Abstract
Study design
Randomized-controlled trial (RCT) with immediate intervention (IMM) and wait-list control (WLC) groups; WLC participants received the intervention during delivery to subsequent cohorts.
Objectives
Investigate the effectiveness and feasibility of a virtually-delivered exercise intervention.
Setting
Home and community.
Methods
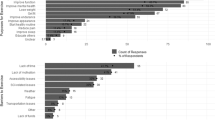
A total of 168 middle-aged (49.6 [12.3] years old) men (57%) and women (43%) who lived an average 15.5 (12.3) years with spinal cord injury (SCI) participated. The 16-week program provides users (a) website access with exercise information, resources, and 16 skill-building modules; (b) virtual 60-minute, group-based weekly meetings; and (c) a starter package of exercise equipment. Primary outcomes included subjective physical activity (IPAQ) and objective exercise (Polar A300 wrist-based activity monitor and H7 heart rate strap). Secondary outcomes included fitness indices during a maximal arm crank test, plus self-reported exercise barriers, exercise self-efficacy, and goal-directed thinking.
Results
RCT results indicate significant between group differences in participants’ self-reported weekly time spent in vigorous-intensity PA and goal directed thinking but not for fitness changes. Data combined for IMM and WLC participants from Polar monitoring show participants performed 150 min per week of aerobic exercise plus reported significantly greater time spent in moderate-PA, vigorous-PA, self-efficacy for exercise and nutrition, goal directed thinking, and exercise barriers. Oxygen uptake (V̇O2 peak) and power output (watts max) were the only physiologic measures to demonstrate significant change, with a moderate effect size.
Conclusion
This virtually-delivered program offers a promising approach to increase exercise among those with SCI and may help participants perceive fewer motivational barriers and greater self-efficacy.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data archiving
The datasets generated during and analyzed for the study are available from the corresponding author on request and will be archived at the Interuniversity Consortium for Political and Social Research (ICPSR) by the end of 2022.
References
Cowan RE. Exercise is medicine initiative: physical activity as a vital sign and prescription in adult rehabilitation practice. Arch Phys Med Rehab. 2016;97:S232–S7.
Cowan R, Malone L, Nash M. Exercise is Medicine™: Exercise prescription after SCI to manage cardiovascular disease risk factors. Topics in Spinal Cord Injury. Rehabilitation. 2009;14:69–83.
American College of Sports Medicine (ACSM). Exercise is medicine fact sheet: ACSM; 2012 [February, 2014]. Available from: http://www.exerciseismedicine.org/documents/EIMFactSheet2012_all.pdf.
Sallis RE. Exercise is medicine and physicians need to prescribe it! Br J Sports Med. 2009;43:3–4. https://doi.org/10.1136/bjsm.2008.054825.
U.S. Department of Health and Human Services. Physical activity and health: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996.
Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–34.
Nash MS, Groah SL, Gater DR Jr, Dyson-Hudson TA, Lieberman JA, Myers J, et al. Identification and management of cardiometabolic risk after spinal cord injury: clinical practice guideline for health care providers. Topics in Spinal Cord Injury. Rehabilitation. 2018;24:379–423.
Valent L, Dallmeijer A, Houdijk H, Talsma E, van der Woude L. The effects of upper body exercise on the physical capacity of people with a spinal cord injury: a systematic review. Clin Rehabil. 2007;21:315–30.
Ravenek KE, Ravenek MJ, Hitzig SL, Wolfe DL. Assessing quality of life in relation to physical activity participation in persons with spinal cord injury: a systematic review. Disabil Health J. 2012;5:213–23. https://doi.org/10.1016/j.dhjo.2012.05.005. Epub 2012/10/02; PubMed PMID: 23021731.
van der Scheer JW, Ginis KAM, Ditor DS, Goosey-Tolfrey VL, Hicks AL, West CR, et al. Effects of exercise on fitness and health of adults with spinal cord injury: a systematic review. Neurology. 2017;89:736–45.
Farrow M, Nightingale TE, Maher J, McKay CD, Thompson D, Bilzon JLJ. Effect of Exercise on Cardiometabolic Risk Factors in Adults With Chronic Spinal Cord Injury: a systematic review. Arch Phys Med Rehabil. 2020. Epub 2020/05/24. https://doi.org/10.1016/j.apmr.2020.04.020. PubMed PMID: 32445849.
Tomasone JR, Wesch NN, Ginis KAM, Noreau L. Spinal cord injury, physical activity, and quality of life: a systematic review. Kinesiol Rev. 2013;2:113–29. https://doi.org/10.1123/krj.2.2.113.
van den Berg-Emons RJ, Bussmann JB, Haisma JA, Sluis TA, van der Woude LH, Bergen MP, et al. A prospective study on physical activity levels after spinal cord injury during inpatient rehabilitation and the year after discharge. Arch Phys Med Rehabil. 2008;89:2094–101. https://doi.org/10.1016/j.apmr.2008.04.024. Epub 2008/11/11 PubMed PMID: 18996237.
