Abstract
Study design
Single-subject-research-design.
Objectives
To improve seated postural control in a participant with spinal cord injury (SCI) with a robotic Trunk-Support-Trainer (TruST).
Setting
Laboratory.
Methods
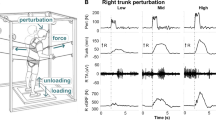
TruST delivered “assist-as-needed” forces on the participant’s torso during a motor learning-and-control-based intervention (TruST-intervention). TruST-assistive forces were progressed and matched to the participant’s postural trunk control gains across six intervention sessions. The T-shirt test was used to capture functional improvements while dressing the upper body. Kinematics were used to compute upper body excursions (cm) and velocity (cm2), and sitting workspace area (cm2). Functional trunk dynamometry was used to examine muscle force (Kg). Surface electromyography (sEMG) was applied to measure trunk muscle activity. The Borg Rating of Perceived Exertion (RPE) was used to monitor physical exertion during TruST-intervention. A two-standard-deviation bandwidth method was adopted for data interpretation.
Results
After TruST-intervention, the participant halved the time needed to don and doff a T-shirt, increased muscle force of trunk muscles (mean = 3 kg), acquired a steadier postural sitting control without vision (mean excursion baseline: 76.0 ± 2 SD = 5.25 cm and post-intervention: 44.1 cm; and mean velocity baseline: 3.0 ± 2 SD = 0.2 cm/s and post-intervention: 1.8 cm/s), and expanded his sitting workspace area (mean baseline: 36.7 ± 2 SD = 36.6 cm2 and post-intervention: 419.2 cm2). The participant increased his tolerance to counteract greater TruST-force perturbations in lateral and posterior directions. Furthermore, abdominal muscle activity substantially augmented after completion of TruST-intervention across all perturbation directions.
Conclusions
Our data indicate a potential effectiveness of TruST-intervention to promote functional sitting in SCI.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The data that support the findings of this study will be available on request from the corresponding author, SA.
References
Chen Y, He Y, DeVivo MJ. Changing demographics and injury profile of new traumatic spinal cord injuries in the United States, 1972–2014. Arch Phys Med Rehabil. 2016;97:1610–9.
Tederko P, Middleton J, Mycielski J, Joseph C, Pagliacci MC, Rapidi CA, et al. Relationship between level of economic development, age, and etiology of spinal cord injury: a cross-sectional survey from 22 countries. Arch Phys Med Rehabil. 2021;102:1947–58.
Fulk GD, Behrman AL, Schmitz TJ. Traumatic spinal cord injury. In: O’Sullivan SB, Schmitz TJ, Fulk GD, editors. Physical rehabilitation. Philadelphia: F.A. Davis Company PA; 2014. p. 889–964.
Carpenter C, Forwell SJ, Jongbloed LE, Backman CL. Community participation after spinal cord injury. Arch Phys Med Rehabil. 2007;88:427–33.
Panjabi M, Albumi K, Duranceau J, Oxland T. Spinal stability and intersegmental muscle forces. A bimechanical model. Spine. 1989;14:194–200.
Park RJ, Tsao H, Cresswell AG, Hodges PW. Anticipatory postural activity of the deep trunk muscles differs between anatomical regions based on their mechanical advantage. Neuroscience. 2014;261:161–72.
Chiou SY, Gottardi SEA, Hodges PW, Strutton PH. Corticospinal excitability of trunk muscles during different postural tasks. PLoS ONE. 2016;11:1–13.
Gurfinkel V, Cacciatore TW, Cordo P, Horak F, Nutt J, Skoss R, et al. Humans postural muscle tone in the body axis of healthy the influence of education and exercise on neck pain transition from sitting to standing. J Neurophysiol. 2006;96:2678–87.
Santamaria V, Luna T, Khan M, Agrawal S. The robotic Trunk-Support-Trainer (TruST) to measure and increase postural workspace during sitting in people with spinal cord injury. Spinal Cord Ser Cases. 2020;6:1–7.
Chen CL, Yeung KT, Bih LI, Wang CH, Chen MI, Chien JC, et al. The relationship between sitting stability and functional performance in patients with paraplegia. Arch Phys Med Rehabil. 2003;84:1276–81.
Serra-Añó P, Pellicer-Chenoll M, Garcia-Massó X, Brizuela G, García-Lucerga C, González Moreno LM, et al. Sitting balance and limits of stability in persons with paraplegia. Spinal Cord. 2013;51:267–72.
Moynahan M. Postural responses during standing in subjects with spinal-cord injury. Gait Posture. 1995;3:156–65.
