Abstract
Introduction
The etiologies of pediatric spinal cord infarction are commonly cardiovascular problems resulting from hypotensive events from trauma and abdominal aortic surgery. Non-traumatic spinal cord infarction in children is rare and remains difficult to diagnose. We report a case of non-traumatic spinal cord infarction of the conus medullaris in a child who recovered after receiving only rehabilitative treatment.
Case presentation
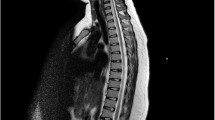
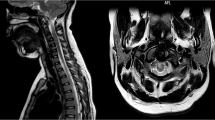
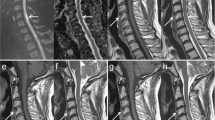
A 12-year-old female patient experienced sudden low back pain for 2 days, followed by weakness in the lower extremities and difficulties in micturition. On admission, magnetic resonance imaging indicated spinal cord infarction of the conus medullaris. After initial treatment with prednisone and mannitol, a few weeks of intensive rehabilitation was recommended. Physical therapy focused on improving lower limb strength. A plastic solid ankle-foot orthosis was used with Lofstrand crutches throughout the period of rehabilitation. After 2 months of rigorous therapy, she was able to walk independently.
Discussion
Non-traumatic spinal cord infarction of the conus medullaris in children is extremely rare. The current case is unique because it involves a patient who presented with pediatric spinal cord infarction of the conus medullaris and showed remarkable neurological recovery after rehabilitation. The case describes a rare spinal cord infarction in a pediatric patient and emphasizes the importance of providing an accurate diagnosis and treatment.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Robertson CE, Brown RD, Wijdicks EF, Rabinstein AA. Recovery after spinal cord infarcts: long-term outcome in 115 patients. Neurology. 2012;78:114–21.
Mullen M, McGarvey M. Spinal cord infarction: vascular anatomy and etiologies. Waltham, MA: UpToDate; 2015.
Vargas M, Gariani J, Sztajzel R, Barnaure-Nachbar I, Delattre BM, Lovblad KO, et al. Spinal cord ischemia: practical imaging tips, pearls, and pitfalls. Am J Neuroradiol 2015;36:825–30.
Küker W, Weller M, Klose U, Krapf H, Dichgans J, Nägele T. Diffusion-weighted MRI of spinal cord infarction. J Neurol. 2004;251:818–24.
Thron AK. Vascular anatomy of the spinal cord: neuroradiological investigations and clinical syndromes. Berlin: Springer Science & Business Media; 1988.
Masson C, Pruvo J, Meder J, Cordonnier C, Touzé E, De La Sayette V, et al. Spinal cord infarction: clinical and magnetic resonance imaging findings and short term outcome. J Neurol Psychiatry. 2004;75:1431–5.
Wong JJ, Dufton J, Mior SA. Spontaneous conus medullaris infarction in a 79 year-old female with cardiovascular risk factors: a case report. J Can Chiropr Assoc. 2012;56:58.
Hendelman W. Atlas of functional neuroanatomy. 2nd edn. Florida: CRC Press; 2005. p. 296.
Burns S, Mior S, O’Connor S. Cervical spondylotic myelopathy: Part I: anatomical and pathomechanical considerations. J Can Chiropr Assoc 1991;35:75.
Sladky JT, Rorke LB. Perinatal hypoxic/ischemic spinal cord injury. Pediatr Pathol 1986;6:87–101.
Monteiro L, Leite I, Pinto JA, Stocker A. Spontaneous thoracolumbar spinal cord infarction: report of six cases. Acta Neurol Scand 1992;86:563–6.
Sheikh A, Warren D, Childs AM, Russell J, Liddington M, Guruswamy V, et al. Paediatric spinal cord infarction—a review of the literature and two case reports. Child Nerv Syst 2017;33:671–6.
Norman MG. Respiratory arrest and cervical spinal cord infarction following lumbar puncture in meningitis. J Can Chiropr Assoc 1982;9:443–7.
