Abstract
Study design
A systematic review.
Objectives
Tuberculous myelitis, an uncommon disorder, often manifests as transverse myelopathy. The majority of the literature comprises isolated case reports, necessitating a systematic review for better understanding and management.
Setting
Uttar Pradesh India.
Methods
Our review followed PRISMA guidelines, searching PubMed, Scopus, Embase, and Google Scholar with no language constraints. Quality assessment of reports was based on selection, ascertainment, causality, and reporting. Data synthesis was qualitative with categorical and continuous data representation.
Results
We analyzed 34 reports describing 39 individuals. The majority (85%) had a duration of illness of one month or less. Upper motor neuron paraparesis was the most common neurological manifestation (69.2%), followed by areflexic paraparesis (15.3%). Paradoxical reactions occurred in 20.5% of cases. Microbiological confirmation was achievable in approximately 77% of cases. Neuroimaging abnormalities were present in 41% of cases, and chest imaging abnormalities in 53.9%. Longitudinally-extensive hyperintensities in cervical and thoracic regions were common spinal imaging abnormalities. Central nervous system tuberculosis was confirmed in 47.7% of cases, while pulmonary and disseminated tuberculosis were each found in 25.6%. Improvement was noted in 87.2% of cases, while 10.3% did not improve or died.
Conclusion
Tuberculous myelitis, is a distinct spinal cord disease. Most cases had microbiological confirmation, and the majority showed improvement with treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 1 print issues and online access
We are sorry, but there is no personal subscription option available for your country.
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
Saylor D. Neurologic complications of tuberculosis. Continuum (Minneap Minn). 2021;27:992–1017. https://doi.org/10.1212/CON.0000000000001005
Donovan J, Thwaites GE, Huynh J. Tuberculous meningitis: where to from here? Curr Opin Infect Dis. 2020;33:259–66. https://doi.org/10.1097/QCO.0000000000000648
Khan MI, Garg RK, Rizvi I, Malhotra HS, Kumar N, Jain A, et al. Tuberculous myelitis: a prospective follow-up study. Neurol Sci. 2022;43:5615–24. https://doi.org/10.1007/s10072-022-06221-6
Jiang Y, Xu X, Guo Z, Liu Y, Lin J, Suo L, et al. Myelitis: a common complication of tuberculous meningitis predicting poor outcome. Front Neurol. 2022;13:830029 https://doi.org/10.3389/fneur.2022.830029
Garg RK, Malhotra HS, Kumar N, Rizvi I, Uniyal U Tuberculous myelitis: a systematic review of published case reports and case series. Prospero 2024 CRD42024520830 Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42024520830
Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015;85:177–89. https://doi.org/10.1212/WNL.0000000000001729
Li R, Zhong X, Qiu W, Wu A, Dai Y, Lu Z, et al. Association between neuromyelitis optica and tuberculosis in a Chinese population. BMC Neurol. 2014;14:33 https://doi.org/10.1186/1471-2377-14-33
Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. 2018;23:60–63.
Della Gatta AN, Rizzo R, Pilu G, Simonazzi G. Coronavirus disease 2019 during pregnancy: a systematic review of reported cases. Am J Obstet Gynecol. 2020;223:36–41.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46. https://doi.org/10.1179/204577211X13207446293695
Ibrahim E, Mohammed KM, Mustafa LH, Ahmed KM, Omer M. Tuberculous myelitis as an unusual presentation of a common disease in Sudan. Authorea Preprints 2024. https://doi.org/10.22541/au.170668319.98707684/v1
Salari M, Zaker Harofte B, Etemadifar M. Longitudinal extensive transverse myelitis due to tuberculosis: a case report. Neuroradiol J. 2023;36:224–8. https://doi.org/10.1177/19714009221122188
Fang L, Gong Y, Han K, Lv Y, Li M, Wang J. Longitudinally extensive transverse myelitis with mycobacterium tuberculosis infection. Acta Neurol Belg. 2023;123:243–6. https://doi.org/10.1007/s13760-021-01723-0
Angel MT, Sivadasan A, Nair AA, Rajakumar P, Nair AV, Joseph T, et al. Drug-resistant tuberculosis, myelitis and MOG antibody. Neuroimmunol Rep. 2022;2:100123 https://doi.org/10.1016/j.nerep.2022.100123
Ranjan S, Dev R, Keisham MD. A sporadic case of holocord tuberculous transverse myelitis with arachnoiditis. Egypt J Radio Nucl Med. 2022;53:252 https://doi.org/10.1186/s43055-022-00937-3
Mantese CE, Lubini R. Froin’s syndrome with tuberculosis myelitis and spinal block. Rev Assoc Med Bras (1992). 2022;68:10–12. https://doi.org/10.1590/1806-9282.20190536
Kamoen O, Bosco K, Libent L, Assenga CE, Mkwizu E, Lyamuya FS, et al. An unusual case of nontraumatic myelopathy in a TB/HIV coinfected patient in Tanzania. Neuroimmunol Rep. 2022;2:100076 https://doi.org/10.1016/j.nerep.2022.100076
Harizi E, Shemsi K, Kola E, Hyseni F, Kola I, Siddique MA, et al. Transverse myelitis in a 26-year-old male with tuberculosis. Radiol Case Rep. 2022;17:3669–73. https://doi.org/10.1016/j.radcr.2022.06.091
Zafar Z, Hafeez MH, Butt M. Elusive tuberculous meningitis with rare neurological complication of longitudinally extensive transverse myelitis: a case report. Spinal Cord Ser Cases. 2021;7:82 https://doi.org/10.1038/s41394-021-00445-y
Van Tuan N, Van Tuan B, Ung HT, Van Thang H, Van Tong H, Thao PN, et al. Longitudinally extensive transverse myelitis combined with tuberculosis meningitis. Med Case Rep. Study Protoc. 2021;2:e0114.
