Abstract
Study design
Exploratory clinical investigation.
Objectives
To assess the feasibility, acceptability, and preliminary efficacy of upper-body rowing exercise adapted to wheelchair users with spinal cord injury (SCI).
Setting
University exercise laboratory.
Methods
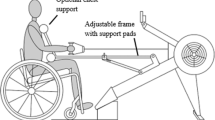
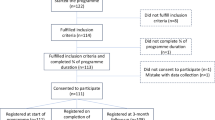
Eight individuals with SCI exercised on a rowing ergometer modified for wheelchair users (REMW), three times weekly, for up to 30 min per session. Participants completed feasibility and acceptability questionnaire (1–5 Likert scale), and the Wheelchair Users Shoulder Pain Index (WUSPI) before and after six weeks of exercise. Average power output (POAVG), distance rowed, percent peak heart rate (%HRpeak), and rating of perceived exertion (RPE) (6–20 scale) were monitored throughout the 18 exercise sessions and analyzed to evaluate preliminary efficacy of the exercise modality.
Results
All eight participants completed the study (97% adherence). Participants rated the exercise high on the feasibility and acceptability scale; median (interquartile range) = 5.0 (4.0–5.0), where higher numbers indicated greater feasibility. Shoulder pain was reduced by 21% yet not significantly different from baseline (p = 0.899). Physiological measures (%HRpeak = 80–83%; RPE = 15.0–16.0) indicated a high cardiovascular training load. From week 1 to week 6, POAVG and distance rowed increased by 37 and 36%, respectively (both p ≤ 0.001).
Conclusions
Data from six weeks of exercise on the REMW suggests that upper-body rowing is a feasible and acceptable exercise modality for wheelchair users with SCI. Session data on %HRpeak, RPE, and shoulder pain indicate that REMW evoked moderate to vigorous intensity exercise without exacerbation of shoulder pain. Future research is required to quantify potential training-induced changes in cardiorespiratory fitness.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets of the current study are available from the corresponding author on reasonable request.
Change history
16 May 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41394-022-00522-w
References
Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, Barrow A, Bourne C, Carruthers P, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord. 2018;56:308–21.
Eitivipart AC, de Oliveira CQ, Arora M, Middleton J, Davis GM. Overview of systematic reviews of aerobic fitness and muscle strength training after spinal cord injury. J Neurotrauma. 2019;36:2943–2963.
Dolbow DR, Figoni SF. Accommodation of wheelchair-reliant individuals by community fitness facilities. Spinal Cord. 2015;53:515–519.
Gutierrez DD, Thompson L, Kemp B, Mulroy S. The relationship of shoulder pain intensity to quality of life, physical activity, and community participation in persons with paraplegia. J Spinal Cord Med. 2007;30:251–5.
Hansen RK, Larsen RG, Laessoe U, Samani A, Cowan RE. Physical activity barriers in danish manual wheelchair users: a cross-sectional study. Arch Phys Med Rehabil. 2021;102:687–93.
Nash MS, van de Ven I, van Elk N, Johnson BM. Effects of circuit resistance training on fitness attributes and upper-extremity pain in middle-aged men with paraplegia. Arch Phys Med Rehabil. 2007;88:70–75.
Ambrosio F, Boninger ML, Souza AK, Fitzgerald SG, Koontz AM, Cooper RA. Biomechanics and strength of manual wheelchair users. J Spinal Cord Med. 2005;28:407–14.
Burnham RS, May L, Nelson E, Steadward R, Reid DC. Shoulder pain in wheelchair athletes. The role of muscle imbalance. Am J Sports Med. 1993;21:238–42.
van der Scheer JW, Martin Ginis KA, Ditor DS, Goosey-Tolfrey VL, Hicks AL, West CR, et al. Effects of exercise on fitness and health of adults with spinal cord injury. A systematic review. Neurology 2017;89:736–45.
Farrow M, Nightingale TE, Maher J, McKay CD, Thompson D, Bilzon JLJ. Effect of exercise on cardiometabolic risk factors in adults with chronic spinal cord injury: a systematic review. Arch Phys Med Rehabil. 2020;101:2177–205.
Arnet U, Van Drongelen S, Scheel-Sailer A, Van Der Woude LHV, Veeger DHEJ. Shoulder load during synchronous handcycling and handrim wheelchair propulsion in persons with paraplegia. J Rehabil Med. 2012;44:222–8.
Curtis KA, Tyner TM, Zachary L, Lentell G, Brink D, Didyk T, et al. Effect of a standard exercise protocol on shoulder pain in long-term wheelchair users. Spinal Cord. 1999;37:421–9.
Volianitis S, Yoshiga CC, Secher NH. The physiology of rowing with perspective on training and health. Eur J Appl Physiol. 2020;120:1943–63.
Olenik LM, Laskin JJ, Burnham R, Wheeler CD, Steadward RD. Efficacy of rowing, backward wheeling and isolated scapular retractor exercise as remedial strength activities for wheelchair users: application of electromyography. Paraplegia. 1995;33:148–52.
Ye G, Grabke EP, Pakosh M, Furlan JC, Masani K. Clinical benefits and system design of FES-rowing exercise for rehabilitation of individuals with spinal cord injury: a systematic review. Arch Phys Med Rehabil. 2021;102:1595–605.
Gorgey AS, Dolbow DR, Dolbow JD, Khalil RK, Gater DR. The effects of electrical stimulation on body composition and metabolic profile after spinal cord injury - Part II. J Spinal Cord Med. 2015;38:23–37.