Pang D, Wilberger JE. Spinal cord injury without radiographic abnormalities in children. J Neurosurg 1982;57:114–29.
Riche M, Modenesi-Freitas J, Djindjian M, Merland J. Arteriovenous malformations (AVM) of the spinal cord in children. Neuroradiology. 1982;22:171–80.
Hasegawa M, Yamashita J, Yamashima T, Ikeda K, Fujishima Y, Yamazaki M. Spinal cord infarction associated with primary antiphospholipid syndrome in a young child: case report. J Neurosurg 1993;79:446–50.
Wieting JM, Krach LE. Spinal cord injury rehabilitation in a pediatric achondroplastic patient: case report. Arch Phys Med Rehabil 1994;75:106–8.
Davis GA, Klug GL. Acute-onset nontraumatic paraplegia in childhood: fibrocartilaginous embolism or acute myelitis? Child Nerv Syst 2000;16:551–4.
Beslow LA, Ichord RN, Zimmerman RA, Smith S, Licht D. Role of diffusion MRI in diagnosis of spinal cord infarction in children. Neuropediatrics. 2008;39:188–91.
Boddu SR, Cianfoni A, Kim KW, Banihashemi MA, Pravatà E, Gobin YP, et al. Spinal cord infarction and differential diagnosis. Neurovascular imaging: from basics to advanced concepts. New York: Springer New York; 2014. p. 1–64.
Khong P-L, Ho H-K, Cheng P-W, Wong VC, Goh W, Chan F-LJPr. Childhood acute disseminated encephalomyelitis: the role of brain and spinal cord MRI. Pediatr Radiol 2002;32:59–66.
van Doorn PAJLPM. Diagnosis, treatment and prognosis of Guillain–Barré syndrome (GBS). Presse Méd. 2013;42:e193–201.
Choi KH, Lee KS, Chung SO, Park JM, Kim YJ, Kim HS, et al. Idiopathic transverse myelitis: MR characteristics. Am J Neuroradiol 1996;17:1151–60.
Transverse Myelitis Consortium Working Group. Proposed diagnostic criteria and nosology of acute transverse myelitis. Neurology. 2002;59:499–505.
Weidauer S, Nichtweiss M, Lanfermann H, Zanella FEJN. Spinal cord infarction: MR imaging and clinical features in 16 cases. Neuroradiology. 2002;44:851–7.
Geldmacher DS. Vascular diseases of the nervous system: spinal cord vascular disease. Bradley’s neurology in clinical practice. 6th ed. Philadelphia: Elsevier; 2012.
Ebner FH, Roser F, Acioly MA, Schoeber W, Tatagiba M. Intramedullary lesions of the conus medullaris: differential diagnosis and surgical management. Neurosurg Rev 2009;32:287.
Kingwell SP, Curt A, Dvorak MF. Factors affecting neurological outcome in traumatic conus medullaris and cauda equina injuries. Neurosurg Focus. 2008;25:E7.
Stettler S, El-Koussy M, Ritter B, Boltshauser E, Jeannet PY, Kolditz P, et al. Non-traumatic spinal cord ischaemia in childhood—clinical manifestation, neuroimaging and outcome. Eur J Paediatr Neurol 2013;17:176–84.
de la Barrera SS, Barca-Buyo A, Montoto-Marques A, Ferreiro-Velasco M, Cidoncha-Dans M, Rodriguez-Sotillo A. Spinal cord infarction: prognosis and recovery in a series of 36 patients. Spinal Cord 2001;39:520.
Acknowledgements
This work was supported by a 2-year Research Grant of Pusan National University. We acknowledge Editage (www.editage.com), an English editing service, for editing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Seo, Z.W., Huh, S. & Ko, HY. Non-traumatic spinal cord infarction of the conus medullaris in a child: a case report. Spinal Cord Ser Cases 7, 59 (2021). https://doi.org/10.1038/s41394-021-00425-2
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41394-021-00425-2