Shantha DW, Yasaratne D, Ralapanawa DM, Jayalath T, Abeyagunawardena S, Dissanayake DM, et al. Tuberculous meningitis complicated with thoracic cord myelitis; a diagnostic conundrum. Sri Lanka J Med. 2021;30:132–7. https://doi.org/10.4038/sljm.v30i1.264
Mohanty NR, Panda B. Central nervous system tuberculosis presenting as a case of myelitis: a rare complication. J Clin Basic Res. 2021;5:1–4. https://doi.org/10.52547/jcbr.5.2.1
Gu LY, Tian J, Yan YP. Concurrent tuberculous transverse myelitis and asymptomatic neurosyphilis: a case report. World J Clin Cases. 2021;9:9645–51. https://doi.org/10.12998/wjcc.v9.i31.9645
Goyal MK, Lal M. Tubercular longitudinally extensive transverse myelitis with lower motor neuron paralysis. Trop Doct. 2021;51:117–9. https://doi.org/10.1177/0049475520956448
Anand KA, Bhowmik KK, Sarkar A, Ghosh R, Mandal A, Swaika B, et al. Tubercular longitudinally extensive transverse myelitis (LETM): an enigma for primary care physicians. J Fam Med Prim Care. 2021;10:1057–60. https://doi.org/10.4103/jfmpc.jfmpc_2101_20
Ramineni KK, Jakkani RK, Swamy BVG, Sravan Kumar M. Pulmonary tuberculosis with longitudinally extensive transverse myelitis. J Neurosci Rural Pr. 2020;11:178–82. https://doi.org/10.1055/s-0039-3402576
Jain R, Anand K, Juneja A. A rare clinical presentation of tuberculous myelitis. Hamdan Med J. 2020;13:254 https://doi.org/10.4103/HMJ.HMJ_33_20
Ortega-Rosales A, Delgado-Torres N, Burneo-Rosales C. A rare neurological complication of tuberculosis: transverse myelitis. IDCases. 2019;17:e00564 https://doi.org/10.1016/j.idcr.2019.e00564
Liu X, Rui M, Lyu L. Tuberculous meningomyelitis in magnetic resonance imaging: a Chinese case report. Eur J Radio Open. 2019;6:284–6. https://doi.org/10.1016/j.ejro.2019.02.006
Elavarasi A, Kasturi N, Mani B. Macular star, and choroidal tubercles: a rare cause of opticospinal syndrome. Can J Neurol Sci. 2019;46:625–7. https://doi.org/10.1017/cjn.2019.45
Rijal S, Adhikari S, House DR. Lower extremity weakness: a rare case of extrapulmonary tuberculosis. Vis J Emerg Med. 2019;14:7–8. https://doi.org/10.1016/j.visj.2018.10.007
Zhang Y, Zhu M, Wang L, Shi M, Deng H. Longitudinally extensive transverse myelitis with pulmonary tuberculosis: two case reports. Medicine (Baltim). 2018;97:e9676 https://doi.org/10.1097/MD.0000000000009676
Alkan G, Emiroǧlu M, Kartal A, Peru H, Koplay M. Occult disseminated tuberculosis with holocord longitudinally extensive transverse myelitis: a rare phenomenon in a child. J Pediatr Neurosci. 2017;12:259–61. https://doi.org/10.4103/jpn.JPN_14_17
Coclitu C, Mergeani A, Parvu T, Rusu O, Ciobotaru A, Bajenaru O, et al. An uncommon cause of longitudinally extensive transverse myelitis. Maedica (Bucur). 2016;11:245–9.
