Abstract
Study design
In this review, we present a case of Aspergillus spinal epidural abscess (ASEA) and review the literature.
Objectives
To provide further insight on a rare condition.
Setting
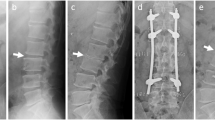
A description of a patient with ASEA in a 58-year-old woman that was successfully treated with conservative management is presented.
Methods
Following case presentation, a literature search (MedLine and PubMed) and assessment of epidemiology, presentation, diagnosis, treatments, and outcomes is performed.
Results
Review of the literature finds 26 reported cases. The infection occurs in males with a higher frequency (66.7%). The thoracic and lumbar regions are more likely afflicted (96.1%). Common symptoms are backache, neurological deficits, and fever. Most frequent comorbidities were malignancy, diabetes mellitus, and immunodeficiency. Complications were numerous and often catastrophic. Treatment entailed a combination of antibiotics and surgery. Overall, ASEA patients did poorly: death in majority (52%), minimal recovery in 22%, and others did attain full recovery (26%).
Conclusions
Generally, this infection has high morbidity and mortality. Early identification is important to a successful outcome. Appropriate management with antifungals is central and proves to be effective as seen in the reported case though surgical intervention is usually a necessity as the literature suggests. From an epidemiological and public health perspective, particularly with recent outbreaks, understanding the treatment of this rare CNS infection becomes even more imperative.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Hendrix WC, Arruda LK, Platts-Mills TA, Haworth CS, Jabour R, Ward GW. Aspergillus epidural abscess and cord compression in a patient with aspergilloma and empyema. Am Rev Respir Dis. 1992;145:1483–6.
Dubbeld P, van Oostenbrugge RJ, Twinjstra A, Schouten HC. Spinal epidural abscess due to Aspergillus infection of the vertebrae: report of 3 cases. Neth J Med. 1996;48:18–23.
Gupta PK, Mahapatra AK, Gaind R, Bhandari S, Musa MM, Lad SD. Aspergillus spinal epidural abscess. Pediatr Neurosurg. 2001;35:18–23.
Tew CW, Han FC, Jureen R, Tey BH. Aspergillus vertebral osteomyelitis and epidural abscess. Singapore Med J. 2009;50:e151–154.
Assaad W, Nuchikat PS, Cohen L, Esguerra JV, Whittier FC. Aspergillus discitis with acute disc abscess. Spine. 1994;19:2226–9.
Batra S, Arora S, Meshram H, Khanna G, Grover SB, Sharma VK. A rare etiology of cauda equina syndrome. J Infect Dev Ctries. 2011;5:79–82.
Chee YC, Poh SC. Aspergillus epidural abscess in a patient with obstructive airway disease. Postgrad Med J. 1983;59:43–45.
Chi CY, Fung CP, Liu CY. Aspergillus flavus epidural abscess and osteomyelitis in a diabetic patient. J Microbiol Immunol Infect. 2003;36:145–8.
Ingwer I, McLeish KR, Tight RR, White AC. Aspergillus fumigatus epidural abscess in a renal transplant recipient. Arch Intern Med. 1978;138:153.
Raj KA, Srinivasamurthy BC, Nagarajan K, Sinduja MG. A rare case of spontaneous Aspergillus spondylodiscitis with epidural abscess in a 45-year-old immunocompetent female. J Craniovertebr Junction Spine. 2013;4:82–84.
Thurnher MM, Olatunji R. Infections of the spine and spinal cord. Handbook Clin Neurol. 2016;136:717–31.
Duarte RM, Vaccaro AR. Spinal infection: state of the art and management algorithm. Eur Spine J. 2013;22:2787–99.
Chiller TM, Roy M, Nguyen D, Guh A, Malani AN, Latham R, et al. Multistate Fungal Infection Clinical Investigation Team Clinical findings for fungal infections caused by methylprednisolone injections. N Engl J Med. 2013;369:1610–9.
Kainer MA, Reagan DR, Nguyen DB, Wiese AD, Wise ME, Ward J, et al. Tennessee Fungal Meningitis Investigation Team Fungal infections associated with contaminated methylprednisolone in Tennessee. N Engl J Med. 2012;367:2194–203.
Smith RM, Schaefer MK, Kainer MA, Wise M, Finks J, Duwve J, et al. Multistate Fungal Infection Outbreak Response Team Fungal infections associated with contaminated methylprednisolone injections. N Engl J Med. 2013;369:1598–609.
