Abstract
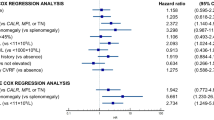
Thiopurines, an effective therapy for Crohn’s disease (CD), often lead to adverse events (AEs). Gene polymorphisms affecting thiopurine metabolism may predict AEs. This retrospective study in CD patients (n = 114) with TPMT activity > 5 Units/Red Blood Cells analyzed TPMT (c.238 G > C, c.460 G > A, c.719 A > G), ITPA (c.94 C > A, IVS2 + 21 A > C), and NUDT15 (c.415 C > T) polymorphisms. All patients received azathioprine (median dose 2.2 mg/kg) with 41.2% experiencing AEs, mainly myelotoxicity (28.1%). No NUDT15 polymorphisms were found, 7% had TPMT, and 31.6% had ITPA polymorphisms. AEs led to therapy modifications in 41.2% of patients. Multivariate analysis identified advanced age (OR 1.046, p = 0.007) and ITPA IVS2 + 21 A > C (OR 3.622, p = 0.015) as independent predictors of AEs. IVS2 + 21 A > C was also associated with myelotoxicity (OR 2.863, p = 0.021). These findings suggest that ITPA IVS2 + 21 A > C polymorphism and advanced age predict AEs during thiopurine therapy for CD with intermediate-normal TPMT activity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Mowat C, Cole A, Windsor A, Ahmad T, Arnott I, Driscoll R, et al. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2011;60:571–607. https://doi.org/10.1136/gut.2010.224154
Chatu S, Subramanian V, Saxena S, Pollok RC. The role of thiopurines in reducing the need for surgical resection in Crohn’s disease: a systematic review and meta-analysis. Am J Gastroenterol. 2012;107:23–34. https://doi.org/10.1038/ajg.2011.401
Peyrin-Biroulet L, Khosrotehrani K, Carrat F, Bouvier AM, Chevaux JB, Simon T, et al. Azathioprine and 6-mercaptopurine for the prevention of postoperative recurrence in Crohn’s disease: a meta-analysis. Am J Gastroenterol. 2009;104:2089–96. https://doi.org/10.1038/ajg.2009.301
Colombel JF, Sandborn WJ, Reinisch W, Mantzaris GJ, Kornbluth A, Rachmilewitz D, et al. Infliximab, azathioprine, or combination therapy for Crohn’s disease. N Engl J Med. 2010;362:1383–95. https://doi.org/10.1056/NEJMoa0904492
Chaparro M, Panés J, García V, Mendoza JL, Bermejo F, López San Román A, et al. Safety of thiopurine therapy in inflammatory bowel disease: Long-term follow-up study of 3931 patients. Inflamm Bowel Dis. 2013;19:1404–10. https://doi.org/10.1097/MIB.0b013e318281f28f
Schwab M, Schäffeler E, Marx C, Fischer C, Lang T, Behrens C, et al. Azathioprine therapy and adverse drug reactions in patients with inflammatory bowel disease: impact of thiopurine S-methyltransferase polymorphism. Pharmacogenetics. 2002;12:429–36. https://doi.org/10.1097/00008571-200208000-00003
Chande N, Laidlaw M, McDonald JW, Macdonald JK. Azathioprine or 6-mercaptopurine for induction of remission in Crohn’s disease. Cochrane Database Syst Rev. 2013;10:CD000545 https://doi.org/10.1002/14651858.CD000545.pub5
Friedman AB, Sparrow MP, Gibson PR. The role of thiopurine metabolites in inflammatory bowel disease and rheumatological disorders. Int J Rheum Dis. 2014;17:132–41. https://doi.org/10.1111/1756-185X.12204
Relling MV, Hancock ML, Rivera GK, Sandlund JT, Ribeiro RC, Krynetski EY, et al. Mercaptopurine therapy intolerance and heterozygosity at the thiopurine S-methyltransferase gene locus. J Natl Cancer Inst. 1999;91:2001–8.
