Abstract
Study design
Cohort study.
Objectives
The objectives of this study were examination, observation and surgical interventions of pediatric patients with diastematomyelia, a rare congenital deformity of the spinal cord.
Setting
Spine surgery and neurosurgery clinic under ministry of health, the Russian Federation.
Methods
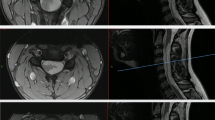
Twenty children (1–18 years of age) with diastematomyelia participated in this study. Diagnosis was based on subjects’ medical history, results of clinical examination, spine radiography in anteroposterior and lateral views, and neurophysiological examinations. Septum resection surgery was done in seventeen subjects.
Results
All the subjects had skin manifestations along the midline of the back. Neurological symptoms were noted in 17 subjects: paraparesis in 11, urinary incontinence in 2, monoparesis in 4, and spasticity in 2 subjects. Three subjects did not show any neurological deficit. Orthopedic examination revealed spinal deformities of various degrees of severity. In 4 subjects, partial restorations of neurological functions were observed; and in 1 subject, bladder incontinence developed after the surgery.
Conclusions
Patients who have limb length discrepancy, congenital scoliosis, skin manifestations should be examined for the presence of diastematomyelia. Patients having neither neurological deficit nor orthopedic deterioration should be monitored, and in case of deterioration, surgical treatment should be reserved. We advocate for performing resection of the septum in patients with diastematomyelia prior to surgical correction of scoliosis or orthopedic correction of lower limb deformities.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Pang D, Dias MS, Ahab-Barmada M. Split cord malformation: Part I: A unified theory of embryogenesis for double spinal cord malformations. Neurosurgery. 1992;31:451–80.
Dias MS, Pang D. Split cord malformations. Neurosurg Clin N Am. 1995;6:339–58.
Herren RY, Edwards JE. Diplomyelia (duplication of the spinal cord). Arch Path. 1940;30:1203–14.
Bekki H, Morishita Y, Kawano O, Shiba K, Iwamoto Y. Diastematomyelia: A Surgical Case with Long-Term Follow-Up. Asian. Spine J. 2015;9:99–102.
Kennedy PR. New data on diastematomyelia. J Neurosurg. 1979;51:355–61.
Gan YC, Sgouros S, Walsh AR, Hockley AD. Diastematomyelia in children: treatment outcome and natural history of associated syringomyelia. Child’s Nerv Syst. 2007;23:515–9.
Miller A, Guille JT, Bowen JR. Evaluation and treatment of diastematomyelia. JBJS. 1993;75:1308–17.
Andersson H, Sullivan L. Diastematomyelia: report of two cases submitted to laminectomy. Acta Orthop Scand. 1965;36:257–64.
Shaw JF. Diastematomyelia. Dev Med Child Neurol. 1975;17:361–4.
Winter RB, Haven JJ, Moe JH, Lagaard SM. Diastematomyelia and congenital spine deformities. JBJS. 1974;56:27–39.
Keim HA, Greene AF. Diastematomyelia and Scoliosis. JBJS. 1973;55:1425–35.
Acknowledgements
The authors thank all the participants of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Vissarionov, S.V., Krutelev, N.A., Snischuk, V.P. et al. Diagnosis and treatment of diastematomyelia in children: a perspective cohort study. Spinal Cord Ser Cases 4, 109 (2018). https://doi.org/10.1038/s41394-018-0141-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-018-0141-0
This article is cited by
-
Pre-operative clinical deterioration and long-term surgical outcomes in 41 patients with split cord malformation type 1
Child's Nervous System (2024)