Chang HM, Yu HH, Yang YH, Lee WI, Lee JH, Wang LC, et al. Successful treatment of Aspergillus flavus spondylodiscitis with epidural abscess in a patient with chronic granulomatous disease. Pediatr Infect Dis J. 2012;31:100–1.
Saigal G, Donovan Post MJ, Kozic D. Thoracic intradural Aspergillus abscess formation following epidural steroid injection. Am J Neuroradiol. 2004;25:642–4.
Sheth NK, Varkey B, Wagner DK. Spinal cord aspergillus invasion--complication of an aspergilloma. Am J Clin Pathol. 1985;84:763–9.
Tang TJ, Janssen HL, van der Vlies CH, de Man RA, Metselaar HJ, Tilanus HW, et al. Aspergillus osteomyelitis after liver transplantation: conservative or surgical treatment? Eur J Gastroenterol Hepatol. 2000;12:123–6.
Vaishya S, Sharma MS. Spinal Aspergillus vertebral osteomyelitis with extradural abscess: case report and review of literature. Surg Neurol. 2004;61:551–5.
Witzig RS, Greer DL, Hyslop NE Jr. Aspergillus flavus mycetoma and epidural abscess successfully treated with itraconazole. J Med Vet Mycol. 1996;34:133–7.
Yoon KW, Kim YJ. Lumbar Aspergillus osteomyelitis mimicking pyogenic osteomyelitis in an immunocompetent adult. Br J Neurosurg. 2015;29:277–9.
Bridwell KH, Campbell JW, Barenkamp SJ. Surgical treatment of hematogenous vertebral Aspergillus osteomyelitis. Spine. 1990;15:281–5.
Byrd BF, Weiner MH, McGee ZA. Aspergillus spinal epidural abscess. JAMA. 1982;248:3138–9.
Delmas Y, Merville P, Dousse V, Dervau-Durieux L, Morel D, Potaux L. A renal transplant recipient with acute paraparesis due to an Aspergillus epidural abscess. Nephrol Dial Transplant. 1997;12:2185–7.
Go BM, Ziring DJ, Kountz DS. Spinal epidural abscess due to Aspergillus sp in a patient with acquired immunodeficiency syndrome. South Med J. 1993;86:957–60.
Horn D, Sae-Tia S, Neofytos D. Aspergillus osteomyelitis: review of 12 cases identified by the Prospective Antifungal Therapy Alliance registry. Diagn Microbiol Infect Dis. 2009;63:384–7.
Jiang Z, Wang Y, Jiang Y, Xu Y, Meng B. Vertebral osteomyelitis and epidural abscess due to Aspergillus nidulans resulting in spinal cord compression: case report and literature review. J Int Med Res. 2013;41:502–10.
McCaslin AF, Lall RR, Wong AP, Lall RR, Sugrue PA, Koski TR. Thoracic spinal cord intramedullary aspergillus invasion and abscess. J Clin Neurosci. 2015;22:404–6.
Son JM, Jee WH, Jung CK, Kim SI, Ha KY. Aspergillus spondylitis involving the cervico-thoraco-lumbar spine in an immunocompromised patient: a case report. Korean J Radiol. 2007;8:448–51.
van Ooij A, Beckers JM, Herpers MJ, Walenkamp GH. Surgical treatment of aspergillus spondylodiscitis. Eur Spine J. 2000;9:75–9.
Sethi S, Siraj F, Kalra K, Chopra P. Aspergillus vertebral osteomyelitis in immunocompetent patients. Indian J Orthop. 2012;46:246–50.
Kwon JW, Hong SH, Choi SH, Yoon YC, Lee SH. MRI findings of Aspergillus spondylitis. AJR Am J Roentgenol. 2011;197:W919–923.
Wang JL, Chang CH, Young-Xu Y, Chan KA. Systematic review and meta analysis of the tolerability and hepatotoxicity of antifungals in empirical and definitive therapy for invasive fungal infection. Antimicrob Agents Chemother. 2010;54:2409–19.
Ashley ES, Lewis R, Lewis J, Martin C, Andes D. Pharmacology of Systemic Antifungal Agents. Clin Infect Dis. 2006;43:S28–39.
Lewis RE. Current concepts in antifungal pharmacology. Mayo Clin Proc. 2011;86:805–17.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Shweikeh, F., Zyck, S., Sweiss, F. et al. Aspergillus spinal epidural abscess: case presentation and review of the literature. Spinal Cord Ser Cases 4, 19 (2018). https://doi.org/10.1038/s41394-018-0046-y
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41394-018-0046-y
This article is cited by
-
Spinal Epidural Abscess
Current Emergency and Hospital Medicine Reports (2024)