Abstract
Study design
Retrospective cohort study.
Objectives
To evaluate surgical consistency and clinical outcomes in intramedullary ependymoma (WHO grade II) cases by using X-bar charts as a tool to assess procedural stability.
Setting
The single institution in Japan.
Methods
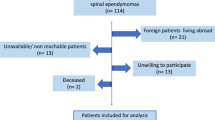
This study included patients who underwent resection of intramedullary ependymomas between 2001 and 2023. All surgeries were performed by one of five board-certified spine surgeons. Operative time was analyzed for stability using X-bar charts. Neurological outcomes were assessed using the modified McCormick Scale (mMS), and regression analysis was performed to evaluate the relationship between operative time and mMS.
Results
The study included 144 patients (82 men, 62 women; average age 50.3 ± 14.6 years). Tumors were located at cervical (67.4%) or thoracic (32.6%) levels, averaging 3.0 ± 1.2 vertebrae. The surgeon who performed 71 cases was defined as the experienced surgeon, and the other surgeons performed 10–24 cases, respectively. The mean operative time was 380.6 ± 140.7 min, and 135 cases achieved gross total resection. The average follow-up duration was 6.9 ± 3.9 years. X-bar charts showed surgical stability once the average number of cases exceeded 17. No significant correlation was found between operative time and mMS for any surgeon. Perioperative complications were minimal.
Conclusions
X-bar charts are a valuable tool for objectively evaluating surgical stability. In intramedullary ependymoma surgeries, consistency in operative time was achieved after 17 cases, and longer procedures did not adversely affect neurological outcomes. This method could be extended to monitor procedural reliability in other complex surgical interventions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Nakamura M, Ishii K, Watanabe K, Tsuji T, Takaishi H, Matsumoto M et al. Surgical treatment of intramedullary spinal cord tumors: prognosis and complications. Spinal Cord. 2008;46:282–6.
Tsuji O, Nagoshi N, Ishii R, Nori S, Suzuki S, Okada E et al. Poor prognostic factors for surgical treatment of spinal intramedullary ependymoma (World Health Organization Grade II). Asian Spine J. 2020;14:821–8.
Naito K, Umebayashi D, Kurokawa R, Endo T, Mizuno M, Hoshimaru M et al. Predictors of progression-free survival in patients with spinal intramedullary ependymoma: a Multicenter Retrospective Study by the Neurospinal Society of Japan. Neurosurgery. 2023;93:1046–56.
Svoboda N, Bradac O, de Lacy P, Benes V. Intramedullary ependymoma: long-term outcome after surgery. Acta Neurochir. 2018;160:439–47.
Kouo T, Kleinman K, Fujii-Rios H, Badaki-Makun O, Kim J, Falco L et al. A resident-led QI initiative to improve pediatric emergency department boarding times. Pediatrics. 2020;145:e20191477.
Uspal NG, Rutman LE, Kodish I, Moore A, Migita RT. Use of a dedicated, non-physician-led mental health team to reduce pediatric emergency department lengths of stay. Acad Emerg Med. 2016;23:440–7.
McCormick PC, Stein BM. Intramedullary tumors in adults. Neurosurg Clin N Am. 1990;1:609–30.
Hair J, Black W, Babin B, Anderson R Multivariate data analysis. 7th edition. Pearson Educational International; 2010.
Jacob KC, Patel MR, Prabhu MC, Vanjani NN, Pawlowski H, Munim MA et al. Lateral lumbar interbody fusion: single surgeon learning curve. World Neurosurg. 2022;164:e411–e419.
Rong LM, Xie PG, Shi DH, Dong JW, Liu B, Feng F et al. Spinal surgeons’ learning curve for lumbar microendoscopic discectomy: a Prospective Study of our first 50 and latest 10 cases. Chin Med J. 2008;121:2148–51.
Okubo T, Nagoshi N, Kono H, Kobayashi Y, Tsuji O, Aoyama R et al. Comparison of surgical outcomes after posterior decompression by junior or senior surgeons for patients with cervical ossification of the posterior longitudinal ligament: results from Retrospective Multicenter Cohort Study. Glob Spine J. 2024;15:1703–11.
Nagoshi N, Iwanami A, Isogai N, Ishikawa M, Nojiri K, Tsuji T et al. Does posterior cervical decompression conducted by junior surgeons affect clinical outcomes in the treatment of cervical spondylotic myelopathy? results from a Multicenter Study. Glob Spine J. 2019;9:25–31.
Benmansour M, Malti A, Jannin P. Deep neural network architecture for automated soft surgical skills evaluation using objective structured assessment of technical skills criteria. Int J Comput Assist Radiol Surg. 2023;18:929–37.
Larrazabal LA, del Nido PJ, Jenkins KJ, Gauvreau K, Lacro R, Colan SD et al. Measurement of technical performance in congenital heart surgery: a Pilot Study. Ann Thorac Surg. 2007;83:179–84.
Pham MN, Ko OS, Huang R, Vo AX, Tsai KP, Lai JD et al. An evaluation of peer-rated surgical skill and its relationship with detrusor muscle sampling in transurethral resection of bladder tumor. Urology. 2022;169:134–40.
Nagoshi N, Tsuji O, Suzuki S, Nori S, Yagi M, Okada E et al. Clinical outcomes and a therapeutic indication of intramedullary spinal cord astrocytoma. Spinal Cord. 2022;60:216–22.
Nagoshi N, Okubo T, Ozaki M, Suzuki S, Takeda K, Iga T et al. Epidemiology and surgical outcomes of pediatric intradural spinal tumors: results from a retrospective series of patients operated in the first two decades of life. Spinal Cord. 2025;63:75–9.
Author information
Authors and Affiliations
Contributions
N.N. and K.N. designed the research, analyzed the data, and wrote the paper; T.O. and M.N. performed data collection; T.O., M.O., S.S., K.T., T.I., M.M., M.N. and K.W. supervised the study; all authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
All authors have no conflict to disclose.
Ethics approval and consent to participate
This study received ethical approval from the institutional review board of the Ethics Committee of the Keio University School of Medicine (20110142). We certify that all applicable institutional regulations concerning the ethical use of human volunteers were followed during the research. Informed consent was obtained from all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nagoshi, N., Nagashima, K., Okubo, T. et al. How many cases of spinal intramedullary ependymoma surgery are required to achieve stability? - Analysis using X-bar charts. Spinal Cord 63, 372–376 (2025). https://doi.org/10.1038/s41393-025-01090-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-025-01090-0