Abstract
Study design
Observational study.
Objectives
To examine the feasibility of meeting the current clinical guidelines for the hemodynamic management of acute spinal cord injury (SCI) which recommend maintaining mean arterial pressure (MAP) at 85–90 mmHg in the days following injury.
Methods
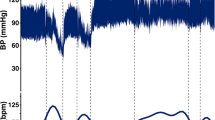
This study examined data collected minute-by-minute to describe the pressure profile in the first 5 days following SCI in 16 patients admitted to the Intensive Care Unit at Vancouver General Hospital (40 ± 19 years, 13 M/3 F, C4-T11). MAP and intrathecal pressure (ITP) were monitored at 100 Hz by arterial and lumbar intrathecal catheters, respectively, and reported as the average of each minute. Spinal cord perfusion pressure was calculated as the difference between MAP and ITP. The minute-to-minute difference (MMdiff) of each pressure variable was calculated as the absolute difference between consecutive minutes.
Results
Only 24 ± 7% of MAP recordings were between 85 and 90 mmHg. Average MAP MMdiff was ~3 mmHg. The percentage of MAP recordings within target range was negatively correlated with the degree of variability (i.e. MMdiff; r = −0.64, p < 0.008) whereas higher mean MAP was correlated with greater variability (r = 0.57, p = 0.021).
Conclusions
Our findings point to the ‘real life’ challenges in maintaining MAP in acute SCI patients. Given MAP fluctuated ~3 mmHg minute-to-minute, maintaining MAP within a 5 mmHg range with conventional volume replacement and vasopressors presents an almost impossible task for clinicians and warrants reconsideration of current management guidelines.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ahuja CS, Wilson JR, Nori S, Kotter MRN, Druschel C, Curt A, et al. Traumatic spinal cord injury. Nat Rev Dis Prim. 2017;3. https://doi.org/10.1038/nrdp.2017.18.
Tator CH, Fehlings MG. Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg. 1991;75:15–26.
Lehmann KG, Lane JG, Piepmeier JM, Batsford WP. Cardiovascular abnormalities accompanying acute spinal cord injury in humans: Incidence, time course and severity. J Am Coll Cardiol. 1987;10:46–52.
Wallace MC, Tator CH, Frazee P. Relationship between posttraumatic ischemia and hemorrhage in the injured rat spinal cord as shown by colloidal carbon angiography. Neurosurgery. 1986;18:433–9.
Dakson A, Brandman D, Thibault-Halman G, Christie SD. Optimization of the mean arterial pressure and timing of surgical decompression in traumatic spinal cord injury: a retrospective study. Spinal Cord. 2017;55:1033–8.
Cohn JA, Wright J, Mckenna SL, Bushnik T. Impact of mean arterial blood pressure during the first seven days post spinal cord injury. Top Spinal Cord Inj Rehabil. 2010;15:96–106.
Early acute management in adults with spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2008;31:403–79.
Ryken TC, Hurlbert RJ, Hadley MN, Aarabi B, Dhall SS, Gelb DE, et al. The acute cardiopulmonary management of patients with cervical spinal cord injuries. Neurosurgery. 2013;72:84–92.
Walters BC, Hadley MN, Hurlbert RJ, Aarabi B, Dhall SS, Gelb DE, et al. Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update. Neurosurgery. 2013;60:82–91.
Evaniew N, Mazlouman SJ, Belley-Côté EP, Jacobs WB, Kwon BK. Interventions to optimize spinal cord perfusion in patients with acute traumatic spinal cord injuries: a systematic review. J Neurotrauma. 2020;37:1127–39.
Kong CY, Hosseini AM, Belanger LM, Ronco JJ, Paquette SJ, Boyd MC, et al. A prospective evaluation of hemodynamic management in acute spinal cord injury patients. Spinal Cord. 2013;51:466–71.
Tee JW, Altaf F, Belanger L, Ailon T, Street J, Paquette S, et al. Mean arterial blood pressure management of acute traumatic spinal cord injured patients during the pre-hospital and early admission period. J Neurotrauma. 2017;34:1271–7.
Squair JW, Bélanger LM, Tsang A, Ritchie L, Mac-Thiong JM, Parent S, et al. Spinal cord perfusion pressure predicts neurologic recovery in acute spinal cord injury. Neurology. 2017;89:1660–7.
Squair JW, Bélanger LM, Tsang A, Ritchie L, Mac-Thiong JM, Parent S, et al. Empirical targets for acute hemodynamic management of individuals with spinal cord injury. Neurology. 2019;93:e1205–11.
Hawryluk G, Whetstone W, Saigal R, Ferguson A, Talbott J, Bresnahan J, et al. Mean arterial blood pressure correlates with neurological recovery after human spinal cord injury: analysis of high frequency physiologic data. J Neurotrauma. 2015;32:1958–67.