Martin Ginis KA, Latimer AE, Arbour-Nicitopoulos KP, Buchholz AC, Bray SR, Craven BC, et al. Leisure time physical activity in a population-based sample of people with spinal cord injury Part I: Demographic and injury-related correlates. Arch Phys Med Rehabil. 2010;91:722–8. 10/1016/j.apmr.2009.12.027.
Hiremath SV, Amiri AM, Thapa-Chhetry B, Snethen G, Schmidt-Read M, Ramos-Lamboy M, et al. Mobile health-based physical activity intervention for individuals with spinal cord injury in the community: A pilot study. PLoS ONE. 2019;14:e0223762. Epub 2019/10/16. https://doi.org/10.1371/journal.pone.0223762. PubMed PMID: 31613909; PubMed Central PMCID: PMC6793862.
Nooijen CF, Stam HJ, Bergen MP, Bongers-Janssen HM, Valent L, van Langeveld S, et al. A behavioural intervention increases physical activity in people with subacute spinal cord injury: a randomised trial. J Physiother. 2016;62:35–41. https://doi.org/10.1016/j.jphys.2015.11.003. Epub 2015/12/25; PubMed PMID: 26701155.
Nightingale TE, Rouse PC, Walhin JP, Thompson D, Bilzon JLJ. Home-based exercise enhances health-related quality of life in persons with spinal cord injury: a randomized controlled trial. Arch Phys Med Rehabil. 2018;99:1998–2006 e1. https://doi.org/10.1016/j.apmr.2018.05.008. Epub 2018/06/15; PubMed PMID: 29902472.
Tomasone JR, Arbour-Nicitopoulos KP, Latimer-Cheung AE, Martin Ginis KA. The relationship between the implementation and effectiveness of a nationwide physical activity telephone counseling service for adults with spinal cord injury. Disabil Rehabil. 2018;40:527–37. https://doi.org/10.1080/09638288.2016.1261415. Epub 2016/12/29; PubMed PMID: 28029067.
Latimer AE, Ginis KAM, Arbour KP. The efficacy of an implementation intention intervention for promoting physical activity among individuals with spinal cord injury: A randomized controlled trial. Rehabil Psychol. 2006;51:273–80. https://doi.org/10.1037/0090-5550.51.4.273. PubMed PMID: WOS:000242144300001.
Arbour-Nicitopoulos KP, Ginis KAM, Latimer AE. Planning, leisure-time physical activity, and coping self-efficacy in persons with spinal cord injury: A randomized controlled trial. Archives of Physical and Medical. Rehabilitation. 2009;90:2003–11. https://doi.org/10.1016/j.apmr.2009.06.019.
Wise HH, Thomas J, Nietert PJ, Brown DD, Sword DO, Diehl N. Home physical activity programs for the promotion of health and wellness in individuals with spinal cord injury. Topics in Spinal Cord Injury. Rehabilitation. 2011;14:122–32.
Bombardier CH, Dyer JR, Burns P, Crane DA, Takahashi MM, Barber J, et al. A tele-health intervention to increase physical fitness in people with spinal cord injury and cardiometabolic disease or risk factors: a pilot randomized controlled trial. Spinal Cord. 2020. Epub 2020/07/23. https://doi.org/10.1038/s41393-020-0523-6. PubMed PMID: 32694748.
Lai B, Wilroy J, Young HJ, Howell J, Rimmer JH, Mehta T, et al. A Mobile App to Promote Adapted Exercise and Social Networking for People With Physical Disabilities: Usability Study. JMIR Form Res. 2019;3:e11689. Epub 2019/03/20. https://doi.org/10.2196/11689. PubMed PMID: 30888325; PubMed Central PMCID: PMC6444218.
Wilroy JD, Lai B, Davlyatov G, Mehta T, Thirumalai M, Rimmer JH. Correlates of adherence in a home-based, self-managed exercise program tailored to wheelchair users with spinal cord injury. Spinal Cord. 2020. Epub 2020/06/17. https://doi.org/10.1038/s41393-020-0497-4. PubMed PMID: 32541883.
Ma JK, West CR, Martin Ginis KA. The effects of a patient and provider co-developed, behavioral physical activity intervention on physical activity, psychosocial predictors, and fitness in individuals with spinal cord injury: a randomized controlled trial. Sports Med. 2019;49:1117–31. https://doi.org/10.1007/s40279-019-01118-5. Epub 2019/05/24; PubMed PMID 31119717.
