Abstract
Study design
Retrospective review.
Objectives
While most individuals with spinal cord injury (SCI) are expected to have 1-2 urinary tract infections (UTIs) per year, there is a subset with higher incidence. We evaluate our practice to characterize common causes of recurrent UTIs, hypothesizing that more frequent infections typically have addressable risk factors.
Setting
Tertiary urology clinic, San Jose, CA.
Methods
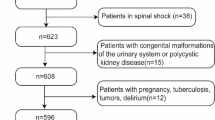
We reviewed patients with SCI referred to a tertiary urology clinic for evaluation and management of “recurrent UTIs” during the years 2015–2020. Following workup, the suspected cause of recurrent UTIs and number of post-specialty evaluation UTIs (patient reported) were noted.
Results
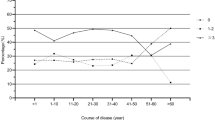
Forty persons with SCI with a mean of 4.8 UTI treatments in the prior year comprised our cohort with most performing CIC (80%). After workup, 37/40 (92.5%) had a likely cause for their reported recurrent UTIs. In 16/40 (40%), careful questioning determined that the patient was not having UTIs based on guideline definitions. In those with confirmed recurrent UTIs, a bladder diary (62.5%) or urodynamic study (64%) was more likely to identify a cause compared to imaging (2.6%) or cystoscopy (8%). With a minimum 1-year follow-up, 90% of our population had a 50% or more reduction in UTI incidence, mostly using non-antibiotic strategies.
Conclusion
In a referral SCI population with a chief complaint of “recurrent UTIs”, over a third were not having UTIs. In addition to detailed history, a bladder diary +/− urodynamics are most useful in finding the cause and improving UTI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during this study are available from the corresponding author on reasonable request.
References
Elliott CS, Dallas KB, Zlatev D, Comiter CV, Crew J, Shem K. Volitional Voiding of the Bladder after Spinal Cord Injury: Validation of Bilateral Lower Extremity Motor Function as a Key Predictor. J Urol. 2018;200:154–60.
Pavese C, Schneider MP, Schubert M, Curt A, Scivoletto G, Finazzi-Agrò E, et al. Prediction of Bladder Outcomes after Traumatic Spinal Cord Injury: A Longitudinal Cohort Study. PLoS Med. 2016;13:e1002041.
Ginsberg DA, Boone TB, Cameron AP, Gousse A, Kaufman MR, Keays E, et al. The AUA/SUFU Guideline on Adult Neurogenic Lower Urinary Tract Dysfunction: Diagnosis and Evaluation. J Urol. 2021;206:1097–105.
Watanabe T, Rivas DA, Chancellor MB. Urodynamics of spinal cord injury. Urologic Clin North Am. 1996;23:459–73.
Simpson LA, Eng JJ, Hsieh JT, Wolfe DL. The health and life priorities of individuals with spinal cord injury: a systematic review. J Neurotrauma. 2012;29:1548–55.
Crescenze IM, Myers JB, Lenherr SM, Elliott SP, Welk B, Mph DO, et al. Predictors of low urinary quality of life in spinal cord injury patients on clean intermittent catheterization. Neurourol Urodyn. 2019;38:1332–8.
Theisen KM, Mann R, Roth JD, Pariser JJ, Stoffel JT, Lenherr SM, et al. Frequency of patient-reported UTIs is associated with poor quality of life after spinal cord injury: a prospective observational study. Spinal Cord. 2020;58:1274–81.
Welk B, Lenherr S, Santiago-Lastra Y, Norman HS, Keiser MG, Elliott CS. Differences in the incidence of urinary tract infections between neurogenic and non-neurogenic bladder dysfunction individuals performing intermittent catheterization. Neurourol Urodyn. 2022;41:1002–11.
Manack A, Motsko SP, Haag-Molkenteller C, Dmochowski RR, Goehring EL Jr, Nguyen-Khoa BA, et al. Epidemiology and healthcare utilization of neurogenic bladder patients in a US claims database. Neurourol Urodyn. 2011;30:395–401.
Dinh A, Hallouin-Bernard MC, Davido B, Lemaignen A, Bouchand F, Duran C, et al. Weekly Sequential Antibioprophylaxis for Recurrent Urinary Tract Infections Among Patients With Neurogenic Bladder: A Randomized Controlled Trial. Clin Infect Dis Off Publ Infect Dis Soc Am. 2020;71:3128–35.
Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis Off Publ Infect Dis Soc Am. 2010;50:625–63.
Wyndaele JJ. Normality in urodynamics studied in healthy adults. J Urol. 1999;161:899–902.
Rosier P, Schaefer W, Lose G, Goldman HB, Guralnick M, Eustice S, et al. International Continence Society Good Urodynamic Practices and Terms 2016: Urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol Urodyn. 2017;36:1243–60.
Stoffel JT. Detrusor sphincter dyssynergia: a review of physiology, diagnosis, and treatment strategies. Transl Androl Urol. 2016;5:127–35.
Weld KJ, Graney MJ, Dmochowski RR. Differences in bladder compliance with time and associations of bladder management with compliance in spinal cord injured patients. J Urol. 2000;163:1228–33.
Nicolle LE. The chronic indwelling catheter and urinary infection in long-term-care facility residents. Infect Control Hospital Epidemiol. 2001;22:316–21.
Bakke A, Vollset SE. Risk factors for bacteriuria and clinical urinary tract infection in patients treated with clean intermittent catheterization. J Urol. 1993;149:527–31.
Merritt JL, Erickson RP, Opitz JL. Bacteriuria during follow-up in patients with spinal cord injury: II Efficacy of antimicrobial suppressants. Arch Phys Med Rehabilit. 1982;63:413–5.
Nemetalla M, Frazer K. Antibiotic Prophylaxis for UTIs in Patients with Neurogenic Bladder. Am Fam physician. 2019;99:186.
Sauerwein D. Urinary tract infection in patients with neurogenic bladder dysfunction. Int J Antimicrobial Agents. 2002;19:592–7.
Lapides J. Role of hydrostatic pressure and distensin in urinary tract infection. Philadelphia: FA Davis Co; 1965.
Lee BB, Haran MJ, Hunt LM, Simpson JM, Marial O, Rutkowski SB, et al. Spinal-injured neuropathic bladder antisepsis (SINBA) trial. Spinal Cord. 2007;45:542–50.
Acknowledgements
The authors whose names are listed above certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or nonfinancial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript. As this was a retrospective study (IRB #20-012ER, Santa Clara Valley Medical Center), a clinical trial registration is not applicable.
Author information
Authors and Affiliations
Contributions
CSE – study design, data analysis, manuscript writing and editing. HKH – data analysis, manuscript writing and editing. KS – study design, data analysis, manuscript writing and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Ethics approval via IRB approval Santa Clara Valley Medical Center, San Jose, CA # 20-012ER. All methods were performed in accordance with relevant guidelines and regulations. No patient consent was obtained on this retrospective study. There is no material from other sources.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Elliott, C.S., Huynh, HK. & Shem, K. Diagnostic evaluation and management of recurrent urinary tract infections in the spinal cord injury population – a retrospective evaluation at a tertiary care center. Spinal Cord 63, 181–186 (2025). https://doi.org/10.1038/s41393-024-01037-x
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41393-024-01037-x