Chouchana L, Narjoz C, Beaune P, Loriot MA, Roblin X. Review article: the benefits of pharmacogenetics for improving thiopurine therapy in inflammatory bowel disease. Aliment Pharmacol Ther. 2012;35:15–36. https://doi.org/10.1111/j.1365-2036.2011.04905.x
Higgs JE, Payne K, Roberts C, Newman WG. Are patients with intermediate TPMT activity at increased risk of myelosuppression when taking thiopurine medications? Pharmacogenomics. 2010;11:177–88. https://doi.org/10.2217/pgs.09.155
Gearry RB, Barclay ML, Burt MJ, Collett JA, Chapman BA, Roberts RL, et al. Thiopurine S-methyltransferase (TPMT) genotype does not predict adverse drug reactions to thiopurine drugs in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2003;18:395–400. https://doi.org/10.1046/j.1365-2036.2003.01690.x
Colombel JF, Ferrari N, Debuysère H, Marteau P, Gendre JP, Bonaz B, et al. Genotypic analysis of thiopurine S-methyltransferase in patients with Crohn’s disease and severe myelosuppression during azathioprine therapy. Gastroenterology. 2000;118:1025–30. https://doi.org/10.1016/S0016-5085(00)70354-4
Ansari A, Arenas M, Greenfield SM, Morris D, Lindsay J, Gilshenan K, et al. Thiopurine methyltransferase activity and the use of azathioprine in inflammatory bowel disease. Aliment Pharmacol Ther. 2002;16:1743–50. https://doi.org/10.1046/j.1365-2036.2002.01353.x
Sumi S, Marinaki AM, Arenas M, Fairbanks L, Shobowale-Bakre EM, Rees DC, et al. Genetic basis of inosine triphosphate pyrophosphohydrolase deficiency. Hum Genet. 2002;111:360–7. https://doi.org/10.1007/s00439-002-0798-z
Marinaki AM, Duley JA, Arenas M, Sumi S, Lewis CM, Shobowale-Bakre M, et al. Adverse drug reactions to azathioprine therapy are associated with polymorphism in the gene encoding inosine triphosphate pyrophosphatase (ITPase). Pharmacogenetics. 2004;14:181–7. https://doi.org/10.1097/00008571-200403000-00006
Moriyama T, Nishii R, Perez-Andreu V, Yang W, Klussmann FA, Zhao X, et al. NUDT15 polymorphisms alter thiopurine metabolism and hematopoietic toxicity. Nat Genet. 2016;48:367–73. https://doi.org/10.1038/ng.3508
Yang JJ, Whirl-Carrillo M, Scott SA, Turner AJ, Schwab M, Tanaka Y, et al. Pharmacogene variation consortium gene introduction: NUDT15. Clin Pharmacol Ther. 2019;105:1091–4. https://doi.org/10.1002/cpt.1411
Maaser C, Sturm A, Vavricka SR, Kucharzik T, Fiorino G, Annese V, et al. ECCO-ESGAR guideline for diagnostic assessment in IBD Part 1: initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis. 2019;13:144–64. https://doi.org/10.1093/ecco-jcc/jjy113
Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005;19:5–36.
Harvey RF, Bradshaw JM. A simple index of Crohn’s disease activity. Lancet. 1980;1:514.
Campbell S, Kingstone K, Ghosh S. Relevance of thiopurine methyltransferase activity in inflammatory bowel disease patients maintained on low-dose azathioprine. Aliment Pharmacol Ther. 2002;16:389–98. https://doi.org/10.1046/j.1365-2036.2002.01177.x
Zelinkova Z, Derijks LJ, Stokkers PC, Vogels EW, van Kampen AH, Curvers WL, et al. Inosine triphosphate pyrophosphatase and thiopurine s-methyltransferase genotypes relationship to azathioprine-induced myelosuppression. Clin Gastroenterol Hepatol. 2006;4:44–49. https://doi.org/10.1016/j.cgh.2005.10.019
Dewit O, Moreels T, Baert F, Peeters H, Reenaers C, de Vos M, et al. Limitations of extensive TPMT genotyping in the management of azathioprine-induced myelosuppression in IBD patients. Clin Biochem. 2011;44:1062–6. https://doi.org/10.1016/j.clinbiochem.2011.06.079
Ansari A, Arenas M, Greenfield SM, Morris D, Lindsay J, Gilshenan K, et al. Prospective evaluation of the pharmacogenetics of azathioprine in the treatment of inflammatory bowel disease. Aliment Pharmacol Ther. 2008;28:973–83. https://doi.org/10.1111/j.1365-2036.2008.03788.x
Hindorf U, Lindqvist M, Peterson C, Söderkvist P, Ström M, Hjortswang H, et al. Pharmacogenetics during standardised initiation of thiopurine treatment in inflammatory bowel disease. Gut. 2006;55:1423–31. https://doi.org/10.1136/gut.2005.074930
Van Dieren JM, van Vuuren AJ, Kusters JG, Nieuwenhuis EE, Kuipers EJ, van der Woude CJ. ITPA genotyping is not predictive for the development of side effects in AZA treated inflammatory bowel disease patients. Gut. 2005;54:1664.
Gutiérrez-Valencia M, Leache L, Saiz LC, Beloqui JJ, Barajas M, Vicuña M, et al. Role of pharmacogenomics in the efficacy and safety of thiopurines in inflammatory bowel disease: a systematic review and meta-analysis. J Clin Gastroenterol. 2023;57:671–85.
Von Ahsen N, Armstrong VW, Behrens C, von Tirpitz C, Stallmach A, Herfarth H, et al. Association of inosine triphosphatase 94C>A and thiopurine S-methyltransferase deficiency with adverse events and study drop-outs under azathioprine therapy in a prospective Crohn disease study. Clin Chem. 2005;51:2282–8. https://doi.org/10.1373/clinchem.2005.057158
Mañosa M, Calafat M, de Francisco R, et al. Phenotype and natural history of elderly onset inflammatory bowel disease: a multicentre, case-control study. Aliment Pharmacol Ther. 2018;47:605–14. https://doi.org/10.1111/apt.14494
Author information
Authors and Affiliations
Contributions
JS and PR contributed to the design of the study, wrote the report, and analyzed data. JG, AA, MM, MS, and JL contributed to extracting and analyzing data and interpreting results. AG and EGP contributed to the design of the study, and analysis of data, and reviewed the final report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Salazar, J., Riera, P., Gordillo, J. et al. Predictive role of ITPA genetic variants in thiopurine-related myelotoxicity in Crohn’s disease patients. Pharmacogenomics J 24, 20 (2024). https://doi.org/10.1038/s41397-024-00341-2
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41397-024-00341-2