Abstract
Introduction
After spinal cord injury, further neurological deterioration up to one to two neurological levels is not uncommon. Late neurological deterioration can occur after two months, mainly due to the syrinx formation. In a rare case like in sub-acute post-traumatic ascending myelopathy, the neurological level may ascend more than four levels from the initial level of injury and it usually starts within a few weeks after injury.
Case presentation
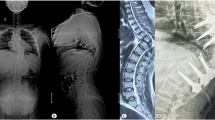
Our case was diagnosed as a case of traumatic spinal cord injury having a lower thoracic neurological level of injury initially, which rapidly progressed over a few weeks into a higher thoracic neurological level. He was operated with pedicle screw fixation of the spine before admission to rehabilitation unit. He was having progressive ascending neurological deterioration, starting a few days after surgery, which was evident by the progression of neurological level by more than four segments clinically. Cerebrospinal fluid(CSF) study showed no significant abnormality. Magnetic resonance imaging (MRI) study showed involvement of the spinal cord at the upper thoracic region. Patient was monitored to note any further worsening. Rehabilitation and supportive measures were provided according to standard protocol.
Discussion
Very few cases of ascending paralysis of more than four levels have been reported globally. It results in increased morbidity and mortality in spinal cord injury patients. In our case few possible reasons are ruled out but the actual underlying reason was not clear. Various hypotheses have been proposed as the cause in previous published literatures. Management is mostly supportive.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
Data regarding this case report can be made available with maintaining patient’s privacy by requesting the corresponding author through provided e-mail.
References
Mathur N, Jain S, Kumar N, Srivastava A, Purohit N, Patni A, et al. Spinal cord injury: scenario in an Indian state. Spinal Cord. 2015;53:349–52. https://doi.org/10.1038/sc.2014.153
Harrop JS, Sharan AD, Vaccaro AR, Przybylski GJ. The cause of neurologic deterioration after acute cervical spinal cord injury. Spine. 2001;26:340–6. https://doi.org/10.1097/00007632-200102150-00008
Yablon IG, Ordia J, Mortara R, Reed J, Spatz E. Acute ascending myelopathy of the spine. Spine. 1989;14:1084–9. https://doi.org/10.1097/00007632-198910000-00010
Fehlings MG, Austin JW. Posttraumatic syringomyelia. J Neurosurg Spine. 2011;14:570–2. https://doi.org/10.3171/2010.4.SPINE1047
Lee TT, Arias JM, Andrus HL, Quencer RM, Falcone SF, Green BA, et al. Progressive posttraumatic myelomalacic myelopathy: treatment with untethering and expansive duraplasty. J Neurosurg. 1997;86:624–8. https://doi.org/10.3171/jns.1997.86.4.0624
Belanger E, Picard C, Lacerte D, Lavallee P, Levi AD. Subacute posttraumatic ascending myelopathy after spinal cord injury. Report of three cases. J Neurosurg. 2000;93:294–9. https://doi.org/10.3171/spi.2000.93.2.0294
Planner AC, Pretorius PM, Graham A, Meagher TM. Subacute progressive ascending myelopathy following spinal cord injury: MRI appearances and clinical presentation. Spinal Cord. 2008;46:140–4. https://doi.org/10.1038/sj.sc.3102056
Frankel H. Ascending cord lesion in the early stages following spinal injury. Spinal Cord. 1969;7:111–8. https://doi.org/10.1038/sc.1969.21
Zhang J, Wang G. Subacute posttraumatic ascending myelopathy: a literature review. Spinal cord. 2017;55:644–50. https://doi.org/10.1038/sc.2016.175
Fletcher ND, Ruska T, Austin TM, Guisse NF, Murphy JS, Bruce RW Jr., et al. Postoperative dexamethasone following posterior spinal fusion for adolescent idiopathic scoliosis. J Bone Jt Surg Am. 2020;102:1807–13. https://doi.org/10.2106/JBJS.20.00259.
Canbay S, Gürer B, Bozkurt M, Comert A, Izci Y, Başkaya MK, et al. Anatomical relationship and positions of the lumbar and sacral segments of the spinal cord according to the vertebral bodies and the spinal roots. Clin Anat. 2014;27:227–33. https://doi.org/10.1002/ca.22253
Kumar A, Kumar J, Garg M, Farooque K, Gamanagatti S, Sharma V. Posttraumatic subacute ascending myelopathy in a 24-year-old male patient. Emerg Radiol. 2010;17:249–52. https://doi.org/10.1007/s10140-009-0832-8
Schmidt BJ. Subacute delayed ascending myelopathy after low spine injury: case report and evidence of a vascular mechanism. Spinal Cord. 2006;44:322–5. https://doi.org/10.1038/sj.sc.3101801
Al-Ghatany M, Al-Shraim M, Levi AD, Midha R. Pathological features including apoptosis in subacute posttraumatic ascending myelopathy. Case report and review of the literature. J Neurosurg Spine. 2005;2:619–23. https://doi.org/10.3171/spi.2005.2.5.0619
Doherty JG, Burns AS, O’Ferrall DM, Ditunno JF Jr. Prevalence of upper motor neuron vs lower motor neuron lesions in complete lower thoracic and lumbar spinal cord injuries. J Spinal Cord Med. 2002;25:289–92. https://doi.org/10.1080/10790268.2002.11753630
Gensicke H, Datta AN, Dill P, Schindler C, Fischer D. Increased incidence of Guillain-Barré syndrome after surgery. Eur J Neurol. 2012;19:1239–44. https://doi.org/10.1111/j.1468-1331.2012.03730.x
Al-Hashel JY, John JK, Vembu P. Unusual presentation of Guillain-Barré syndrome following traumatic bone injuries: report of two cases. Med Princ Pract. 2013;22:597–9. https://doi.org/10.1159/000348797
Acknowledgements
We thank to all faculty members and residents of Department of Physical Medicine and Rehabilitation, AIIMS, Patna for their support in care of the patient and data acquisition.
Author information
Authors and Affiliations
Contributions
AB identified the case and particular findings, conceptualized the manuscript, searched literature and wrote the manuscript; SKP reviewed the examination and investigations, determined management protocol and responsible for reviewing the manuscript; AKG helped in patient care, conceptualized the manuscript, helped in writing discussion and gave feedback for modifications of manuscript; JP examined the patient and acquired data and photographs; SG examined the patient and acquired data and helped in writing the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Biswas, A., Pandey, S.K., Gupta, A.K. et al. Very rare incidence of ascending paralysis in a patient of traumatic spinal cord injury: a case report. Spinal Cord Ser Cases 8, 69 (2022). https://doi.org/10.1038/s41394-022-00536-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-022-00536-4
This article is cited by
-
Response to: Very rare incidence of ascending paralysis in a patient of traumatic spinal cord injury: a case report
Spinal Cord Series and Cases (2023)