Ma JK, Cheifetz O, Todd KR, Chebaro C, Phang SH, Shaw RB, et al. Co-development of a physiotherapist-delivered physical activity intervention for adults with spinal cord injury. Spinal Cord. 2020;58:778–86. https://doi.org/10.1038/s41393-020-0422-x. Epub 2020/01/24; PubMed PMID: 31969687.
Lai B, Rimmer J, Barstow B, Jovanov E, Bickel CS. Teleexercise for persons with spinal cord injury: a mixed-methods feasibility case series. JMIR Rehabil Assist Technol. 2016;3:e8. https://doi.org/10.2196/rehab.5524. Epub 2017/06/06; PubMed PMID: 28582252; PubMed Central PMCID: PMC5454561.
Chemtob K, Rocchi M, Arbour-Nicitopoulos K, Kairy D, Fillion B, Sweet SN. Using tele-health to enhance motivation, leisure time physical activity, and quality of life in adults with spinal cord injury: A self-determination theory-based pilot randomized control trial. Psychol Sport Exerc. 2019;43:243–52. https://doi.org/10.1016/j.psychsport.2019.03.008
Rocchi MA, Robichaud Lapointe T, Gainforth HL, Chemtob K, Arbour-Nicitopoulos KP, Kairy D, et al. Delivering a tele-health intervention promoting motivation and leisure-time physical activity among adults with spinal cord injury: an implementation evaluation. Sport, Exercise, and Performance Psychology. 2020. https://doi.org/10.1037/spy0000207.
Allin S, Shepherd J, Thorson T, Tomasone J, Munce S, Linassi G, et al. Web-Based Health Coaching for Spinal Cord Injury: results from a mixed methods feasibility evaluation. JMIR Rehabilitation Assistive Technol. 2020;7:e16351. https://doi.org/10.2196/16351.
Pancer M, Manganaro M, Pace I, Marion P, Gagnon DH, Laramee MT, et al. A web-based physical activity portal for individuals living with a spinal cord injury: qualitative study. JMIR Form Res. 2019;3:e12507. https://doi.org/10.2196/12507. Epub 2019/07/28; PubMed PMID: 31350835.
Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–34. https://doi.org/10.1249/mss.0b013e3180616b27. Epub 2007/09/01; PubMed PMID: 17762377.
Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. Journal of the American Medical Association JAMA. 2018. https://doi.org/10.1001/jama.2018.14854.
Goosey-Tolfrey VL, van der Scheer JW, Lexell J, Clements K, Martin Ginis KA. International SCIEGPG. Development of scientific exercise guidelines for adults with spinal cord injury. Br J Sports Med. 2018;52:1166–7. https://doi.org/10.1136/bjsports-2018-099202. Epub 2018/04/27; PubMed PMID: 29695510.
Martin Ginis KA, Hicks AL, Latimer AE, Warburton DE, Bourne C, Ditor DS, et al. The development of evidence-informed physical activity guidelines for adults with spinal cord injury. Spinal Cord. 2011;49:1088–96.
Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, Barrow A, Bourne C, Carruthers P, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord. 2018;56:308–21. https://doi.org/10.1038/s41393-017-0017-3. Epub 2017/10/27; PubMed PMID: 29070812.
Centers for Disease Control and Prevention. 2007 Behavioral Risk Factor Surveillance System Questionnaire. 2007.
Bandura A Social foundations of thought and action: Social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986.
Marlatt GA, Gordon JR. Relapse prevention. Warm Beach, Washington: The Guilford Press; 1985.
Froehlich-Grobe K, Lee J, Aaronson LS, Nary DE, Washburn RA, Little TD. Exercise for everyone: a randomized controlled trial of Project Workout On Wheels in promoting exercise among wheelchair users. Arch Phys Med Rehabil. 2014;95:20–8. https://doi.org/10.1016/j.apmr.2013.07.006.
Cole M, Froehlich-Grobe K, Driver S, Shegog R, McLaughlin J. Website Redesign of a 16-week exercise intervention for people with spinal cord injury by using participatory action research. JMIR Rehabil Assist Technol. 2019;6:e13441. https://doi.org/10.2196/13441.
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Saebu M, Sorensen M. Factors associated with physical activity among young adults with a disability. Scand J Med Sci Sports. 2011;21:730–8. https://doi.org/10.1111/j.1600-0838.2010.01097.x. Epub 2010/05/13; PubMed PMID: 20459465.
Bombardier CH, Fann JR, Tate DG, Richards JS, Wilson CS, Warren AM, et al. An exploration of modifiable risk factors for depression after spinal cord injury: which factors should we target? Arch Phys Med Rehabil. 2012;93:775-81. Epub 2012/03/24. https://doi.org/10.1016/j.apmr.2011.12.020. PubMed PMID: 22440484.
IPAQ Core Group. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ) - Short and Long Forms 2005 [cited 2020 October]. Available from: www.ipaq.ki.se.
Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med. 1970;2:92–8.
American College of Sports Medicine. ACSM’s exercise testing and prescription (10th Edition). 10th ed. Madeline P, Bayles AMS, editor. Philadelphia, PA: Wolters Kluwer; 2017.
Becker H, Stuifenbergen A, Oh HS, Hall S. Self-rated abilities for health practices: a health self-efficacy measure. Health Values. 1993;17:42–50.
Becker H, Stuifbergen AK, Sands D. Development of a scale to measure barriers to health promotion activities among persons with disabilities. Am J Health Promot. 1991;5:449–54.
Snyder CR, Sympson SC, Ybasco FC, Borders TF, Babyak MA, Higgins RL. Development and validation of the state hope scale. J Pers Soc Psychol. 1996;70:321–35.
Kennedy P, Evans M, Sandhu N. Psychological adjustment to spinal cord injury: the contribution of coping, hope and cognitive appraisals. Psychol Health Med. 2009;14:17–33. https://doi.org/10.1080/13548500802001801. Epub 2008/12/17; PubMed PMID: 19085309.
Kortte KB, Stevenson JE, Hosey MM, Castillo R, Wegener ST. Hope predicts positive functional role outcomes in acute rehabilitation populations. Rehabil Psychol. 2012;57:248–55. https://doi.org/10.1037/a0029004. Epub 2012/09/06; PubMed PMID: 22946612.
Martz E, Livneh H. Psychosocial adaptation to disability within the context of positive psychology: findings from the literature. J Occup Rehabil. 2016;26:4–12. https://doi.org/10.1007/s10926-015-9598-x. Epub 2015/08/19; PubMed PMID: 26283187.
Ginis KA, Latimer AE, Hicks AL, Craven BC. Development and evaluation of an activity measure for people with spinal cord injury. Med Sci Sports Exerc. 2005;37:1099–111.
Latimer AE, Ginis K, Craven BC, Hicks AL. The physical activity recall assessment for people with spinal cord injury: validity. Med Sci Sports Exerc. 2006;38:208–16.
Janssen TW, van Oers CA, Veeger HE, Hollander AP, van der Woude LH, Rozendal RH. Relationship between physical strain during standardised ADL tasks and physical capacity in men with spinal cord injuries. Paraplegia. 1994;32:844–59. https://doi.org/10.1038/sc.1994.131. Epub 1994/12/01; PubMed PMID: 7708424.
Acknowledgements
The authors would like to thank the individuals who served as focus group members to provide input and guidance in developing the WOWii website and the initial pilot participants who provided important information in shaping the program plus everyone who participated in the WOWii trial. Their time and input were invaluable to our team and we enjoyed getting to know each one of them. The team would also like to acknowledge early study coordinators, Maria Cole, MPH, MSW and Danielle Carlton, MPH who helped launch the study. The content of this paper was developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR; grant number 90IF0091). NIDILRR is a center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS).
Funding
The content of this paper was developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90IF0091). NIDILRR is a center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The content of this paper does not necessarily represent the policy of NIDILRR, ACL, and HHS, and is not endorsed by the Federal Government. The content of this paper was developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR; grant number 90IF0091). NIDILRR is a center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The content of this paper does not necessarily represent the policy of NIDILRR, ACL, and HHS, and is not endorsed by the Federal Government.
Author information
Authors and Affiliations
Contributions
KFG: conceptualized the study design, developed the first full draft of the manuscript. JL: assisted with study conceptualization, conducted all analyses, and wrote the analyses and power sections plus substantially edited text for the results section. CO: assisted with data management, cleaning, and editing various rounds of drafts of the manuscript. AL: assisted with intervention delivery, data entry, Polar data abstraction, plus conducting literature reviews and summarizing new evidence, plus conducting literature reviews and summarizing new evidence. ES: assisted with intervention delivery, data entry, plus analyzing satisfaction data and drafting the text regarding participants satisfaction with the study. SD: assisted with study conceptualization, data interpretation, plus provided substantial contribution to the writing and editing the manuscript drafts. RS: assisted with study conceptualization, data analyses and interpretation, plus provided substantial contribution to the writing and editing the manuscript drafts. SJL: conducted all lab-based testing for fitness measures and weight plus assisted with interpreting results and writing results for the physiologic testing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Froehlich-Grobe, K., Lee, J., Ochoa, C. et al. Effectiveness and feasibility of the workout on wheels internet intervention (WOWii) for individuals with spinal cord injury: a randomized controlled trial. Spinal Cord 60, 862–874 (2022). https://doi.org/10.1038/s41393-022-00787-w
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41393-022-00787-w
This article is cited by
-
Qualitative analysis of perceived motivators and barriers to exercise in individuals with spinal cord injury enrolled in an exercise study
Spinal Cord Series and Cases (2022)