Abstract
Study design
Cross-sectional study.
Objective
To elucidate the association between age and incidence of deep vein thrombosis (DVT) in patients with spinal cord injury (SCI).
Setting
Rehabilitation Medicine Department of the First Affiliated Hospital of China University of Science and Technology.
Methods
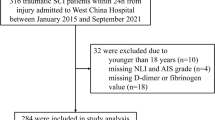
Patients from August 2018 to December 2020 with SCI (N = 260) were tertiles divided the age into three groups to analyze the association between age and incidence of DVT.
Results
American Spinal Cord Injury Association impairment scale (AIS), urinary tract infection (UTI), pulmonary infection (PI), and anticoagulation therapy (AT) were confounders for the association between age and incidence of DVT. The incidence of DVT increased by 1.07-fold (Non-adjusted model, OR = 1.07, P < 0.001), 1.05-fold (Minimally-adjusted model: adjusted for confounders, OR = 1.05, P = 0.010) and 1.06-fold [Fully-adjusted model: adjusted for confounders and unbalanced probable variables: AIS, UTI, PI, AT, Sex, D-dimer(new), Fibrinogen (new), Modes of injury and Level of injury, OR = 1.06, P = 0.012] when age increased by 1 year. The incidence of DVT had an increasing trend with age in different age tertile in the three models (P for trend <0.05). Age had a linearly association with incidence of DVT (OR = 1.07, P = 0.065) and stable in different subgroups, for lower age, the association was also linearly (OR = 4.40, P = 1.000), for middle (fold point = 46.46, P < 0.001) and higher age (fold point = 66, P = 0.017), the association was curvilinear.
Conclusion
Age had a linearly association with incidence of DVT. Quitting smoking, preventing/treating UTI and AT should be adopted in advance for patients with SCI for all age, especially for older.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Chopard R, Albertsen IE, Piazza G. Diagnosis and treatment of lower extremity venous thromboembolism: a review. JAMA. 2020;324:1765–76.
Lau D, Dalle Ore CL, Tarapore PE, Huang M, Manley G, Singh V, et al. Value of aggressive surgical and intensive care unit in elderly patients with traumatic spinal cord injury. Neurosurg Focus. 2019;46:E3.
Hon B, Botticello A, Kirshblum S. Duplex ultrasound surveillance for deep vein thrombosis after acute traumatic spinal cord injury at rehabilitation admission. J Spinal Cord Med. 2020;43:298–305.
Piran S, Schulman S. Incidence and risk factors for venous thromboembolism in patients with acute spinal cord injury: a retrospective study. Thromb Res. 2016;147:97–101.
Yamada K, Suda K, Matsumoto Harmon S, Komatsu M, Ushiku C, Takahata M, et al. Rapidly progressive cervical myelopathy had a high risk of developing deep venous thrombosis: a prospective observational study in 289 cases with degenerative cervical spine disease. Spinal Cord. 2019;57:58–64.
De la Garza Ramos R, Goodwin CR, Abu-Bonsrah N, Jain A, Miller EK, Huang N, et al. Patient and operative factors associated with complications following adolescent idiopathic scoliosis surgery: an analysis of 36,335 patients from the Nationwide Inpatient Sample. J Neurosurg Pediatr. 2016;25:730–6.
Kim JH. Multicollinearity and misleading statistical results. Korean J Anesthesiol. 2019;72:558–69.
Ernst M, Hartz A. Phenylpropanolamine and hemorrhagic stroke. N Engl J Med. 2001;344:1094.
Jaddoe V, de Jonge L, Hofman A, Franco O, Steegers E, Gaillard R. First trimester fetal growth restriction and cardiovascular risk factors in school age children: population based cohort study. BMJ. 2014;348:1–11.
Vetter C, Devore E, Wegrzyn L, Massa J, Speizer F, Kawachi I, et al. Association Between Rotating Night Shift Work and Risk of Coronary Heart Disease Among Women. JAMA. 2016;315:1726–34.
Liu JM, Lan M, Zhou Y, Chen XY, Huang SH, Liu ZL. Serum concentrations of fibrinogen in patients with spinal cord injury and its relationship with neurologic function. World Neurosurg. 2017;106:219–23.
Bozic M, Teran N, Peterlin B, Stegnar M. Fibrinogen polymorphisms TaqI, HaeIII and BclI are not associated with a higher risk of deep vein thrombosis. Pathophysiol Haemost Thromb. 2003;33:164–9.
Crippa L, Ravasi F, D’Angelo SV, Varagona R, Milani E, Safa O, et al. Diagnostic value of compression ultrasonography and fibrinogen-related parameters for the detection of postoperative deep vein thrombosis following elective hip replacement: a pilot study. Thromb Haemost. 1995;74:1235–9.