Solinsky R, Draghici A, Hamner JW, Goldstein R, Taylor A. High-intensity, whole-body exercise improves blood pressure control in individuals with spinal cord injury: a prospective randomized controlled trial. PLoS One. 2021;16:1–13.
Lamont LS. A simple ergometer modification can expand the exercise options for wheelchair clients. Disabil Rehabil Assist Technol. 2011;6:176–8.
Troy KL. Biomechanical validation of upper extremity exercise in wheelchair users: design considerations and improvements in a prototype device. Disabil Rehabil Assist Technol. 2011;6:22–28.
Troy KL, Munce TA, Longworth JA. An exercise trial targeting posterior shoulder strength in manual wheelchair users: Pilot results and lessons learned. Disabil Rehabil Assist Technol. 2015;10:415–20.
Wong RN, Stewart AL, Sawatzky B, Laskin JJ, Borisoff J, Mattie J et al. Exploring exercise participation and the usability of the adaptive rower and arm crank ergometer through wheelchair users’ perspectives. Disabil. Rehabil. (in press).
Hansen RK, Samani A, Laessoe U, Handberg A, Larsen RG. Effect of wheelchair-modified rowing exercise on cardiometabolic risk factors in spinal cord injured wheelchair users: protocol for a randomised controlled trial. BMJ Open. 2020;10:e040727.
Powell KE, Paluch AE, Blair SN. Physical activity for health: what kind? how much? how intense? on top of what? Annu Rev Public Health. 2011;32:349–65.
Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehab Med. 1970;2-3:92–98.
Soper C, Hume PA. Towards an ideal rowing technique for performance: the contributions from biomechanics. Sport Med. 2004;34:825–48.
Visovsky C, Corripio J. Feasibility and acceptability of a resistance exercise intervention: for women undergoing chemotherapy for breast cancer. Nurs Heal. 2015;3:110–9.
Curtis KA, Roach KE, Applegate EB, Amar T, Benbow CS, Genecco TD, et al. Development of the Wheelchair User’s Shoulder Pain Index (WUSPI). Paraplegia. 1995;33:290–3.
Martin Ginis KA, Hicks AL. Exercise research issues in the spinal cord injured population. Exerc Sport Sci Rev. 2005;33:49–53.
Baumgart JK, Brurok B, Sandbakk Ø. Comparison of peak oxygen uptake between upper-body exercise modes: a systematic literature review and meta-analysis. Front Physiol. 2020;11:1–12.
Cragg JJ, Noonan VK, Krassioukov A, Borisoff J. Cardiovascular disease and spinal cord injury. Results a Natl Popul health Surv Neurol. 2013;81:723–8.
Wilbanks SR, Rogers R, Pool S, Bickel CS. Effects of functional electrical stimulation assisted rowing on aerobic fitness and shoulder pain in manual wheelchair users with spinal cord injury. J Spinal Cord Med. 2016;39:645–54.
Curtis KA, Roach KE, Applegate EB, Amar T, Benbow CS, Genecco TD, et al. Reliability and validity of the Wheelchair User’s Shoulder Pain Index (WUSPI). Paraplegia. 1995;33:595–601.
Bjerkefors A, Tinmark F, Nilsson J, Arndt A. Seated double-poling ergometer performance of individuals with spinal cord injury - a new ergometer concept for standardized upper body exercise. Int J Sports Med. 2013;34:176–82.
Evans N, Wingo B, Sasso E, Hicks A, Gorgey AS, Harness E. Exercise recommendations and considerations for persons with spinal cord injury. Arch Phys Med Rehabil. 2015;96:1749–50.
Acknowledgements
We would like to thank the participants who participated in the study. We would also like to acknowledge suppliers of training equipment (Wolturnus A/S for assistive equipment (Bodypoint vests and belt) and arm crank ergometer; Aalborg Rowing Club for lending of a Concept 2 ergometer; Modest Sport for sponsoring Adapt2row units; and iQniter for sponsoring heart rate belts). No financial assistance was received in support of this study.
Author information
Authors and Affiliations
Contributions
RKH, AS, UL and RGL conceived and designed the protocol. RKH, JLJW and KF acquired data and RKH and JLJW analyzed data. RKH, AS, UL, RGL and KF interpreted the results. RKH and RGL drafted the manuscript and JLJW, AS, UL, KF revised the manuscript for important intellectual content. RKH, JLJW, AS, UL, KF and RGL all approved the final version of the manuscript, and all agreed to be accountable for all aspects of the work. As a corresponding author, RKH confirms that he has full access to the data in this study and final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the Committees on Health Research Ethics in The North Denmark Region (N-20190053) and registered at ClinicalTrials.gov (NCT04390087). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Informed consent
All participants received verbal as well as written information about the study before written consent was obtained.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hansen, R.K., de Wit, J.L.J., Samani, A. et al. Wheelchair-modified ergometer rowing exercise in individuals with spinal cord injury: a feasibility, acceptability, and preliminary efficacy study. Spinal Cord Ser Cases 8, 48 (2022). https://doi.org/10.1038/s41394-022-00518-6
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41394-022-00518-6
This article is cited by
-
A pull function attachment to manual wheelchairs: a case report on usability and shoulder pain in people with spinal cord injury
Spinal Cord Series and Cases (2025)
-
Rowing exercise increases cardiorespiratory fitness and brachial artery diameter but not traditional cardiometabolic risk factors in spinal cord-injured humans
European Journal of Applied Physiology (2023)