Abstract
Introduction
Post-traumatic syringomyelia is an uncommon complication after traumatic spinal cord injury. This case study details our decision-making and surgical approach for a patient with symptomatic post-traumatic syringomyelia after sustaining a gunshot wound.
Case presentation
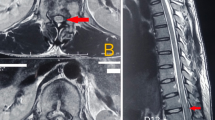
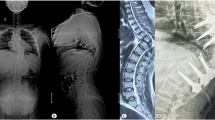
A 24-year-old man with past medical history of distant American Spinal Injury Association Impairment Grade B spinal cord injury due to ballistic injury developed delayed post-traumatic syringomyelia, resulting in unilateral sensory loss and left upper extremity weakness. CT and MR imaging revealed a syrinx spanning his cervical and thoracic spine causing significant spinal cord compression. To relieve achieve decompression and restore CSF flow dynamics, we performed a bony extradural decompression, bullet fragment extraction, spinal cord untethering, and midline myelotomy. Postoperatively, the patient demonstrated clinical and radiographical improvement.
Discussion
Post-traumatic syringomyelia is potentially morbid sequalae of spinal cord injuries. Suspicion for post-traumatic syringomyelia should be maintained in patients with delayed, progressive neurologic deficits. In this setting, surgical intervention may require extradural and intradural procedures to mitigate neural compression along the dilated central canal by the syrinx.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.
References
Lasfargues JE, Custis D, Morrone F, Carswell J, Nguyen T. A model for estimating spinal cord injury prevalence in the United States. Paraplegia. 1995;33:62–8.
Schlesinger H. Die Syringomyelie: Eine Monographie. Leipzig und Wien: Franz Deuticke; 1895.
Hida K, Iwasaki Y, Imamura H, Abe H. Posttraumatic syringomyelia: its characteristic magnetic resonance imaging findings and surgical management. Neurosurgery. 1994;35:886–91.
Elliott NS, Lockerby DA, Brodbelt AR. A lumped-parameter model of the cerebrospinal system for investigating arterial-driven flow in posttraumatic syringomyelia. Med Eng Phys. 2011;33:874–82.
Mitchell JK (editor). Incomplete sections of nerves; injuries of the spinal cord and its neighborhood. In: Remote consequences of injuries of nerves and their treatment. Philadelphia: Lea Brothers & Co; 1895. p. 114–7.
Wagner W, Stolper P. Die Verletzungen der WirbelsaÈule und des RuÈckenmarks. Stuttgart: Verlag von Ferdinand Enke; 1898. p. 111–25.
National Spinal Cord Injury Statistical Center. 2020 Annual statistical report for the spinal cord injury model systems—complete public version. Birmingham, Alabama: University of Alabama at Birmingham; 2020.
Bonfield CM, Levi AD, Arnold PM, Okonkwo DO. Surgical management of post-traumatic syringomyelia. Spine. 2010;35:S245–58.
Krebs J, Koch HG, Hartmann K, Frotzler A. The characteristics of posttraumatic syringomyelia. Spinal Cord. 2016;54:463–6.
Kim HG, Oh HS, Kim TW, Park KH. Clinical features of post-traumatic syringomyelia. Korean J Neurotrauma. 2014;10:66–9.
Anton HA, Schweigel JF. Posttraumatic syringomyelia: the British Columbia experience. Spine. 1986;11:865–8.
Asano M, Fujiwara K, Yonenobu K, Hiroshima K. Post-traumatic syringomyelia. Spine. 1996;21:1446–53.
Goldstein B, Hammond MC, Stiens SA, Little JW. Posttraumatic syringomyelia: profound neuronal loss, yet preserved function. Arch Phys Med Rehabil. 1998;79:107–12.
Carroll AM, Brackenridge P. Post-traumatic syringomyelia: a review of the cases presenting in a regional spinal injuries unit in the north east of England over a 5-year period. Spine. 2005;30:1206–10.
Lee TT, Arias JM, Andrus HL, Quencer RM, Falcone SF, Green BA, et al. Progressive posttraumatic myelomalacic myelopathy: treatment with untethering and expansive duraplasty. J Neurosurg. 1997;86:624–8.
Rossier AB, Foo D, Shillito J, Dyro FM. Posttraumatic cervical syringomyelia. Incidence, clinical presentation, electrophysiological studies, syrinx protein and results of conservative and operative treatment. Brain. 1985;108:439–61.
Brodbelt AR, Stoodley MA. Post-traumatic syringomyelia: a review. J Clin Neurosci. 2003;10:401–8.
Timpone VM, Patel SH. MRI of a syrinx: is contrast material always necessary? Am J Roentgenol. 2015;204:1082–5.
Ronen J, Catz A, Spasser R, Gepstein R. The treatment dilemma in post-traumatic syringomyelia. Disabil Rehabil. 1999;21:455–7.
