Abstract
Study design
A retrospective cohort study.
Objectives
To document the prevalence of asymptomatic bacteriuria and to characterize the resistance patterns to antibiotics among children with neurogenic bladder who require clean intermittent catheterization, with an emphasis on multidrug resistance.
Setting
A national referral pediatric and adolescent rehabilitation facility in Jerusalem, Israel.
Methods
Routine urine cultures were collected before urodynamic studies in suitable individuals during 2010–2018. None of them had symptoms of urinary tract infection at the time of specimen collection. Cultures were defined as being positive if a single bacterial species was isolated together with a growth of over 105 colony-forming units/ml. Resistance patterns were defined as extended-spectrum beta-lactamase (ESBL) and resistant to 3 antimicrobial groups (multi-drug resistant, MDR).
Results
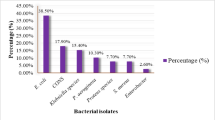
In total, 281 urine cultures were available for 186 participants (median age 7 years, range 0.5–18). Etiologies for CIC included myelomeningocele (n = 137, 74%), spinal cord injury (n = 16, 9%) and caudal regression syndrome (n = 9, 5%). Vesicoureteral reflux was diagnosed in 36 participants (19%), 14 of whom were treated with prophylactic antibiotics. Asymptomatic bacteriuria was present in 217 specimens (77%, 95%CI [0.72–0.82]). The bacteria species were E. coli (71%), Klebsiella (13%), and Proteus (10%). ESBL was found in 11% of the positive cultures and MDR in 9%, yielding a total of 34 (16% of positive cultures) positive for ESBL and/or MDR bacteria.
Conclusions
Asymptomatic bacteriuria and resistance to antimicrobials are common in pediatric individuals who require CIC.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Maison POM, Lazarus J. The management of paediatric neurogenic bladder: an approach in a resource-poor setting. Paediatr Int Child Health. 2017;37:280–5. https://doi.org/10.1080/20469047.2017.1351745.
Cass AS, Luxenberg M, Gleich P, Johnson CF, Hagen S. Clean intermittent catheterization in the management of the neurogenic bladder in children. J Urol. 1984;132:526–8. https://doi.org/10.1016/S0022-5347(17)49720-5.
Forster CS, Haslam DB, Jackson E, Goldstein SL. Utility of a routine urinalysis in children who require clean intermittent catheterization. J Pediatr Urol. 2017;13:488.e1–e5. https://doi.org/10.1016/j.jpurol.2017.01.016.
Ortiz TK, Velazquez N, Ding L, Routh JC, Wiener JS, Seed PC, et al. Predominant bacteria and patterns of antibiotic susceptibility in urinary tract infection in children with spina bifida. J Pediatr Urol. 2018;14:444.e1–e8. https://doi.org/10.1016/j.jpurol.2018.03.017.
Ferri M, Ranucci E, Romagnoli P, Giaccone V. Antimicrobial resistance: A global emerging threat to public health systems. Crit Rev Food Sci Nutr. 2017;57:2857–76. https://doi.org/10.1080/10408398.2015.1077192.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81. https://doi.org/10.1111/j.1469-0691.2011.03570.x.
Hill TC, Baverstock R, Carlson KV, Estey EP, Gray GJ, Hill DC, et al. Best practices for the treatment and prevention of urinary tract infection in the spinal cord injured population: The Alberta context Bladder management in the context of a spinal cord injury. Can Urol Assoc J. 2013;77:122–30. https://doi.org/10.5489/cuaj.337.
Pitout JD, Laupland KB. Extended-spectrum beta-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infect Dis. 2008;8:159–66. https://doi.org/10.1016/S1473-3099(08)70041-0.
Stein R, Bogaert G, Dogan HS, Hoen L, Kocvara R, Nijman RJM, et al. EAU/ESPU guidelines on the management of neurogenic bladder in children and adolescent part I diagnostics and conservative treatment. Neurourol Urodyn. 2020;39:45–57.
Ottolini MC, Shaer CM, Rushton HG, Majd M, Gonzales EC, Patel KM. Relationship of asymptomatic bacteriuria and renal scarring in children with neuropathic bladders who are practicing clean intermittent catheterization. J Pediatr. 1995;127:368–72. https://doi.org/10.1016/s0022-3476(95)70065-x
Zegers SH, Dieleman J, van der Bruggen T, Kimpen J, de Jong-de Vos van Steenwijk C. The influence of antibiotic prophylaxis on bacterial resistance in urinary tract infections in children with spina bifida [published correction appears in BMC Infect Dis. 2017;17:175]. BMC Infect Dis. 2017;17:63. https://doi.org/10.1186/s12879-016-2166-y.
Schlager TA, Anderson S, Trudell J, Hendley JO. Nitrofurantoin prophylaxis for bacteriuria and urinary tract infection in children with neurogenic bladder on intermittent catheterization. J Pediatr. 1998;132:704–8.
Johnson HW, Anderson JD, Chambers GK, Arnold WJ, Irwin BJ, Brinton JR. A short-term study of nitrofurantoin prophylaxis in children managed with clean intermittent catheterization. Pediatrics. 1994;93:752–5.
Massa LM, Hoffman JM, Cardenas DD. Validity, accuracy, and predictive value of urinary tract infection signs and symptoms in individuals with spinal cord injury on intermittent catheterization. J Spinal Cord Med. 2009;32:568–73.
Zegers BS, Winkler-Seinstra PL, Uiterwaal CS, de Jong TV, Kimpen JL, de Jong-de Vos van Steenwijk CC. Urinary tract infections in children with spina bifida: an inventory of 41 European centers. Pediatr Nephrol. 2009;24:783–8. https://doi.org/10.1007/s00467-008-1067-8.
Forster CS, Courter J, Jackson EC, Mortensen JE, Haslam DB. Frequency of multidrug-resistant organisms cultured from urine of children undergoing clean intermittent catheterization. J Pediatr Infect Dis Soc. 2017;6:332–8.
Snow-Lisy DC, Halline C, Johnson EK, Diaz-Saldano D, Meyer T, Yerkes EB. Reassessing the utility of routine urine culture with urodynamics: UTI incidence and risk factors. J Pediatr Urol. 2017;13:372.e1–e8.
Bonkat G, Pickard R, Bartoletti R, Cai T, Bruyere F, Geerlings SE, et al. EAU guidelines. Edn. presented at the EAU Annual Congress Copenhagen 2018. pp 39–41.
Bauer SB, Austin PF, Rawashdeh YF, de Jong TP, Franco I, Siggard C, et al. International children’s continence society’s recommendations for initial diagnostic evaluation and follow-up in congenital neuropathic bladder and bowel dysfunction in children. Neurourol Urodyn 2012;31:610–4.
Acknowledgements
We thank Nurit Twill for administrative assistance.
Author information
Authors and Affiliations
Contributions
RB-D and YB-Y conceived the idea and study design, RB-D analyzed the data, and led manuscript writing; FC, SD, RM, EK assisted with study design, data collection, audited data collection integrity. JB-C, RC, and YB-Y provided consult and guidance in manuscript writing. All authors have reviewed and approved this version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study protocol was reviewed and approved by the Alyns’ hospital Helsinki review committee.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ben-David, R., Carroll, F., Kornitzer, E. et al. Asymptomatic bacteriuria and antibiotic resistance profile in children with neurogenic bladder who require clean intermittent catheterization. Spinal Cord 60, 256–260 (2022). https://doi.org/10.1038/s41393-021-00679-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-021-00679-5