Abstract
Study design
Cross-sectional.
Objective
To investigate the associations of a set of psychosocial resources with pain and pain-related factors in individuals with spinal cord injury (SCI) and chronic pain.
Setting
Community, Switzerland.
Methods
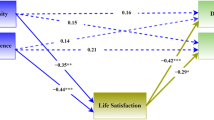
Data from 1,064 individuals with chronic pain who participated in the second community survey of the Swiss Spinal Cord Injury Cohort Study (Survey 2017) were analyzed. Multiple linear regression modeling was performed to test the hypotheses that higher levels of psychosocial resources (self-efficacy, self-esteem, purpose in life, optimism, hope, social support, sense of belonging) are negatively associated with pain intensity, pain interference and depressive symptoms.
Results
Higher self-esteem, optimism and hope were related to less pain interference and all psychosocial resources under study were negatively associated with depressive symptoms in final models. However, neither of the psychosocial resources was related to pain intensity when models were adjusted for pain interference and depressive symptoms.
Conclusions
These findings strengthen the evidence that psychosocial resources can have an impact on pain interference and depressive symptoms as pain-related factors, and support the notion that psychosocial resources might be promising targets for pain interventions in individuals with SCI.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Rubinelli S, Glassel A, Brach M. From the person’s perspective: perceived problems in functioning among individuals with spinal cord injury in Switzerland. J Rehabil Med. 2016;48:235–43.
Müller R, Brinkhof MW, Arnet U, Hinrichs T, Landmann G, Jordan X, et al. Prevalence and associated factors of pain in the Swiss spinal cord injury population. Spinal Cord. 2017;55:346–54.
van Gorp S, Kessels AG, Joosten EA, van Kleef M, Patijn J. Pain prevalence and its determinants after spinal cord injury: a systematic review. Eur J Pain. 2015;19:5–14.
Treede R-D, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the International Classification of Diseases (ICD-11). Pain. 2019;160:19–27.
Müller R, Landmann G, Béchir M, Hinrichs T, Arnet U, Jordan X, et al. Chronic pain, depression and quality of life in individuals with spinal cord injury: mediating role of participation. J Rehabil Med. 2017;49:489–96.
Kronborg C, Handberg G, Axelsen F. Health care costs, work productivity and activity impairment in non-malignant chronic pain patients. Eur J Health Econ. 2009;10:5–13.
Main C, Spanswick C, Watson P. The nature of disability. In: Parker H, Watson P (eds.). Pain management: an interdisciplinary approach. 1st edn. (Curchill Livinstone, Edinburgh, 2000), pp 89-106.
Turk DC, Wilson HD, Cahana A. Treatment of chronic non-cancer pain. Lancet. 2011;377:2226–35.
Iddon JE, Dickson JM, Unwin J. Positive psychological interventions and chronic non-cancer pain: a systematic review of the literature. Int J Appl Posit Psychol. 2016;1:133–57.
Heutink M, Post M, Overdulve C, Pfennings L, van de Vis W, Vrijens N, et al. Which pain coping strategies and cognitions are associated with outcomes of a cognitive behavioral intervention for neuropathic pain after spinal cord injury? Top Spinal Cord Inj Rehabil. 2013;19:330–40.
Robinson-Whelen S, Hughes RB, Taylor HB, Markley R, Vega JC, Nosek TM, et al. Promoting psychological health in women with SCI: Development of an online self-esteem intervention. Disabil Health J. 2020;13:100867.
Snyder CR, Lopez SJ (eds.). Oxford handbook of positive psychology. 1st edn. (Oxford University Press, New York, 2009).
Bushnell MC, Ceko M, Low LA. Cognitive and emotional control of pain and its disruption in chronic pain. Nat Rev Neurosci. 2013;14:502–11.
Finan PH, Garland EL. The role of positive affect in pain and its treatment. Clin J Pain. 2015;31:177–87.
van Diemen T, Crul T, van Nes I, Group S-S, Geertzen JH, Post MW. Associations between self-efficacy and secondary health conditions in people living with spinal cord injury: A systematic review and meta-analysis. Arch Phys Med Rehabil. 2017;98:2566–77.
Geyh S, Nick E, Stirnimann D, Ehrat S, Michel F, Peter C, et al. Self-efficacy and self-esteem as predictors of participation in spinal cord injury—an ICF-based study. Am J Phys Med Rehabil. 2012;50:699–706.
Harper LA, Coleman JA, Olivera SL, Perdomo JL, Arango JA. Comparison of mental health between individuals with spinal cord injury and able-bodied controls in Neiva, Colombia. J Rehabil Res Dev. 2014;51:127–36.
Müller R, Terrill AL, Jensen MP, Molton IR, Ravesloot C, Ipsen C. Happiness, pain intensity, pain interference, and distress in individuals with physical disabilities. Am J Phys Med Rehabil. 2015;94:1041–51.