Schurch B, Wichmann W, Rossier AB. Post-traumatic syringomyelia (cystic myelopathy): a prospective study of 449 patients with spinal cord injury. J Neurol Neurosurg Psychiatry. 1996;60:61–7.
Klekamp J. Treatment of posttraumatic syringomyelia. J Neurosurg Spine. 2012;17:199–211.
Shannon N, Symon L, Logue V, Cull D, Kang J, Kendall B, et al. Clinical features, investigation and treatment of post-traumatic syringomyelia. J Neurol Neurosurg Psychiatry. 1981;44:35–42.
Tator CH, Meguro K, Rowed DW. Favorable results with syringosubarachnoid shunts for treatment of syringomyelia. J Neurosurg. 1982;56:517–23.
Laxton AW, Perrin RG. Cordectomy for the treatment of posttraumatic syringomyelia. Report of four cases and review of the literature. J Neurosurg Spine. 2006;4:174–8.
Edgar R, Quail P. Progressive post-traumatic cystic and non-cystic myelopathy. Br J Neurosurg. 1994;8:7–22.
Sgouros S, Williams B. A critical appraisal of drainage in syringomyelia. J Neurosurg. 1995;82:1–10.
Cacciola F, Capozza M, Perrini P, Benedetto N, Di Lorenzo N. Syringopleural shunt as a rescue procedure in patients with syringomyelia refractory to restoration of cerebrospinal fluid flow. Neurosurgery. 2009;65:471–6.
Suzuki M, Davis C, Symon L, Gentili F. Syringoperitoneal shunt for treatment of cord cavitation. J Neurol Neurosurg Psychiatry. 1985;48:620–7.
Lam S, Batzdorf U, Bergsneider M. Thecal shunt placement for treatment of obstructive primary syringomyelia. J Neurosurg Spine. 2008;9:581–8.
Falci SP, Indeck C, Lammertse DP. Posttraumatic spinal cord tethering and syringomyelia: surgical treatment and long-term outcome. J Neurosurg Spine. 2009;11:445–60.
Holly LT, Johnson JP, Masciopinto JE, Batzdorf U. Treatment of posttraumatic syringomyelia with extradural decompressive surgery. Neurosurg Focus. 2000;8:E8.
Ushewokunze SO, Gan YC, Phillips K, Thacker K, Flint G. Surgical treatment of post-traumatic syringomyelia. Spinal Cord. 2010;48:710–3.
Kleindienst A, Engelhorn T, Roeckelein V, Buchfelder M. Development of pre-syrinx state and syringomyelia following a minor injury: a case report. J Med Case Rep. 2020;14:223.
Gotsch KE, Annest JL, Mercy JA, Ryan GW. Surveillance for fatal and nonfatal firearm-related injuries—United States, 1993–1998. MMWR. 2001;50:1–32.
McQuirter JL, Rothenberg SJ, Dinkins GA, Manalo M, Kondrashov V, Todd AC. The effects of retained lead bullets on body lead burden. J Trauma. 2001;50:892–9.
Waters RL, Sie IH. Spinal cord injuries from gunshot wounds to the spine. Clin Orthop Relat Res. 2003;408:120–5.
Sidhu GS, Ghag A, Prokuski V, Vaccaro AR, Radcliff KE. Civilian gunshot injuries of the spinal cord: a systematic review of the current literature. Clin Orthop Relat Res. 2013;471:3945–55.
Vernon JD, Silver JR, Ohry A. Post-traumatic syringomyelia. Paraplegia. 1982;20:339–64.
Beckley AO, Oleson CV, Formal CS. Development of syringomyelia from retained bullet fragment following spinal cord injury. Toronto, Canada: American Congress of Rehabilitation Medicine; Department of Rehabilitation Medicine Faculty Papers; 2014.
Wetjen NM, Heiss JD, Oldfield EH. Time course of syringomyelia resolution following decompression of Chiari malformation Type I. J Neurosurg Pediatr. 2008;1:118–23.
Acknowledgements
The authors thank Eleanor Buckle who provided valuable assistance with technical aspects of this project.
Author information
Authors and Affiliations
Contributions
TDA and NT conceived of the presented idea. TDA and JM wrote the manuscript with support from BYH, DM, KRL, LH, LJB, YX, PPS, NVK, and NT. NT supervised the project.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Ethical approval was not required by the Johns Hopkins Medicine Institutional Review Board, as the presented work is a medical/educational activity that does not meet the Department of Health and Human Services definition of “research”, which is: “a systematic investigation, including research development, testing and evaluation, designed to develop or contribute to generalizable knowledge.”
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Azad, T.D., Materi, J., Hwang, B.Y. et al. Spinal cord untethering and midline myelotomy for delayed, symptomatic post-traumatic syringomyelia due to retained ballistic fragments: case report. Spinal Cord Ser Cases 8, 66 (2022). https://doi.org/10.1038/s41394-022-00533-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-022-00533-7