Rath M, Vette AH, Ramasubramaniam S, Li K, Burdick J, Edgerton VR, et al. Trunk stability enabled by noninvasive spinal electrical stimulation after spinal cord injury. J Neurotrauma. 2018;35:2540–53.
Martin Moraud E, von Zitzewitz J, Miehlbradt J, Wurth S, Formento E, DiGiovanna J, et al. Closed-loop control of trunk posture improves locomotion through the regulation of leg proprioceptive feedback after spinal cord injury. Sci Rep. 2018;8:1–12.
Asboth L, Friedli L, Beauparlant J, Martinez-Gonzalez C, Anil S, Rey E, et al. Cortico–reticulo–spinal circuit reorganization enables functional recovery after severe spinal cord contusion. Nat Neurosci. 2018;21:576–88.
Angeli CA, Boakye M, Morton RA, Vogt J, Benton K, Chen Y, et al. Recovery of over-ground walking after chronic motor complete spinal cord injury. N Engl J Med. 2018;379:1244–50.
Roy RR, Harkema SJ, Edgerton VR. Basic concepts of activity-based interventions for improved recovery of motor function after spinal cord injury. Arch Phys Med Rehab. 2012;93:1487–97.
Boswell-Ruys C, Harvey L, Barker J, Ben M, Middleton J, Lord S, et al. Training unsupported sitting in people with chronic spinal cord injuries: a randomized controlled trial. Spinal Cord. 2010;48:138–43.
Lotter JK, Henderson CE, Plawecki A, Holthus ME, Lucas EH, Ardestani MM, et al. Task-specific versus impairment-based training on locomotor performance in individuals with chronic spinal cord injury: a randomized crossover study. Neurorehabil Neural Repair. 2020;34:627–39.
Ragnarsson KT. Functional electrical stimulation after spinal cord injury: current use, therapeutic effects and future directions. Spinal Cord. 2008;46:255–74.
Marchesi G, Ricaldone E, De Luca A, Torre K, Quinland E, Bellitto A, et al. A robot-based assessment of trunk control in spinal cord injured athletes. In: 2020 8th IEEE RAS/EMBS International Conference for Biomedical Robotics and Biomechatronics (BioRob); 2020. p. 497–502.
Eizad A, Lee H, Pyo S, Afzal MR, Lyu SK, Yoon J. A novel trunk rehabilitation robot based evaluation of seated balance under varying seat surface and visual conditions. IEEE Access. 2020;8:204902–13.
Santamaria V, Luna TD, Agrawal SK. Feasibility and tolerance of a robotic postural training to improve standing in a person with ambulatory spinal cord injury. Spinal Cord Ser Cases. 2021;7:1–9.
Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M, et al. Reference for the 2011 revision of the international standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2011;34:547–54.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT, et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord. 2007;45:275–91.
Ditunno PL, Ditunno JF. Walking index for spinal cord injury (WISCI II): scale revision. Spinal Cord. 2001;39:654–6.
Abou L, Ribeiro de Freitas G, Palandi J, Ilha J. Clinical instruments for measuring unsupported sitting balance in subjects with spinal cord injury: a systematic review. Top Spinal Cord Inj Rehabil. 2018;24:177–93.
Borg G. Psychophysical bases of perceived exertion. Med Sci Sport Exerc. 1982;14:377–81.
Perdices M, Tate RL. Single-subject designs as a tool for evidence-based clinical practice: are they unrecognised and undervalued? Neuropsychol Rehabil. 2009;19:904–27.
de Leva P. Adjustments to Zatsiorsky-Seluyanov’s segment inertia parameters. J Biomech. 1996;29:1223–30.
Spratt J. Thorax. In: Standring S (ed). Gray’s Anatomy: The Anatomical Basis of Clinical Practice (40th edition). Churchill Livingstone/Elsevier, Edinburgh: 2008, pp 953–975.
Khan MI, Santamaria V, Kang J, Bradley BM, Dutkowsky JP, Gordon AM, et al. Enhancing seated stability using trunk support trainer (TruST). IEEE Robot Autom Lett. 2016;2:1609–16.
Santamaria V, Khan M, Luna T, Kang J, Dutkowsky J, Gordon AM, et al. Promoting functional and independent sitting in children with cerebral palsy using the robotic trunk support trainer. IEEE Trans Neural Syst Rehabil Eng. 2020;28:2995–3004.
