Abstract
Study design
Prospective cohort study.
Objectives
To validate a Clinical Prediction Rule (CPR) for ambulation in a non-traumatic spinal cord injury population (NTSCI).
Setting
Tertiary spinal rehabilitation inpatient service, Melbourne, Australia.
Methods
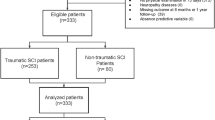
Adults with confirmed NTSCI were recruited between April 2013 and July 2017. Data based on the original van Middendorp CPR (age and four neurological variables) were collected from participant’s medical records and by interview. The Spinal Cord Independence Measure item 12 was used to quantify the ability to walk at 6 and 12 months. A receiver operator curve (ROC) was utilised to determine the performance of the CPR. Ambulatory outcomes were compared for AIS A, B, C and D and aetiology groups.
Results
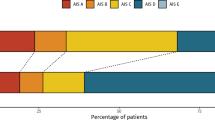
The area under the ROC curve (AUC) was 0.94 with 95% confidence interval (CI) 0.86–1.0 (n = 52). Overall accuracy was 75% at 6 months and 82% at 12 months. For the whole cohort the sensitivity at 12 months was 95% and specificity 73%. However, specificity for AIS C and D was only 50%.
Conclusion
The CPR correctly predicted those who did not walk at 6 and 12 months following NTSCI, but was less accurate in predicting those who would walk particularly those with an AIS C or D classification. This CPR may be useful to inform planning for future care in individuals with NTSCI, particularly for those who are not expected to walk. Further research with larger sample sizes is required to determine if the trends identified in this study are generalisable.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Change history
14 April 2020
A Correction to this paper has been published: https://doi.org/10.1038/s41393-020-0466-y
References
Adams RD, Salam-Adams M. Chronic nontraumatic diseases of the spinal cord. Neurol Clin. 1991;9:605–23.
New PW, Reeves RK, Smith É, Eriks-Hoogland I, Gupta A, Scivoletto G, et al. International retrospective comparison of inpatient rehabilitation for patients with spinal cord dysfunction: differences according to etiology. Arch Phys Med Rehabil. 2016;97:380–5.
New PW, Cripps RA, Bonne Lee B. Global maps of non-traumatic spinal cord injury epidemiology: towards a living data repository. Spinal Cord. 2014;52:97–109.
Scivoletto G, Farchi S, Laurenza L, Molinari M. Traumatic and non-traumatic spinal cord lesions: an Italian comparison of neurological and functional outcomes. Spinal Cord. 2011;49:391–6.
Ditunno PL, Patrick M, Stineman M, Ditunno JF. Who wants to walk? Preferences for recovery after SCI: a longitudinal and cross-sectional study. Spinal Cord. 2008;46:500–6.
Ditunno JF Jr. Predicting recovery after spinal cord injury: a rehabilitation imperative. Arch Phys Med Rehabil. 1999;80:361–4.
Scivoletto G, Tamburella F, Laurenza L, Torre M, Molinari M. Who is going to walk? A review of the factors influencing walking recovery after spinal cord injury. Front Human Neuroscience. 2014;8:1.
Sturt RN, Holland AE, New PW. Walking ability at discharge from inpatient rehabilitation in a cohort of non-traumatic spinal cord injury patients. Spinal Cord. 2009;47:763.
New PW, Jackson T. The costs and adverse events associated with hospitalization of patients with spinal cord injury in Victoria, Australia. Spine. 2010;35:796–802.
van Middendorp JJ, Hosman AJF, Donders ART, Pouw MH, Ditunno JF, Curt A, et al. A clinical prediction rule for ambulation outcomes after traumatic spinal cord injury: a longitudinal cohort study. Lancet. 2011;377:1004–10.
van Silfhout L, Peters AEJ, Graco M, Schembri R, Nunn AK, Berlowitz DJ. Validation of the Dutch clinical prediction rule for ambulation outcomes in an inpatient setting following traumatic spinal cord injury. Spinal Cord. 2015;54:614.
Malla R. External validation study of a clinical prediction rule for ambulation outcomes after traumatic spinal cord injuries: University of Texas; School of Public Health; Houston, Texas 2013.
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. SCIM—spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord. 1997;35:850.
Hicks KE, Zhao Y, Fallah N, Rivers CS, Noonan VK, Plashkes T, et al. A simplified clinical prediction rule for prognosticating independent walking after spinal cord injury: a prospective study from a Canadian multicenter spinal cord injury registry. Spine J. 2017;17:1383–92.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (Revised 2011). J Spinal Cord Med. 2011;34:535–46.
Phan P, Budhram B, Zhang Q, Rivers CS, Noonan VK, Plashkes T, et al. Highlighting discrepancies in walking prediction accuracy for patients with traumatic spinal cord injury: an evaluation of validated prediction models using a Canadian Multicenter Spinal Cord Injury Registry. Spine J. 2019;19:703 710.
Gupta A, Taly AB, Srivastava A, Vishal S, Murali T. Traumatic vs non-traumatic spinal cord lesions: comparison of neurological and functional outcome after in-patient rehabilitation. Spinal Cord. 2008;46:482–7.
Nater A, Fehlings MG. Clinical prediction rules: the importance of the validation phase. Spine J. 2017;17:1393–6.
New PW, Marshall R. International Spinal Cord Injury Data Sets for non-traumatic spinal cord injury. Spinal Cord. 2014;52:123–32.
Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC, et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil. 2007;29:1926–33.
Itzkovich M, Tamir A, Philo O, Steinberg F, Ronen J, Spasser R, et al. Reliability of the Catz-Itzkovich spinal cord independence measure assessment by interview and comparison with observation. Am J Phys Med Rehabil. 2003;82:267–72.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36.
Kim CM, Eng JJ, Whittaker MW. Level walking and ambulatory capacity in persons with incomplete spinal cord injury: relationship with muscle strength. Spinal cord. 2004;42:156–62.
Acknowledgements
We gratefully acknowledge Physiotherapists Genevieve Hendrey and Adele Winter from Caulfield Hospital for their contribution to participant recruitment.
Funding
This project was in part financially supported by an Alfred Health small research grant.
Author information
Authors and Affiliations
Contributions
RS and PN conceived the idea for the project; RS collected the data; BH analysed the data; BH, AH and CB interpreted the data; CB completed the literature review; CB wrote the first draft of the paper and all authors revised the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Ethical approval
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. Approval was obtained from the Alfred Health Human Research Ethics Committee; ethics number = 114/13
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sturt, R., Hill, B., Holland, A. et al. Validation of a clinical prediction rule for ambulation outcome after non-traumatic spinal cord injury. Spinal Cord 58, 609–615 (2020). https://doi.org/10.1038/s41393-019-0386-x
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41393-019-0386-x
This article is cited by
-
Performance of the Dutch clinical prediction rule for the ambulation outcome after spinal cord injury in a middle-income country clinical setting: an external validation study in the Thai retrospective cohort
Spinal Cord (2023)
-
Reliability and validity of the international standards for neurological classification of spinal cord injury in patients with non-traumatic spinal cord lesions
Spinal Cord (2022)