Abstract
Introduction
Neuropathic pain after spinal cord injury is difficult to treat, and it is associated with abnormalities in the function of the thalamus-to-cortex neural circuitry. Aerobic exercise provides immediate improvement in neuropathic pain and is associated with abnormal resting electroencephalography (EEG) findings in patients with spinal cord injury. This study aimed to investigate whether physical therapy, including walking, can improve neuropathic pain and EEG peak alpha frequency (PAF) in the long term in a patient with cervical spinal cord injury.
Case presentation
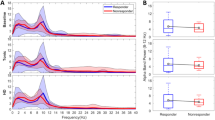
A 50-year-old man was admitted with a cervical spinal cord insufficiency injury sustained one week prior. The residual height was C5. Neuropathic pain was observed in the fingers bilaterally. A numerical rating scale (NRS) was evaluated to measure the weekly mean and maximum intensities of pain. Resting EEG was measured, and the PAF was calculated. Each time point was evaluated in 2-week intervals from the time of admission, and the rate of change (Δ) of PAF was calculated based on the initial evaluation. Interventions included 18 weeks of standard physical therapy focusing on gait, with additional intensive gait training (4–10 weeks). The NRS scores for the mean and maximum intensities of pain decreased significantly after 6 weeks, and ΔPAF increased significantly after 4 weeks. Improvement in PAF coincided with the start of intensive gait training.
Discussion
PAF shifts to a high frequency during intensive gait training, suggesting the effectiveness of aerobic exercise. Furthermore, there is a close relationship between PAF, pain, and the quantification of pain changes.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
Original data have been stored by the corresponding author and will be made available on request.
References
Levi R, Hultling C, Nash MS, Seiger A. The Stockholm spinal cord injury study: 1. Medical problems in a regional SCI population. Paraplegia. 1995;33:308–15. https://doi.org/10.1038/sc.1995.70.
Finnerup NB, Johannesen IL, Sindrup SH, Bach FW, Jensen TS. Pain and dysesthesia in patients with spinal cord injury: a postal survey. Spinal Cord. 2001;39:256–62. https://doi.org/10.1038/sj.sc.3101161.
Burke D, Fullen BM, Stokes D, Lennon O. Neuropathic pain prevalence following spinal cord injury: a systematic review and meta-analysis. Eur J Pain. 2017;21:29–44. https://doi.org/10.1002/ejp.905.
Adriaansen JJE, Post MWM, de Groot S, van Asbeck FWA, Stolwijk-Swüste JM, Tepper M, et al. Secondary health conditions in persons with spinal cord injury: a longitudinal study from one to five years post-discharge. J Rehabil Med. 2013;45:1016–22. https://doi.org/10.2340/16501977-1207.
Widerström-Noga EG, Felipe-Cuervo E, Yezierski RP. Chronic pain after spinal injury: interference with sleep and daily activities. Arch Phys Med Rehabil. 2001;82:1571–7. https://doi.org/10.1053/apmr.2001.26068.
Ataoğlu E, Tiftik T, Kara M, Tunç H, Ersöz M, Akkuş S. Effects of chronic pain on quality of life and depression in patients with spinal cord injury. Spinal Cord. 2013;51:23–6. https://doi.org/10.1038/sc.2012.51.
Fawkes-Kirby TM, Wheeler MA, Anton HA, Miller WC, Townson AF, Weeks CAO. Clinical correlates of fatigue in spinal cord injury. Spinal Cord. 2008;46:21–5. https://doi.org/10.1038/sj.sc.3102053.
Kressler J, Thomas CK, Field-Fote EC, Sanchez J, Widerström-Noga E, Cilien DC, et al. Understanding therapeutic benefits of overground bionic ambulation: exploratory case series in persons with chronic, complete spinal cord injury. Arch Phys Med Rehabil. 2014;95:1878–87. https://doi.org/10.1016/j.apmr.2014.04.026.
Cruciger O, Schildhauer TA, Meindl RC, Tegenthoff M, Schwenkreis P, Citak M, et al. Impact of locomotion training with a neurologic controlled hybrid assistive limb (HAL) exoskeleton on neuropathic pain and health related quality of life (HRQoL) in chronic SCI: a case study. Disabil Rehabil Assist Technol. 2016;11:529–34. https://doi.org/10.3109/17483107.2014.981875.
Norrbrink C, Lindberg T, Wahman K, Bjerkefors A. Effects of an exercise programme on musculoskeletal and neuropathic pain after spinal cord injury–results from a seated double-poling ergometer study. Spinal Cord. 2012;50:457–61. https://doi.org/10.1038/sc.2011.160.
Soler MD, Kumru H, Pelayo R, Vidal J, Tormos JM, Fregni F, et al. Effectiveness of transcranial direct current stimulation and visual illusion on neuropathic pain in spinal cord injury. Brain. 2010;133:2565–77. https://doi.org/10.1093/brain/awq184.
