Abstract
Introduction
Cysticercosis, caused by Cysticercus cellulosae, is one of the common parasitic diseases that can affect the central nervous system (neurocysticercosis, NCC). Isolated involvement of cysticercosis of the spine, without the involvement of the brain, has been very rarely reported.
Case presentation
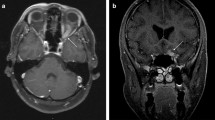
This report presented a case, who was presenting with low back pain with radiation and cauda equina syndrome (CES). On MRI, the patient was found to have a subarachnoid cystic lesion at the level of lumbosacral vertebrae. Under neurosurgery, the patient underwent L5/S1 laminectomy, decompression, and excision of the cyst. On histopathological examination, the patient was diagnosed of having Cysticercosis. Immediately after surgery, the patient had neurological deterioration. However, at the end of 1 year, the patient had significant improvement both neurologically and functionally.
Discussion
Spinal NCC should be considered in the differential diagnosis for a patient, who presents with a cystic lesion in the spinal subarachnoid space. Surgical exploration and excision of the cysts should be conducted not only to establish the diagnosis but also to decompress the cord and peripheral nerves.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Alsina GA, Johnson JP, McBride DQ, Rhoten PRL, Mehringer CM, Stokes JK, et al. Spinal neurocysticercosis. Neurosurg Focus. 2002;12:e8.
Chang KH, Han MH. MRI of CNS parasitic diseases. J Magn Reson Imaging. 1998;8:297–307.
Ciftçi E, Diaz-Marchan PJ, Hayman LA. Intradural-extramedullary spinal cysticercosis: MR imaging findings. Comput Med Imaging Graph. 1999;23:161–4.
Pittella JE. Neurocysticercosis. Brain Pathol. 1997;7:681–93.
DeGiorgio CM, Medina MT, Durón R, Zee C, Escueta SP. Neurocysticercosis. Epilepsy Curr. 2004;4:107–11.
Paterakis KN, Kapsalaki E, Hadjigeorgiou GM, Barbanis S, Fezoulidis I, Kourtopoulos H, et al. Primary spinal intradural extramedullary cysticercosis. Surg Neurol. 2007;68:309–11.
Lopez S, Santillan F, Diaz JJ, Mogrovejo P. Spinal cord compression by multiple cysticercosis. Surg Neurol Int. 2019;10:94.
Colli BO, Assirati Júnior JA, Machado HR, dos Santos F, Takayanagui OM. Cysticercosis of the central nervous system. II. Spinal cysticercosis. Arq Neuropsiquiatr. 1994;52:187–99.
Kishore LT, Gayatri K, Naidu MR, Mateen MA, Dinakar I, Ratnakar KS, et al. Intermedullary spinal cord cysticercosis-a case report and literature review. Indian J Pathol Microbiol. 1991;34:219–21.
White AC, Coyle CM, Rajshekhar V, Singh G, Hauser WA, Mohanty A, et al. Diagnosis and Treatment of Neurocysticercosis: 2017 Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH). Clin Infect Dis. 2018;66:e49–75.
Spector LR, Madigan L, Rhyne A, Darden B, Kim D. Cauda equina syndrome. J Am Acad Orthop Surg. 2008;16:471–9.
Gitelman A, Hishmeh S, Morelli BN, Joseph SA, Casden A, Kuflik P, et al. Cauda equina syndrome: a comprehensive review. Am J Orthop. 2008;37:556–62.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
Kirshblum S, Snider B, Rupp R, Read MS. International Standards Committee of ASIA and ISCoS. Updates of the International Standards for Neurologic Classification of Spinal Cord Injury: 2015 and 2019. Phys Med Rehabil Clin N Am. 2020;31:319–30.
Garcia HH, Del Brutto OH, Cysticercosis Working Group in Peru. Neurocysticercosis: updated concepts about an old disease. Lancet Neurol. 2005;4:653–61.
Del Brutto OH. Neurocysticercosis in Australia: still free of autochthonous cases? Med J Aust. 2012;196:385.
Del Brutto OH. Neurocysticercosis in Western Europe: a re-emerging disease? Acta Neurol Belg. 2012;112:335–43.
Del Brutto OH. A review of cases of human cysticercosis in Canada. Can J Neurol Sci. 2012;39:319–22.
Del Brutto OH. Neurocysticercosis among international travelers to disease-endemic areas. J Travel Med. 2012;19:112–7.
Kelesidis T, Tsiodras S. Extraparenchymal neurocysticercosis in the United States. Am J Med Sci. 2012;344:79–82.
Del Brutto OH. Diagnostic criteria for neurocysticercosis, revisited. Pathog Glob Health. 2012;106:299–304.
Muralidharan V, Nair BR, Patel B, Rajshekhar V. Primary intradural extramedullary cervical spinal cysticercosis. World Neurosurg. 2017;106:1052.e5–11.
Pal A, Biswas C, Ghosh TR, Deb P. A rare case of recurrence of primary spinal neurocysticercosis mimicking an arachnoid cyst. Asian J Neurosurg. 2017;12:250–2.
Sperlescu A, Balbo RJ, Rossitti SL. Brief comments on the pathogenesis of spinal cysticercosis. Arq Neuropsiquiatr. 1989;47:105–9.
Jang JW, Lee JK, Lee JH, Seo BR, Kim SH. Recurrent primary spinal subarachnoid neurocysticercosis. Spine. 2010;35:E172–5.
Jongwutiwes U, Yanagida T, Ito A, Kline SE. Isolated intradural-extramedullary spinal cysticercosis: a case report. J Travel Med. 2011;18:284–7.
Bansal S, Suri A, Sharma MC, Kakkar A. Isolated lumbar intradural extra medullary spinal cysticercosis simulating tarlov cyst. Asian J Neurosurg. 2017;12:279–82.
García HH, Evans CAW, Nash TE, Takayanagui OM, White AC, Botero D, et al. Current consensus guidelines for treatment of neurocysticercosis. Clin Microbiol Rev. 2002;15:747–56.
Author information
Authors and Affiliations
Contributions
All authors participated in drafting of the paper, and critical revision of the article. All authors approved the final version of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Institutional ethical committee approval was received.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Roy, S.S., Barman, A., Viswanath, A. et al. Isolated neurocysticercosis of the spine presenting with low back pain and cauda equina syndrome: a case report. Spinal Cord Ser Cases 8, 70 (2022). https://doi.org/10.1038/s41394-022-00535-5
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41394-022-00535-5