Abstract
Study design
Longitudinal.
Objective
With an increased risk of depression in spinal cord injury, the study longitudinally examines depression to understand how post-injury autonomic regulation and coping might be related to somatic and cognitive manifestations of depression after 3 years.
Setting
Indian Spinal Injuries Center.
Methods
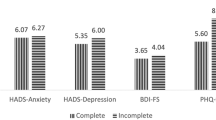
Twenty-eight spinal cord injury participants completed the follow-up assessment of the Patient Health Questionnaire 3 years post-injury. The participants were grouped based on post-injury autonomic regulation (high and low HRV) and the somatic and cognitive manifestation of depression reflected in a depression ratio. Wilcoxson signed-rank test tested the post-injury (T1) and 3 year follow–up (T2) depression scores.
Results
Depression score reduced after 3 years of injury (p ≤ 0.05). Only the high HRV group showed a higher depression ratio (somatic/ cognitive) atfollow-up (T2) (p ≤ 0.05). No difference was observed in post-injury coping between high and low HRV groups.
Conclusion
The reduced depression score at follow-up (T2) aligns with the ‘disability paradox’ and mightindicate cognitive adaptation, specifically for those who showed autonomic adaptability in the form of post-injury high autonomic variability.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated during and analyzed during the current study are not publicly available to maintain confidentiality as they contain information regarding spinal cord injury patients’ mental well-being. However, these are available from the corresponding author on reasonable request.
References
Williams R, Murray A Prevalence of depression after spinal cord injury: A meta-analysis. Arch Phys Med Rehabil [Internet]. Elsevier Ltd; 2015;96:133–40. https://doi.org/10.1016/j.apmr.2014.08.016.
Craig AR, Hancock KM, Dickson HG. Spinal cord injury: A search for determinants of depression two years after the event. Br J Clin Psychol. 1994;33:221–30.
Craig A, Tran Y, Middleton J. Psychological morbidity and spinal cord injury: A systematic review. Spinal Cord. 2009;47:108–14.
Hoffman JM, Bombardier CH, Graves DE, Kalpakjian CZ, Krause JS. A longitudinal study of depression from 1 to 5 years after spinal cord injury. Arch Phys Med Rehabil [Internet]. Elsevier Inc. 2011;92:411–8. https://doi.org/10.1016/j.apmr.2010.10.036.
Arango-Lasprilla JC, Ketchum JM, Starkweather A, Nicholls E, Wilk AR. Factors predicting depression among persons with spinal cord injury 1 to 5 years post injury. NeuroRehabilitation. 2011;29:9–21.
Bonanno GA, Kennedy P, Galatzer-Levy IR, Lude P, Elfström ML. Trajectories of resilience, depression, and anxiety following spinal cord injury. Rehabil Psychol. 2012;57:236–47.
Saunders LL, Krause JS, Focht KL. A longitudinal study of depression in survivors of spinal cord injury. Spinal Cord. 2012;50:72–7. https://pubmed.ncbi.nlm.nih.gov/21808257/
Bombardier CH, Adams LM, Fann JR, Hoffman JM. Depression trajectories during the first year after spinal cord injury. Arch Phys Med Rehabil. 2016;97:196–203.
Craig A, Nicholson Perry K, Guest R, Tran Y, Dezarnaulds A, Hales A, et al. Prospective Study of the Occurrence of Psychological Disorders and Comorbidities after Spinal Cord Injury. Arch Phys Med Rehabil [Internet]. Elsevier Ltd; 2015;96:1426–34. https://doi.org/10.1016/j.apmr.2015.02.027.
Lim S-W, Shiue Y-L, Ho C-H, Yu S-C, Kao P-H, Wang J-J, et al. Anxiety and depression in patients with traumatic spinal cord injury: a nationwide population-based cohort study. PLoS One. 2017;12:e0169623. https://doi.org/10.1371/journal.pone.0169623.
Singh R, Rohilla RK, Siwach R, Dhankar SS, Kaur K. Understanding psycho-social issues in persons with spinal cord injury and impact of remedial measures. Int J Psychosoc Rehabil. 2011;16:104–11.
Arafat S, Ahmed S, Ahmed F, Zaman S, Andalib A. Depression in spinal cord injury patients: a cross-sectional observation with PHQ-9 in a rehabilitation center of Bangladesh. J Behav Heal. 2017;7:1.
Krause JS, Reed KS, McArdle JJ. Prediction of somatic and non-somatic depressive symptoms between inpatient rehabilitation and follow-up. Spinal Cord [Internet]. Spinal Cord. 2010;48:239–44. https://pubmed.ncbi.nlm.nih.gov/19736559/
Krause JS, Reed KS, McArdle JJ Factor structure and predictive validity of somatic and nonsomatic symptoms from the patient health questionnaire-9: A longitudinal study after spinal cord injury. Arch Phys Med Rehabil [Internet]. Elsevier Inc. 2010;91:1218–24. https://doi.org/10.1016/j.apmr.2010.04.015.