Moseley LG. Using visual illusion to reduce at-level neuropathic pain in paraplegia. Pain. 2007;130:294–8. https://doi.org/10.1016/j.pain.2007.01.007.
Heutink M, Post MWM, Bongers-Janssen HMH, Dijkstra CA, Snoek GJ, Spijkerman DCM, et al. The CONECSI trial: results of a randomized controlled trial of a multidisciplinary cognitive behavioral program for coping with chronic neuropathic pain after spinal cord injury. Pain. 2012;153:120–8. https://doi.org/10.1016/j.pain.2011.09.029.
Vaegter HB, Handberg G, Graven-Nielsen T. Similarities between exercise-induced hypoalgesia and conditioned pain modulation in humans. Pain. 2014;155:158–67. https://doi.org/10.1016/j.pain.2013.09.023.
Sato G, Osumi M, Morioka S. Effects of wheelchair propulsion on neuropathic pain and resting electroencephalography after spinal cord injury. J Rehabil Med. 2017;49:136–43. https://doi.org/10.2340/16501977-2185.
Sarnthein J, Stern J, Aufenberg C, Rousson V, Jeanmonod D. Increased EEG power and slowed dominant frequency in patients with neurogenic pain. Brain. 2006;129:55–64. https://doi.org/10.1093/brain/awh631.
Wydenkeller S, Maurizio S, Dietz V, Halder P. Neuropathic pain in spinal cord injury: significance of clinical and electrophysiological measures. Eur J Neurosci. 2009;30:91–9. https://doi.org/10.1111/j.1460-9568.2009.06801.x.
Llinás RR, Ribary U, Jeanmonod D, Kronberg E, Mitra PP. Thalamocortical dysrhythmia: a neurological and neuropsychiatric syndrome characterized by magnetoencephalography. Proc Natl Acad Sci USA. 1999;96:15222–7. https://doi.org/10.1073/pnas.96.26.15222.
Gutmann B, Mierau A, Hülsdünker T, Hildebrand C, Przyklenk A, Hollmann W, et al. Effects of physical exercise on individual resting state EEG alpha peak frequency. Neural Plast. 2015;2015:717312. https://doi.org/10.1155/2015/717312.
Bryce TN, Biering-Sørensen F, Finnerup NB, Cardenas DD, Defrin R, Lundeberg T, et al. International spinal cord injury pain classification: part I. Background and description. March 6-7, 2009. Spinal Cord. 2012;50:413–7.
Matsuki Y, Sukenaga N, Miyagi K, Tsunetoh T, Mizogami M, Shigemi K, et al. Reliability and validity of the Japanese translation of the DN4 Diagnostic Questionnaire in patients with neuropathic pain. J Anesth. 2018;32:403–8.
Klimesch W, Russegger H, Doppelmayr M, Pachinger T. A method for the calculation of induced band power: implications for the significance of brain oscillations. Electroencephalogr Clin Neurophysiol. 1998;108:123–30. https://doi.org/10.1016/s0168-5597(97)00078-6.
Klimesch W. EEG alpha and theta oscillations reflect cognitive and memory performance: a review and analysis. Brain Res Brain Res Rev. 1999;29:169–95. https://doi.org/10.1016/s0165-0173(98)00056-3.
Gramkow MH, Hasselbalch SG, Waldemar G, Frederiksen KS. Resting state EEG in exercise intervention studies: a systematic review of effects and methods. Front Hum Neurosci. 2020;14:155.
Gutmann B, Zimmer P, Hülsdünker T, Lefebvre J, Binnebößel S, Oberste M, et al. The effects of exercise intensity and post-exercise recovery time on cortical activation as revealed by EEG alpha peak frequency. Neurosci Lett. 2018;668:159163.
Ngernyam N, Jensen MP, Arayawichanon P, Auvichayapat N, Tiamkao S, Janjarasjitt S, et al. The effects of transcranial direct current stimulation in patients with neuropathic pain from spinal cord injury. Clin Neurophysiol. 2015;126:382–90. https://doi.org/10.1016/j.clinph.2014.05.034.
Siddall PJ, Taylor DA, McClelland JM, Rutkowski SB, Cousins MJ. Pain report and the relationship of pain to physical factors in the first 6 months following spinal cord injury. Pain. 1999;81:187–97.
Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003;103:249–57.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
This work was supported by a JSPS KAKENHI Grant-in-Aid for Young Scientists (Number 21K17482).
Author information
Authors and Affiliations
Contributions
GS carried out planning the work and participated in acquired the data and draft the manuscript. MO participated in the data analysis and helped to draft the manuscript. RM participated in acquire the data. SM participated in helping draft the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Written informed consent was obtained from the patient for the publication.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sato, G., Osumi, M., Mikami, R. et al. Long-term physical therapy for neuropathic pain after cervical spinal cord injury and resting state electroencephalography: a case report. Spinal Cord Ser Cases 8, 41 (2022). https://doi.org/10.1038/s41394-022-00510-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-022-00510-0