Abstract
Study design
Cross-cultural reliability and validity.
Objectives
To develop and validate the Korean version of the Sitting Balance Measure (SBM-K) in Korean persons with incomplete spinal cord injury (ISCI).
Setting
Tertiary care center.
Methods
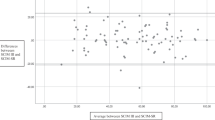
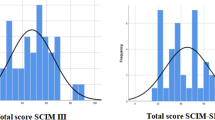
Twenty-nine persons with ISCI were evaluated using SBM-K, which was validated using the kappa coefficient and intraclass coefficient (ICC). The correlation between SBM-K individual items and total score was analyzed using Spearman’s correlation, and the internal consistency of test items was measured using Cronbach’s alpha. Additionally, the standard error measurement (SEM) and minimal detectable change (MDC) were measured. For the clinical validity of SBM-K, the correlation of SBM-K with the modified Sitting Balance Scale (mSBS) and the Korean-Spinal Cord Independence Measure-III (KSCIM-III) was determined via Spearman’s correlation. Linear regression was performed to determine whether SBM-K could predict KSCIM-III.
Results
The weighted kappa score of the SBM-K individual items and ICC of SBM-K total score were 0.76–0.83 (good–very good) and 0.98 (0.95–0.99), respectively. The correlation between the SBM-K total score and individual items was notable (r = 0.78–0.98). Cronbach’s alpha, SEM, and MDC of SBM-K were 0.98, 0.59, and 1.64, respectively. The clinical validity of SBM-K correlated with mSBS (r = 0.88) and KSCIM-III (r = 0.65–0.89). SBM-K accounted for 17–72% of the variance in predicting KSCIM-III.
Conclusions
SBM-K showed sufficient test-retest reliability, validity, and marginal measurement errors. SBM-K can serve as an optimal clinical assessment tool for Korean ISCI patients and may provide clinicians with reliable sitting balance assessment in Korean clinical settings.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Lee BB, Cripps RA, Fitzharris M, Wing PC. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord. 2014;52:110–6. https://doi.org/10.1038/sc.2012.158.
Reft J, Hasan Z. Trajectories of target reaching arm movements in individuals with spinal cord injury: effect of external trunk support. Spinal Cord. 2002;40:186–91. https://doi.org/10.1038/sj.sc.3101277.
Chen CL, Yeung KT, Bih LI, Wang CH, Chen MI, Chien JC. The relationship between sitting stability and functional performance in patients with paraplegia. Arch Phys Med Rehabil. 2003;84:1276–81. https://doi.org/10.1016/s0003-9993(03)00200-4.
Jørgensen V, Elfving B, Opheim A. Assessment of unsupported sitting in patients with spinal cord injury. Spinal Cord. 2011;49:838–43. https://doi.org/10.1038/sc.2011.9.
Wadhwa G, Aikat R. Development, validity and reliability of the Sitting Balance Measure (SBM) in spinal cord injury. Spinal Cord. 2016;54:319–23. https://doi.org/10.1038/sc.2015.148.
Quinzaños J, Villa AR, Flores AA, Pérez R. Proposal and validation of a clinical trunk control test in individuals with spinal cord injury. Spinal Cord. 2014;52:449–54. https://doi.org/10.1038/sc.2014.34.
Berg KO, Maki BE, Williams JI, Holliday PJ, Wood-Dauphinee SL. Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil. 1992;73:1073–80.
Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34:119–26. https://doi.org/10.1111/j.1532-5415.1986.tb05480.x.
Arora T, Oates A, Lynd K, Musselman KE. Current state of balance assessment during transferring, sitting, standing and walking activities for the spinal cord injured population: a systematic review. J Spinal Cord Med. 2020;43:10–23. https://doi.org/10.1080/10790268.2018.1481692.
American Spinal Injury Association. International standards for neurological classification of spinal cord injury. Chicago, IL: American Spinal Injury Association; 2003.
Wong SS, Yam MS, Ng SS. The Figure-of-Eight Walk Test: reliability and associations with stroke-specific impairments. Disabil Rehabil. 2013;35:1896–902. https://doi.org/10.3109/09638288.2013.766274.
Curtin F, Schulz P. Multiple correlations and Bonferroni’s correction. Biol Psychiatry. 1998;44:775–7.
Liaw LJ, Hsieh CL, Hsu MJ, Chen HM, Lin JH, Lo SK. Test-retest reproducibility of two short-form balance measures used in individuals with stroke. Int J Rehabil Res. 2012;35:256–62. https://doi.org/10.1097/MRR.0b013e3283544d20.
Chen HM, Hsieh CL, Sing Kai Lo S, Liaw LJ, Chen SM, Lin JH. The test-retest reliability of 2 mobility performance tests in patients with chronic stroke. Neurorehabil Neural Repair. 2007;21:347–52. https://doi.org/10.1177/1545968306297864.
