Abstract
Study design
Retrospective cohort study.
Objectives
The goal of this study was to assess the impact of multidrug resistant gram-negative organisms (MDRGNOs) on outcomes in those with SCI/D.
Setting
VA SCI System of Care, Department of Veterans Affairs, United States.
Methods
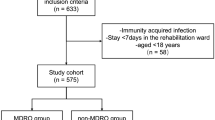
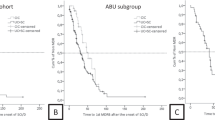
Multidrug resistance (MDR) was defined as being non-susceptible to ≥1 antibiotic in ≥3 antibiotic classes. Multivariable cluster-adjusted regression models were fit to assess the association of MDRGNOs with 1-year mortality, 30-day readmission, and postculture length of stay (LOS) stratified by case setting patients. Only the first culture per patient during the study period was included.
Results
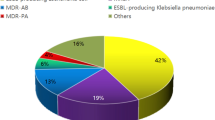
A total of 8,681 individuals with SCI/D had a culture with gram-negative bacteria during the study period, of which 33.0% had a MDRGNO. Overall, 954 (10.9%) died within 1 year of culture date. Poisson regression showed that MDR was associated with 1-year mortality among outpatients (IRR: 1.28, 95% CI, 1.06–1.54) and long-term care patients (OR: 2.06, 95% CI, 1.28–3.31). MDR significantly impacted postculture LOS in inpatients, as evidenced by a 10% longer LOS in MDR vs. non-MDR (IRR: 1.10, 95% CI, 1.02–1.19). MDR was not associated with increased 30-day readmission.
Conclusions
MDRGNOs are prevalent in SCI/D and MDR may result in poor outcomes. Further attention to prevention of infections, antibiotic stewardship, and management are warranted in this population.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data archiving
The datasets generated during and/or analyzed during the current study are not publicly available as the sample size is too large to obtain informed consents and HIPAA authorizations for public discloser of the final study data containing PII and/or PHI and would be inconsistent with the IRB approved waiver of informed consent and waiver of HIPPA authorization that was approved.
References
Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States. Atlanta, Georgia: Centers for Disease Control and Prevention; 2013. https://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.pdf. Accessed 7 Mar 2019.
Weiner LM, Webb AK, Limbago B, Dudeck MA, Patel J, Kallen AJ, et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2011–2014. Infect Control Hosp Epidemiol. 2016;37:1288–301.
Montgomerie JZ. Infections in patients with spinal cord injuries. Clin Infect Dis. 1997;25:1285–90.
Evans CT, LaVela SL, Weaver FM, Priebe M, Sandford P, Niemiec S, et al. Epidemiology of hospital-acquired infections in veterans with spinal cord injury and disorder. Infect Control Hosp Epidemiol. 2008;29:234–42.
Fitzpatrick MA, Suda KJ, Safdar N, Goldstein B, Jones MM, Poggensee L, et al. Unique risks and clinical outcomes associated with extended-spectrum betalactamase Enterobacteriaceae in veterans with spinal cord injury/disorder: a case-case-control study. Infect Control Hosp Epidemiol. 2016;37:768–76.
Rabadi MH, Mayanna SK, Vincent AS. Predictors of mortality in veterans with traumatic spinal cord injury. Spinal Cord. 2013;51:784–8.
DeJong G, Tian W, Hsieh CH, Junn C, Karam C, Ballard PH, et al. Rehospitalization in the first year of traumatic spinal cord injury after discharge from medical rehabilitation. Arch Phys Med Rehabil. 2013;94:S87–97.
LaVela SL, Evans CT, Miskevics S, Parada JP, Priebe M, Weaver FM. Long-term outcomes from nosocomial infections in persons with spinal cord injuries and disorders. Am J Infect Control. 2007;35:393–400.
Nelson RE, Slayton RB, Stevens VW, Jones MM, Khader K, Rubin MA, et al. Attributable mortality of healthcare-associated infections due to multidrug-resistant gram-negative bacteria and methicillin-resistant staphylococcus aureus. Infect Control Hosp Epidemiol. 2017;38:848–56.