McLvor J, Anderson DR, Britt RP, Dovey P. Comparison of 125I-labelled fibrinogen uptake and venography in the detection of recent deep-vein thrombosis in the legs. Br J Radiol. 1975;48:1013–8.
Wu J, Qing J, Yao Y, Chen D, Jiang Q. Performance of age-adjusted D-dimer values for predicting DVT before the knee and hip arthroplasty. J Orthop Surg Res. 2021;16:82.
Mackiewicz-Milewska M, Cisowska-Adamiak M, Pyskir J, Świątkiewicz I. Usefulness of D-dimer and ultrasonography screening for detecting deep vein thrombosis in patients with spinal cord injury undergoing rehabilitation. J Clin Med. 2021;10:689.
Wang ZM, Zou P, Yang JS, Liu TT, Song LL, Lu Y, et al. Epidemiological characteristics of spinal cord injury in Northwest China: a single hospital-based study. J Orthop Surg Res. 2020;15:214.
Ma J, Du P, Qin J, Zhou Y, Liang N, Hu J, et al. Incidence and risk factors predicting deep venous thrombosis of lower extremity following spinal fractures. Sci Rep. 2021;11:2441.
Yu X, Liu W, Zhang HW. [Analysis of related factors of deep venous thrombosis after spinal cord injury]. Zhongguo Gu Shang. 2020;33:140–3.
Teter K, Schrem E, Ranganath N, Adelman M, Berger J, Sussman R, et al. Presentation and management of inferior vena cava thrombosis. Ann Vasc Surg. 2019;56:17–23.
Gregson J, Kaptoge S, Bolton T, Pennells L, Willeit P, Burgess S, et al. Cardiovascular risk factors associated with venous thromboembolism. JAMA Cardiol. 2019;4:163–73.
Özcan M, Erem M, Turan FN. Symptomatic deep vein thrombosis following elective knee arthroscopy over the age of 40. Clin Appl Thromb Hemost. 2019;25:1–6.
Larsson SC, Mason AM, Bäck M, Klarin D, Damrauer SM, Michaëlsson K, et al. Genetic predisposition to smoking in relation to 14 cardiovascular diseases. Eur Heart J. 2020;41:3304–10.
Al-Nasser B. Influence of tobacco smoking on perioperative risk of venous thromboembolism. Turkish J Anaesthesiol Reanim. 2020;48:11–6.
Cichos KH, Lehtonen EJ, McGwin G Jr., Ponce BA, Ghanem ES. Inhospital complications of patients with neuromuscular disorders undergoing total joint arthroplasty. J Am Acad Orthop Surg. 2019;27:e535–43.
Geerlings SE. Clinical presentations and epidemiology of urinary tract infections. Microbiol Spectr. 2016;4:1–11.
Hu HZ, Granger N, Jeffery ND. Pathophysiology, clinical importance, and management of neurogenic lower urinary tract dysfunction caused by suprasacral spinal cord injury. J Vet Intern Med. 2016;30:1575–88.
Grimnes G, Isaksen T, Tichelaar Y, Brækkan SK, Hansen JB. Acute infection as a trigger for incident venous thromboembolism: Results from a population-based case-crossover study. Res Pract Thromb Haemost. 2018;2:85–92.
Acknowledgements
We would like to thank Tingting Zhang, CuicuiChang, Tingting Bao, Nanzu Chengjiang, Liai Sun, and Lina Ma for collecting the data. We would also like to thank Xinglin Chen for helping us analyze the data and thanks to Editage (www.editage.com) for editing the English.
Author information
Authors and Affiliations
Contributions
JLZ: Conducted the study and wrote the draft. YYF: Designed the study, interpreted the data, and edited the manuscript. HYP, YT, JZ, and SSZ: Collected the data. CW: Planned the project, created, and statistical analyzed the data. The authors all read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Informed consent was waived due to the nature of the retrospective study, which consistent with ethical requirements and waiver from the Ethics Committee of First Affiliated Hospital of the University of Science and Technology of China (Anhui Provincial Hospital), this study also approved by the committee, the approved number was 2020-RE-008.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhang, J., Fang, Y., Pang, H. et al. Association between age and incidence of deep vein thrombosis in patients with spinal cord injury: an observational cross-sectional study. Spinal Cord 60, 1006–1013 (2022). https://doi.org/10.1038/s41393-022-00814-w
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41393-022-00814-w
This article is cited by
-
Analysis of risk factors for lower deep vein thrombosis (DVT) in patients over 60 years of age after total hip arthroplasty
BMC Musculoskeletal Disorders (2025)
-
Associations of RBC counts and incidence of DVT in patients with spinal cord injury: a five year observational retrospective study
Journal of Orthopaedic Surgery and Research (2024)
-
Distribution characteristics of perioperative deep vein thrombosis (DVT) and risk factors of postoperative DVT exacerbation in patients with thoracolumbar fractures caused by high-energy injuries
European Journal of Trauma and Emergency Surgery (2024)