Abstract
Introduction
Cauda equina syndrome (CES) is most caused by lumbar disc herniation, and the associated treatment involves prompt surgical decompression. Rarer causes of CES include perineural (Tarlov) cysts.
Clinical presentation
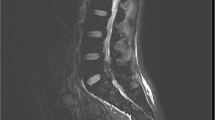
A 62-year-old female with history of rheumatoid arthritis, hip and knee replacements, and chronic low back pain presented with worsening back pain, left leg weakness and pain for 6 weeks, and bowel/bladder incontinence with diminished sensation in the perianal region for 24 h prior to presentation. MRI demonstrated severe spinal stenosis at L4-S1, central disc herniation at L5-S1, and compression of the cauda equina, consistent with CES. A lumbar decompression was performed. Patient did well at 2-week follow up, but presented 5 weeks post-discharge with increased left leg pain/weakness and genitalia anesthesia. Imaging was unremarkable. Two months later, the patient presented with diminished sensation in the buttocks and bilateral lower extremities and bowel/bladder incontinence. Imaging demonstrated a large cystic presacral mass with involvement of the left sciatic foramen and S3 neural foramen. A team of plastic, orthopedic, and neurological surgeons performed an S3 sacral laminectomy, foraminotomy, partial sacrectomy, and S3 rhizotomy, and excision of the large left hemorrhagic pudendal mass. Final pathology demonstrated a perineural cyst with organizing hemorrhage. On follow-up, the patient’s pain and weakness improved.
Conclusion
CES-like symptoms were initially attributed to a herniated disk. However, lumbar decompression did not resolve symptoms, prompting further radiographic evaluation at two separate presentations. This represents the first reported case of a pudendal tumor causing symptoms initially attributed to a herniated disc.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Change history
20 September 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41394-022-00547-1
References
Quaile A. Cauda equina syndrome-the questions. Int Orthop. 2019;43:957–61. https://doi.org/10.1007/s00264-018-4208-0.
Spector LR, Madigan L, Rhyne A, Darden B, Kim D. Cauda equina syndrome. J Am Acad Orthop Surg. 2008;16:471–9. https://doi.org/10.5435/00124635-200808000-00006.
Thakur JD, Storey C, Kalakoti P, Ahmed O, Dossani RH, Menger RP., et al. Early intervention in cauda equina syndrome associated with better outcomes: a myth or reality? Insights from the Nationwide Inpatient Sample database (2005-11). Spine J. 2017;17:1435–48. https://doi.org/10.1016/j.spinee.2017.04.023.
Klepinowski T, Orbik W, Sagan L. Global incidence of spinal perineural Tarlov’s cysts and their morphological characteristics: a meta-analysis of 13,266 subjects. Surg Radio Anat. 2021;43:855–63. https://doi.org/10.1007/s00276-020-02644-y.
Lim VM, Khanna R, Kalinkin O, Castellanos ME, Hibner M. Evaluating the discordant relationship between Tarlov cysts and symptoms of pudendal neuralgia. Am J Obstet Gynecol. 2020;222:70.e1–6. https://doi.org/10.1016/j.ajog.2019.07.021.
Langdown AJ, Grundy JRB, Birch NC. The clinical relevance of Tarlov cysts. J Spinal Disord Tech. 2005;18:29–33. https://doi.org/10.1097/01.bsd.0000133495.78245.71.
Acosta FL, Quinones-Hinojosa A, Schmidt MH, Weinstein PR. Diagnosis and management of sacral Tarlov cysts. Case report and review of the literature. Neurosurg Focus. 2003;15:E15. https://doi.org/10.3171/foc.2003.15.2.15.
Elsawaf A, Awad TE, Fesal SS. Surgical excision of symptomatic sacral perineurial Tarlov cyst: case series and review of the literature. Eur Spine J. 2016;25:3385–92. https://doi.org/10.1007/s00586-016-4584-3.
Mazzola CR, Power N, Bilsky MH, Robert R, Guillonneau B. Pudendal schwannoma: a case report and literature review. Can Urol Assoc J. 2014;8:E199–203. https://doi.org/10.5489/cuaj.1734.
Tschugg A, Tschugg S, Hartmann S, Rhomberg P, Thomé C. Far caudally migrated extraforaminal lumbosacral disc herniation treated by a microsurgical lateral extraforaminal transmuscular approach: case report. J Neurosurg Spine. 2016;24:385–8. https://doi.org/10.3171/2015.7.SPINE15342.
Long B, Koyfman A, Gottlieb M. Evaluation and management of cauda equina syndrome in the emergency department. Am J Emerg Med. 2020;38:143–8. https://doi.org/10.1016/j.ajem.2019.158402.
Author information
Authors and Affiliations
Contributions
All authors reviewed and provided approval on this case report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The patient signed a consent for use of her records for deidentified research purposes.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mahajan, U.V., Labak, K.B., Labak, C.M. et al. Pudendal tumor mimicking cauda equina syndrome and acute radiculopathy: case report. Spinal Cord Ser Cases 8, 71 (2022). https://doi.org/10.1038/s41394-022-00537-3
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41394-022-00537-3