Fitzpatrick MA, Suda KJ, Safdar N, Burns SP, Jones MM, Poggensee L, et al. Changes in bacterial epidemiology and antibiotic resistance among Veterans with spinal cord injury/disorder over the past 9 years. J Spinal Cord Med. 2018;41:199–207.
Evans CT, Fitzpatrick MA, Jones MM, Burns SP, Poggensee L, Ramanathan S, et al. Prevalence and factors associated with multidrug-resistant gram-negative organisms in patients with spinal cord injury. Infect control Hosp Epidemiol. 2017;38:1464–71.
Kale IO, Fitzpatrick MA, Suda KJ, Burns SP, Poggensee L, Ramanathan S, et al. Risk factors for community-associated multidrug-resistant Pseudomonas aeruginosa in veterans with spinal cord injury and disorder: a retrospective cohort study. Spinal Cord. 2017;55:687–91.
Ramanathan S, Suda KJ, Fitzpatrick MA, Poggensee L, LaVela SL, Burns SP, et al. Multidrug-resistant Acinetobacter: Risk factors and outcomes in veterans with spinal cord injuries and disorders. Am J Infect Control. 2017;45:1183–9.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81.
Agresti A. Categorical data analysis. 3rd ed. Hoboken, New Jersey: John Wiley & Sons; 2013.
Mylotte JM, Graham R, Kahler L, Young BL, Goodnough S. Impact of nosocomial infection on length of stay and functional improvement among patients admitted to an acute rehabilitation unit. Infect Control Hosp Epidemiol. 2001;22:83–7.
Giske CG, Monnet DL, Cars O, Carmeli Y. ReAct-action on antibiotic resistance. clinical and economic impact of common multidrug-resistant gram-negative bacilli. Antimicrob Agents Chemo. 2008;52:813–21.
Patel G, Huprikar S, Factor SH, Jenkins SG, Calfee DP. Outcomes of carbapenem-resistant Klebsiella pneumoniae infection and the impact of antimicrobial and adjunctive therapies. Infect Control Hosp Epidemiol. 2008;29:1099–106.
Funding
This work was supported by funding from the Veterans Health Administration, Office of Research and Development, Rehabilitation Research and Development Service SPIRE Award (grant no. B-1583-P). The views expressed in this article are those of the authors and do not necessarily reflect the policy of the Department of Veterans Affairs or the US government.
Author information
Authors and Affiliations
Contributions
CTE was the principal investigator and responsible for overseeing the project that the data were obtained from. CT also provided guidance and expertize in epidemiological methods and reviewing the manuscript. SR was responsible for data analysis and writing the manuscript. MAF and KJS provided helped with writing the discussion and providing infectious disease expertize. SPB and SLV provided spinal cord injury expertise related to the paper and findings. MMJ provided clinical experience with VA microbiology data and infectious disease expertize. All authors provided edits and revisions of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
This study was approved by the Edward Hines Jr. VA Hospital IRB. We certify that all applicable institutional and governmental regulations concerning the ethical use of human subjects data were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ramanathan, S., Fitzpatrick, M.A., Suda, K.J. et al. Multidrug-resistant gram-negative organisms and association with 1-year mortality, readmission, and length of stay in Veterans with spinal cord injuries and disorders. Spinal Cord 58, 596–608 (2020). https://doi.org/10.1038/s41393-019-0393-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-019-0393-y
This article is cited by
-
The prevalence of antibiotic-resistant and multidrug-resistant bacteria in urine cultures from inpatients with spinal cord injuries and disorders: an 8-year, single-center study
BMC Infectious Diseases (2022)
-
Epidemiology and outcomes associated with carbapenem-resistant Acinetobacter baumannii and carbapenem-resistant Pseudomonas aeruginosa: a retrospective cohort study
BMC Infectious Diseases (2022)
-
Multidrug-resistant bacteria in urine culture among patients with spinal cord injury and disorder: Time to first detection and analysis of risk factors
Spinal Cord (2022)