Ryken TC, Hurlbert RJ, Hadley MN, Aarabi B, Dhall SS, Gelb DE, et al. The acute cardiopulmonary management of patients with cervical spinal cord injuries. Neurosurgery. 2013;72:84–92.
Squair JW, Bélanger LM, Tsang A, Ritchie L, Mac-Thiong JM, Parent S, et al. Empirical targets for acute hemodynamic management of individuals with spinal cord injury. Neurology. 2019;93:E1205–11.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
Squair JW, Gautier M, Mahe L, Soriano JE, Rowald A, Bichat A, et al. Neuroprosthetic baroreflex controls haemodynamics after spinal cord injury. Nature. 2021;590:308–14.
Phillips AA, Squair JW, Sayenko DG, Edgerton VR, Gerasimenko Y, Krassioukov AV. An autonomic neuroprosthesis: noninvasive electrical spinal cord stimulation restores autonomic cardiovascular function in individuals with spinal cord injury. J Neurotrauma. 2018;35:446–51.
Sachdeva R, Nightingale TE, Pawar K, Kalimullina T, Mesa A, Marwaha A, et al. Noninvasive neuroprosthesis promotes cardiovascular recovery after spinal cord injury. Neurotherapeutics. 2021;1:3.
Parati G, Ochoa JE, Lombardi C, Bilo G. Assessment and management of blood-pressure variability. Nat Rev Cardiol. 2013;10:143–55.
Dawson SL, Manktelow BN, Robinson TG, Panerai RB, Potter JF. Which parameters of beat-to-beat blood pressure and variability best predict early outcome after acute ischemic stroke? Stroke. 2000;31:463–8.
Narkiewicz K, Winnicki M, Schroeder K, Phillips BG, Kato M, Cwalina E, et al. Relationship between muscle sympathetic nerve activity and diurnal blood pressure profile. Hypertension. 2002;39:168–72.
Weaver LC, Fleming JC, Mathias CJ, Krassioukov AV. Disordered cardiovascular control after spinal cord injury. Handb Clin Neurol. 2012;109:213–33.
Parati G, Mancia G, Di Rienzo M, Castiglioni P, Taylor JA, Studinger P. Point:counterpoint: cardiovascular variability is/is not an index of autonomic control of circulation. J Appl Physiol. 2006;101:676–82.
Martirosyan NL, Kalani MYS, Bichard WD, Baaj AA, Fernando Gonzalez L, Preul MC, et al. Cerebrospinal fluid drainage and induced hypertension improve spinal cord perfusion after acute spinal cord injury in pigs. Neurosurgery. 2015;76:461–8.
Shiraishi M, Kamo T, Nemoto S, Narita M, Kamegai M, Baevsky RM, et al. Blood pressure variability during 120-day head-down bed rest in humans. Biomed Pharmacother. 2003;57:35–8.
Seo WS, Oh HS. The circadian rhythms of blood pressure and heart rate in the hypertensive subjects: dippers and non-dippers. Yonsei Med J. 2002;43:320–8.
Hubli M, Gee CM, Krassioukov AV. Refined assessment of blood pressure instability after spinal cord injury. Am J Hypertens. 2015;28:173–81.
Streijger F, So K, Manouchehri N, Tigchelaar S, Lee JHT, Okon EB, et al. Changes in pressure, hemodynamics, and metabolism within the spinal cord during the first 7 days after injury using a Porcine model. J Neurotrauma. 2017;34:3336–50.
Acknowledgements
The authors would like to acknowledge the support of our funders—Praxis Spinal Cord Institute, Vancouver Coastal Health Research Institute and Michael Smith Foundation for Health Research—for their support. We thank the patients and their families for providing consent to our data collection that formed the present paper.
Funding
Funding for this clinical trial was primarily received from Praxis Spinal Cord Institute (formerly the Rick Hansen Institute). Additional funds were received from the Vancouver Coastal Health Research Institute and Michael Smith Foundation for Health Research. BKK is the Canada Research Chair in SCI.
Author information
Authors and Affiliations
Contributions
CMG analysed data, interpreted results, and drafted the paper for important intellectual content. AT, LMB, LR, TA, SP, RCM, ND, JS, CGF, and MCF collected data and revised the manuscript for important intellectual content. BKK conceived of and designed the work that led to the submission, interpreted results, and revised the paper for important intellectual content. All authors approved the final version and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. Ethics approval was received from the University of British Columbia Clinical Research Ethics Board.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gee, C.M., Tsang, A., Bélanger, L.M. et al. All over the MAP: describing pressure variability in acute spinal cord injury. Spinal Cord 60, 470–475 (2022). https://doi.org/10.1038/s41393-022-00802-0
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41393-022-00802-0
This article is cited by
-
Critical Care of Spinal Cord Injury
Current Neurology and Neuroscience Reports (2024)
-
Invasive devices to monitor the intraspinal perfusion pressure in the hemodynamic management of acute spinal cord injury: A systematic scoping review
Acta Neurochirurgica (2024)