Abstract
Introduction
Ganglion impar block (GIB) is a well-recognised treatment for chronic coccydynia. Several side effects have previously been described with this procedure, including transient motor dysfunction, bowel, bladder, and sexual dysfunction, neuritis, rectal perforation, impingement of the sciatic nerve, cauda equina syndrome, and infection.
Case presentation
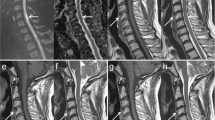
We describe the first report of imaging-documented conus infarction after an unguided-GIB performed in theatre using particulate steroids for a 17-year-old patient with coccydynia. Immediately post-GIB, patient developed transient neurological deficits in her lower limbs of inability to mobilise her legs that lasted for 24 h. These include back and leg pain, decreased power and movement, increased tone, brisk reflexes, reduced light touch sensation and proprioception of legs up to the T10 level. Urgent MRI spine showed intramedullary hyperintense signal within the conus and mild restricted diffusion on the distal cord and conus, suggestive of an acute conus infarction. On follow-up, the GIB did not result in symptom improvement of coccydynia and there was persistent altered sensation of her legs.
Discussion
Various approaches of ganglion impar block have been described and performed in the past with different imaging techniques and injectants. A few cases of unusual neurological complications have been reported with the use of epidural steroid injections and ganglion impar block. Clinicians should be aware of the possible neurological complications following ganglion impar blocks and the risk of inadvertent intravascular injection of particulate steroids can potentially to be minimised by using imaging guidance.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Gunduz OH, Kenis-Coskun O. Ganglion blocks as a treatment of pain: current perspectives. J Pain Res. 2017;10:2815–26.
Oh C-S, Chung I-H, Ji H-J, Yoon D-M. Clinical implications of topographic anatomy on the ganglion impar. Anesthesiology. 2004;101:249–50.
Toshniwal GR, Dureja GP, Prashanth SM. Transsacrococcygeal approach to ganglion impar block for management of chronic perineal pain: a prospective observational study. Pain Physician. 2007;10:661–6.
Walters A, Muhleman M, Osiro S, Bubb K, Snosek M, Shoja MM, et al. One is the loneliest number: A review of the ganglion impar and its relation to pelvic pain syndromes. Clin Anat. 2013;26:855–61.
Wang G, Liang J, Jia Z, Wan L, Yang M. Spinal cord infarction caused by sacral canal epidural steroid injection. Medicine (U S). 2018;97:E0111.
Gharibo CG, Fakhry M, Diwan S, Kaye AD. Conus medullaris infarction after a right l4 transforaminal epidural steroid injection using dexamethasone. Pain Physician. 2016;19:E1211–4.
Gupta N, Garg R, Saini S, Bharti SJ, Kumar V. An unusual complication after ganglion impar block for chronic cancer pain management. AANA J. 2017;85:424–6.
Foye PM, Buttaci CJ, Stitik TP, Yonclas PP. Successful injection for coccyx pain. Am J Phys Med Rehabil. 2006;85:783–4.
Plancarte DR, Amescua C, Patt RB, Allende S. Presacral blockade of the ganglion of walther (ganglion Impar). Anesthesiol J Am Soc Anesthesiol. 1990;73(3A):A751.
Huang JJ. Another modified approach to the ganglion of Walther block (ganglion of impar). J Clin Anesth. 2003;15:282–3.
Lin CS, Cheng JK, Hsu YW, Chen CC, Lao HC, Huang CJ, et al. Ultrasound-guided ganglion impar block: A technical report. Pain Med. 2010;11:390–4.
Datir A, Connell D. CT-guided injection for ganglion impar blockade: a radiological approach to the management of coccydynia. Clin Radio. 2010;65:21–5.
Marker DR, U-Thainual P, Ungi T, Flammang AJ, Fichtinger G, Iordachita II, et al. MR-guided perineural injection of the ganglion impar: technical considerations and feasibility. Skelet Radio. 2016;45:591–7.
Scott-Warren JT, Hill V, Rajasekaran A. Ganglion impar blockade: a review. Curr Pain Headache Rep. 2013;17:306.
Dietrich TJ, Sutter R, Froehlich JM, Pfirrmann CWA. Particulate versus non-particulate steroids for lumbar transforaminal or interlaminar epidural steroid injections: an update. Skelet Radio. 2015;44:149–55.
KENALOG ®-40 INJECTION (triamcinolone acetonide injectable suspension, USP) [Internet]. [cited 22 May 2019]. Available from: https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=e25cfc22-29ba-473f-88c4-3c88e9f6863b&type=display.
Ludwig MA, Burns SP. Spinal cord infarction following cervical transforaminal epidural injection. Spine (Philos Pa 1976). 2005;30:E266–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kuek, D.K.C., Chung, S.L., Zishan, U.S. et al. Conus infarction after non-guided transcoccygeal ganglion impar block using particulate steroid for chronic coccydynia. Spinal Cord Ser Cases 5, 92 (2019). https://doi.org/10.1038/s41394-019-0237-1
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41394-019-0237-1
This article is cited by
-
Fibrocartilaginous embolism of the posterior spinal artery: A case report regarding the responsible intervertebral disc on magnetic resonance imaging
Spinal Cord Series and Cases (2022)
-
Bupivacaine/triamcinolone
Reactions Weekly (2020)