Park KY, Chung YJ, Kim JH. The reliability and validity of the spinal cord independence measure (SCIM) III. J Korean Soc Occup Ther. 2009;17:97–109.
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. SCIM—spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord. 1997;35:850–6. https://doi.org/10.1038/sj.sc.3100504.
Wannapakhe J, Saensook W, Keawjoho C, Amatachaya S. Reliability and discriminative ability of the spinal cord independence measure III (Thai version). Spinal Cord. 2016;54:213–20. https://doi.org/10.1038/sc.2015.114.
Brennan P, Silman A. Statistical methods for assessing observer variability in clinical measures. BMJ 1992;304:1491–4. https://doi.org/10.1136/bmj.304.6840.1491.
Lu WS, Wang CH, Lin JH, Sheu CF, Hsieh CL. The minimal detectable change of the simplified stroke rehabilitation assessment of movement measure. J Rehabil Med. 2008;40:615–9. https://doi.org/10.2340/16501977-0230.
Altman DG, Bland JM. Measurement in medicine: the analysis of method comparison studies. Statistician. 1983;32:307–17. https://doi.org/10.2307/2987937.
Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. Appleton & Lange: Norwalk, Connecticut; 1993, pp 2–450.
Godi M, Franchignoni F, Caligari M, Giordano A, Turcato AM, Nardone A. Comparison of reliability, validity, and responsiveness of the mini-BESTest and Berg Balance Scale in patients with balance disorders. Phys Ther. 2013;93:158–67. https://doi.org/10.2522/ptj.20120171.
Lynch SM, Leahy P, Barker SP. Reliability of measurements obtained with a modified functional reach test in subjects with spinal cord injury. Phys Ther. 1998;78:128–33. https://doi.org/10.1093/ptj/78.2.128.
Patten C, Kothari D, Whitney J, Lexell J, Lum PS. Reliability and responsiveness of elbow trajectory tracking in chronic poststroke hemiparesis. J Rehabil Res Dev. 2003;40:487–500. https://doi.org/10.1682/jrrd.2003.11.0487.
Goldsmith CH, Boers M, Bombardier C, Tugwell P. Criteria for clinically important changes in outcomes: development, scoring and evaluation of rheumatoid arthritis patient and trial profiles. OMERACT Committee. J Rheumatol. 1993;20:561–5.
Flansbjer UB, Blom J, Brogårdh C. The reproducibility of berg balance scale and the single-leg stance in chronic stroke and the relationship between the two tests. PM R J Inj Funct Rehabil. 2012;4:165–70. https://doi.org/10.1016/j.pmrj.2011.11.004.
Schuck P, Zwingmann C. The ‘smallest real difference’ as a measure of sensitivity to change: a critical analysis. Int J Rehabil Res. 2003;26:85–91. https://doi.org/10.1097/00004356-200306000-00002.
Further reading
Beckerman H, Roebroeck ME, Lankhorst GJ, Becher JG, Bezemer PD, Verbeek AL. Smallest real difference, a link between reproducibility and responsiveness. Qual Life Res. 2001;10:571–8. https://doi.org/10.1023/a:1013138911638
Roebroeck ME, Harlaar J, Lankhorst GJ. The application of generalizability theory to reliability assessment: an illustration using isometric force measurements. Phys Ther 1993;73:386–95. https://doi.org/10.1093/ptj/73.6.386. discussion 396
Schreuders TA, Roebroeck ME, Goumans J, van Nieuwenhuijzen JF, Stijnen TH, Stam HJ. Measurement error in grip and pinch force measurements in patients with hand injuries. Phys Ther 2003;83:806–15. https://doi.org/10.1093/ptj/83.9.806
Acknowledgements
Editorial Support, in terms of English language editing, proofreading, and formatting, was provided by Editage.
Author information
Authors and Affiliations
Contributions
JL: conceptualization, writing—original draft, validation, investigation. SA: formal analysis, software. OK: resources. GK: writing—review and editing. MK: supervision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The study was approved by the National Rehabilitation Hospital Institutional Review Board (IRB File No. NRC-2019-05-032). All participants received explanations of the study protocol, and written informed consent was obtained.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lee, J., An, S., Kim, O. et al. Test-retest reliability and validity of the Sitting Balance Measure-Korean in individuals with incomplete spinal cord injury. Spinal Cord 60, 641–646 (2022). https://doi.org/10.1038/s41393-021-00715-4
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41393-021-00715-4
This article is cited by
-
Significance of physical factors on activities of daily living in patients with tetraplegia after spinal cord injury: a retrospective study
BMC Sports Science, Medicine and Rehabilitation (2024)
-
Quantifying unsupported sitting posture impairments in humans with cervical spinal cord injury using a head-mounted IMU sensor
Spinal Cord (2024)
-
Correspondence to “Test-retest reliability and validity of the Sitting Balance Measure-Korean in individuals with incomplete spinal cord injury”
Spinal Cord (2022)