK, HS, and DH contributed to the interpretation of the results. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hayashi, C., Kumano, Y., Hirokawa, D. et al. Long-term urological outcomes of spinal lipoma after prophylactic untethering in infancy: real-world outcomes by lipoma anatomy. Spinal Cord 58, 490–495 (2020). https://doi.org/10.1038/s41393-019-0385-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-019-0385-y
This article is cited by
-
Spinal cord lipomas: lessons learned in the era of total resection
Child's Nervous System (2024)
-
Lumbosacral lipoma in childhood, how strong is the evidence base? A systematic review
Child's Nervous System (2024)
-
Surgery for spina bifida occulta: spinal lipoma and tethered spinal cord
Child's Nervous System (2023)
-
Radical resection of lumbosacral lipomas in children: the Great Ormond Street Hospital experience
Child's Nervous System (2022)
-
Does conus morphology have implications for outcome in lumbosacral lipoma?
Child's Nervous System (2021)