Richardson EJ, Richards JS. Factor structure of the PHQ-9 screen for depression across time since injury among persons with spinal cord. Injury 2008;53:243–9.
Elfström ML, Kreuter M, Rydén A, Persson LO, Sullivan M. Effects of coping on psychological outcome when controlling for background variables: A study of traumatically spinal cord lesioned persons. Spinal Cord. 2002;40:408–15.
Pollard C, Kennedy P. A longitudinal analysis of emotional impact, coping strategies and post-traumatic psychological growth following spinal cord injury: A 10-year review. Br J Health Psychol. 2007;12:347–62.
Beauchaine TP. Respiratory sinus arrhythmia: A transdiagnostic biomarker of emotion dysregulation and psychopathology. Curr Opin Psychol. 2015;3:43–7.
Koch C, Wilhelm M, Salzmann S, Rief W, Euteneuer F. A meta-analysis of heart rate variability in major depression. Psychol Med. 2019;49:1948–57. https://doi.org/10.1017/S0033291719001351.
Kemp AH, Quintana DS, Gray MA, Felmingham KL, Brown K, Gatt JM, et al. Impact of Depression and Antidepressant Treatment on Heart Rate Variability: A Review and Meta-Analysis. Biol Psychiatry [Internet]. Elsevier Inc. 2010;67:1067–74. https://doi.org/10.1016/j.biopsych.2009.12.012.
Mitra S, Singh V. Autonomic dysregulation and low heart rate variability in spinal cord injury(SCI): A marker for depression. Int J Physiother. 2020;7:108–13.
Singh V, Mitra S. Psychophysiological impact of spinal cord injury: Depression, coping and heart rate variability. J Spinal Cord Med [Internet]. 2022;0:1–9. https://doi.org/10.1080/10790268.2022.2052503.
Migliorini C, Tonge B. Reflecting on subjective well-being and spinal cord injury. J Rehabil Med. 2009;41:445–50.
Albrecht GL, Devlieger PJ. The disability paradox: highly qualified of life against all odds. Soc Sci Med. 1999;48:977–88.
Kalpakjian CZ, Toussaint LL, Albright KJ, Bombardier CH, Krause JK, Tate DG, et al. Patient health questionnaire-9 in spinal cord injury: An examination of factor structure as related to gender. J Spinal Cord Med. 2009;32:147–56.
Elfström ML, Rydén A, Kreuter M, Persson LO, Sullivan M. Linkages between coping and psychological outcome in the spinal cord lesioned: Development of SCL-related measures. Spinal Cord. 2002;40:23–9.
Malik M, Bigger JT, Camm AJ, Kleiger RE, Malliani A, Moss AJ. et al. Task force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability standards of measurement, physiological interpretation, and clinical use. Eur Heart J. 1996;17:354–81.
Koch C, Wilhelm M, Salzmann S, Rief W, Euteneuer F A meta-Analysis of heart rate variability in major depression. Psychol Med. Cambridge University Press; 2019;49:1948–57.
Ditor DS, Kamath MV, MacDonald MJ, Bugaresti J, McCartney N, Hicks AL. Reproducibility of heart rate variability and blood pressure variability in individuals with spinal cord injury. Clin Auton Res. 2005;15:387–93.
Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13.
Thayer JF, Hansen AL, Saus-rose E, Psychol C, Johnsen BH. Heart rate variability, prefrontal neural function, and cognitive performance: the neurovisceral integration perspective on self-regulation, adaptation, and health. Ann Behav Med. 2009;37:141–53.
Kennedy P, Marsh N, Lowe R, Grey N, Short E, Rogers B. A longitudinal analysis of psychological impact and coping strategies following spinal cord injury. Br J Health Psychol. 2000;5:157–72.
Acknowledgements
We acknowledge all the Spinal cord injury participants for their participation.
Author information
Authors and Affiliations
Contributions
Conception or design of the work, data analysis and interpretation, drafting the article, critical revision of the article, final approval of the version to be published: VS and SM. Data collection: SM.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singh, V., Mitra, S. Autonomic variability, depression and the disability paradox in spinal cord injury. Spinal Cord Ser Cases 8, 76 (2022). https://doi.org/10.1038/s41394-022-00542-6
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41394-022-00542-6
This article is cited by
-
Delayed Withdrawal of Life-Sustaining Treatment in Disorders of Consciousness: Practical and Theoretical Considerations
Neurocritical Care (2025)
-
A Systematic Review of the Impact of Spinal Cord Injury on Costs and Health-Related Quality of Life
PharmacoEconomics - Open (2024)