Peter C, Müller R, Post MW, van Leeuwen C, Werner CS, Geyh S. Depression in spinal cord injury: Assessing the role of psychological resources. Rehabil Psychol. 2015;60:67–80.
Jensen MP, Moore MR, Bockow TB, Ehde DM, Engel JM. Psychosocial factors and adjustment to chronic pain in persons with physical disabilities: a systematic review. Arch Phys Med Rehabil. 2011;92:146–60.
Basten-Günther J, Peters M, Lautenbacher S. Optimism and the experience of pain: a systematic review. Behav Med. 2019;45:323–39.
Wright MA, Wren AA, Somers TJ, Goetz MC, Fras AM, Huh BK, et al. Pain acceptance, hope, and optimism: relationships to pain and adjustment in patients with chronic musculoskeletal pain. J Pain. 2011;12:1155–62.
Vassend O, Quale A, Røise O, Schanke A. Predicting the long-term impact of acquired severe injuries on functional health status: The role of optimism, emotional distress and pain. Spinal Cord. 2011;49:1193–7.
Geyh S, Müller R, Peter C, Bickenbach JE, Post MW, Stucki G, et al. Capturing the psychologic-personal perspective in spinal cord injury. Am J Phys Med Rehabil. 2011;90:79–96.
Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19.
Gross-Hemmi MH, Gemperli A, Fekete C, Brach M, Schwegler U, Stucki G. Methodology and study population of the second Swiss national community survey of functioning after spinal cord injury. Spinal Cord. https://doi.org/10.1038/s41393-020-00584-3.
Kalpakjian CZ, Scelza WM, Forchheimer MB, Toussaint LL. Preliminary reliability and validity of a spinal cord injury secondary conditions scale. J Spinal Cord Med. 2007;30:131–9.
Swiss Spinal Cord Injury Cohort Study (SwiSCI). Survey 2017 [Internet]. Nottwil: Schweizer Paraplegiker-Forschung; 2018 [Accessed 7 Sep 2020]. https://www.swisci.ch/en/research-projects-home/study-design/community-survey/survey-2017.
Textor J, Hardt J, Knüppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiol. 2011;22:745.
Fekete C, Eriks-Hoogland I, Baumberger M, Catz A, Itzkovich M, Lüthi H, et al. Development and validation of a self-report version of the Spinal Cord Independence Measure (SCIM III). Spinal Cord. 2013;51:40–47.
Cohen J. A power primer. Psychol Bull. 1992;112:155–9.
Enders CK (ed.). Applied missing data analysis. (Guilford press, New York, 2010).
Fredrickson BL. The broaden–and–build theory of positive emotions. Philos Trans R Soc Lond B. 2004;359:1367–77.
Müller R, Gertz KJ, Molton IR, Terrill AL, Bombardier CH, Ehde DM, et al. Effects of a tailored positive psychology intervention on well-being and pain in individuals with chronic pain and a physical disability. Clin J Pain. 2016;32:32–44.
Acknowledgements
We thank the SwiSCI Steering Committee with its members Xavier Jordan, Fabienne Reynard (Clinique Romande de Réadaptation, Sion); Michael Baumberger, Hans Peter Gmünder (Swiss Paraplegic Center, Nottwil); Armin Curt, Martin Schubert (University Clinic Balgrist, Zürich); Margret Hund-Georgiadis, Kerstin Hug (REHAB Basel, Basel); Laurent Prince (Swiss Paraplegic Association, Nottwil); Heidi Hanselmann (Swiss Paraplegic Foundation, Nottwil); Daniel Joggi (Representative of persons with SCI); Nadja Münzel (Parahelp, Nottwil); Mirjam Brach, Gerold Stucki (Swiss Paraplegic Research, Nottwil); Armin Gemperli (SwiSCI Coordination Group at Swiss Paraplegic Research, Nottwil).
Funding
SwiSCI is hosted and funded by Swiss Paraplegic Research.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the conceptualization of the study. CB performed the data analysis, with support from CF, SK and HT. CB and CF drafted the manuscript and interpreted the results together with RM, GL, SK and HT. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was granted by the Medical Ethics Committee of Northwest- and Central Switzerland (EKNZ, Project-ID: 11042 PB_2016-02608, approved Dec 2016). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Braunwalder, C., Müller, R., Kunz, S. et al. Psychosocial resources and chronic pain in individuals with spinal cord injury: evidence from the second Swiss national community survey. Spinal Cord 59, 410–418 (2021). https://doi.org/10.1038/s41393-020-00577-2
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41393-020-00577-2
This article is cited by
-
Reciprocal association between pain and quality of life after newly acquired spinal cord injury
Quality of Life Research (2024)