Khan M, Santamaria V, Agrawal S. Improving trunk-pelvis stability using active force control at the trunk and passive resistance at the pelvis. IEEE Robot Autom Lett. 2018;3:2569–75.
Gribble PA, Hertel J, Facsm À, Plisky P. Using the star excursion balance test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012;47:339–57.
Gao KL, Chan KM, Purves S, Tsang WWN. Reliability of dynamic sitting balance tests and their correlations with functional mobility for wheelchair users with chronic spinal cord injury. J Orthop Transl. 2015;3:44–49.
Quinzaños J, Villa AR, Flores AA, Pérez R. Proposal and validation of a clinical trunk control test in individuals with spinal cord injury. Spinal Cord. 2014. https://doi.org/10.1038/sc.2014.34.
Shumway-Cook A, Woollacott MH. Postural control. In: Motor control: translating research into clinical practice. Philadelphia, PA: Wolters Kluwer; 2017. p. 153–82.
Santamaria V, Rachwani J, Saussez G, Bleyenheuft Y, Dutkowsky J, Gordon AM, et al. The seated postural & reaching control test in cerebral palsy: a validation study. Phys Occup Ther Pediatr. 2020;40:441–69.
Gordon AM, Hung Y-C, Brandao M, Ferre CL, Kuo H-C, Friel K, et al. Bimanual training and constraint-induced movement therapy in children with hemiplegic cerebral palsy. Neurorehabil Neural Repair. 2011;25:692–702.
Bleyenheuft Y, Ebner-Karestinos D, Surana B, Paradis J, Sidiropoulos A, Renders A, et al. Intensive upper- and lower-extremity training for children with bilateral cerebral palsy: a quasi-randomized trial. Dev Med Child Neurol. 2017;59:625–33.
Behrman A, Argetsinger L, Roberts M, Stout D, Thompson J, Ugiliweneza B, et al. Activity-based therapy targeting neuromuscular capacity after pediatric-onset spinal cord injury. Top Spinal Cord Inj Rehabil. 2019;25:132–49.
Sayenko DG, Alekhina MI, Masani K, Vette AH, Obata H, Popovic MR, et al. Positive effect of balance training with visual feedback on standing balance abilities in people with incomplete spinal cord injury. Spinal Cord. 2010;48:886–93.
Tse CM, Chisholm AE, Lam T, Eng JJ. A systematic review of the effectiveness of task-specific rehabilitation interventions for improving independent sitting and standing function in spinal cord injury. J Spinal Cord Med. 2018;41:254–66.
Hung YC, Brandão MB, Gordon AM. Structured skill practice during intensive bimanual training leads to better trunk and arm control than unstructured practice in children with unilateral spastic cerebral palsy. Res Dev Disabil. 2017;60:65–76.
Mentiplay BF, Perraton LG, Bower KJ, Adair B, Pua YH, Williams GP, et al. Assessment of lower limb muscle strength and power using hand-held and fixed dynamometry: a reliability and validity study. PLoS ONE. 2015;10:1–18.
Al’joboori Y, Hannah R, Lenham F, Borgas P, Kremers CJP, Bunday KL, et al. The immediate and short-term effects of transcutaneous spinal cord stimulation and peripheral nerve stimulation on corticospinal excitability. Front Neurosci. 2021;15:1–17.
Maurer C, Peterka RJ. A new interpretation of spontaneous sway measures based on a simple model of human postural control. J Neurophysiol. 2005;93:189–200.
Windhorst U. Muscle proprioceptive feedback and spinal networks. Brain Res Bull. 2007;73:155–202.
Macefield VG, Knellwolf TP. Functional properties of human muscle spindles. J Neurophysiol. 2018;120:452–67.
Vette AH, Thrasher TA, Sin VW, Masani K, Craven BC, Popovic MR, et al. Responses of the trunk to multidirectional perturbations during unsupported sitting in normal adults. J Appl Biomech. 2010;26:332–40.
Acknowledgements
We thank the valuable collaboration of the participant. This research was funded by NYS research funding DOH01-C31290GG, SKA principal investigator.
Author information
Authors and Affiliations
Contributions
VS, XA, and SA designed the study and analyzed and interpreted the data. During data collection, XA was the bioengineer and VS delivered the motor intervention. VS, XA, and SA collaborated in the write-up and revisions of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Santamaria, V., Ai, X. & Agrawal, S.K. A motor learning-based postural intervention with a robotic trunk support trainer to improve functional sitting in spinal cord injury: case report. Spinal Cord Ser Cases 8, 88 (2022). https://doi.org/10.1038/s41394-022-00554-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41394-022-00554-2