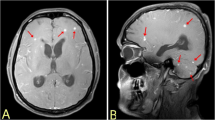
Jain RS, Kumar S, Tejwani S. A rare association of tuberculous longitudinally extensive transverse myelitis (LETM) with brain tuberculoma. Springerplus. 2015;4:476 https://doi.org/10.1186/s40064-015-1232-z
Sahu SK, Giri S, Gupta N. Longitudinal extensive transverse myelitis due to tuberculosis: a report of four cases. J Postgrad Med. 2014;60:409–12. https://doi.org/10.4103/0022-3859.143977
Suda S, Ueda M, Komaba Y, Yamazaki M, Katsumata T, Katayama Y. Tuberculous myelitis diagnosed by elevated adenosine deaminase activity in cerebrospinal fluid. J Clin Neurosci. 2008;15:1068–9. https://doi.org/10.1016/j.jocn.2007.10.006
Lee KH, Ra SW, Park IN, Choi HS, Jung H, Chon GR, et al. A case of transverse myelitis due to multidrug-resistant tuberculosis. Tuberc Respir Dis. 2006;60:353–6. https://doi.org/10.4046/trd.2006.60.3.353
Arméstar F, Coll-Cantí J, Capellades J, Batlle M. Tuberculous myelitis with paraplegia. Med Clin (Barc). 2006;126:556–7. https://doi.org/10.1157/13087147
Shin HJ, Jeon SJ, Kim DK, Ahn KS, Kim HJ, Lee CW. A case of tuberculous myelitis misdiagnosed as lupus myelitis. J Korean Rheum Assoc. 2005;12:154–8
Putruele AM, Legarreta CG, Limongi L, Rossi SE. Tuberculous transverse myelitis: case report and review of the literature. Clin Pulm Med. 2005;12:46–52.
White VL, Al-Shahi R, Gamble E, Brown P, Davison AG. Transverse myelopathy and radiculomyelopathy associated with pulmonary atypical mycobacterium infections. Thorax. 2001;56:158–60. https://doi.org/10.1136/thorax.56.2.158
Von Reyn CF, Mark EJ. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 33-2001. A 33-year-old man with a rash, pulmonary infection, and neurologic disorder. N Engl J Med. 2001;345:1263–9. https://doi.org/10.1056/NEJMcpc332001
Quinlan JJ. A case of tuberculous transverse myelitis. Can Med Assoc J. 1943;48:530–1.
Jarius S, Aktas O, Ayzenberg I, Bellmann-Strobl J, Berthele A, Giglhuber K, et al. Update on the diagnosis and treatment of neuromyelits optica spectrum disorders (NMOSD) - revised recommendations of the Neuromyelitis Optica Study Group (NEMOS). Part I: diagnosis and differential diagnosis. J Neurol. 2023;270:3341–68. https://doi.org/10.1007/s00415-023-11634-0
Dutra BG, da Rocha AJ, Nunes RH, Maia ACM Jr. Neuromyelitis optica spectrum disorders: spectrum of MR imaging findings and their differential diagnosis. Radiographics. 2018;38:169–93. https://doi.org/10.1148/rg.2018170141
Dastur DK. The pathology and pathogenesis of tuberculous encephalopathy and myeloradiculopathy: a comparison with allergic encephalomyelitis. Childs Nerv Syst. 1986;2:13–9. https://doi.org/10.1007/BF00274027
Asundi A, Cervantes-Arslanian AM, Lin NH, Barbosa F. Infectious Myelitis. Semin Neurol. 2019;39:472–81. https://doi.org/10.1055/s-0039-1688923
Author information
Authors and Affiliations
Contributions
RKG: Conceptualization, Methodology, Literature Search, Data Curation, Formal Analysis, Writing—Original Draft, Writing—Review & Editing. NK: Methodology, Literature Search, Data Extraction, Quality Assessment, Writing—Review & Editing. RU: Data Curation, Writing—Review & Editing. PKS: Supervision, Conceptualization, Writing—Review & Editing, Final Approval. HSM: Quality Assessment, Visualization, Writing—Review & Editing. IR: Supervision, Writing—Review & Editing, Final Approval.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
As no human participants were involved in this study, ethical clearance was not required. No human or animal subjects were involved so ethical clearance was not taken.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Garg, R.K., Kumar, N., Uniyal, R. et al. Tuberculous myelitis: a systematic review of published case reports and case series. Spinal Cord Ser Cases 11, 6 (2025). https://doi.org/10.1038/s41394-025-00701-5
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41394-025-00701-5