Abstract
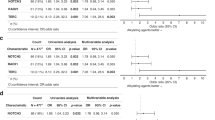
This study investigates combine effect of low BMI and possible pharmacogenetic influence of ABC gene polymorphisms in treatment responses of BC patients. BMI was analysed prior to commencement of chemotherapy. Clinical response was evaluated by radiological imaging and categorised as per RECISTv.1 criteria. SNPs (C1236T, C3435T, C58626A) in ABCB1 and ABCC2 gene were selected. 148 patients were analysed using PCR-RFLP. ABCC2 (58626AA) was significantly associated with treatment non-responsiveness in all genetic models namely dominant (OR 2.954; [1.442–6.051]; p = 0.003), recessive (OR 5.723; [2.48–13.20]; p < 0.0001), codominant (χ2 21.219; p < 0.0001). The proportion of ORR and NRs were significantly different between low (<18.5) and high (≥18.5) BMI classes (OR 16.097; [7.12–36.35]; p < 0.0001). Furthermore, when treatment response was combined with BMI groups, significant associations were observed for C58626A SNP across all genetic models among low BMI group: dominant (OR 3.324; [1.012–10.406]; p = 0.041), recessive (OR 7.250; [1.533–34.278]; p = 0.012) and codominant (χ2 8.657; p = 0.013). Both PFS (35.31 months; p = 0.005) and OS (39.75 months; p = 0.032) were lowered among AA genotype (ABCC2) while the hazard risk of this genotype was further increased in low BMI patients (HR 1.963). 3435CT genotypes in ABCB1 gene showed 87% reduction in risk of death (HR 0.13; p = 0.025). Low BMI independently and jointly with 58626AA genotype of ABCC2 gene was responsible for poor chemotherapy response and survival outcome among AC-T regimen receiving BC patients. Together, this study underscores the importance of genetic counselling and nutritional assessment for favourable treatment outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Ferlay J, Ervik M, Lam F, Laversanne M, Colombet M, Mery L et al. Global cancer observatory: cancer today. International agency for research cancer. World Health Organization. 2024. https://gco.iarc.who.int/today. Accessed 27 Apr 2024.
Gangane N, Anshu, Manvatkar S, Ng N, Hurtig AK, Sebastián MS. Prevalence and risk factors for patient delay among women with breast cancer in rural India. Asia Pac J Public Health. 2016;28:72–82.
Chintamani, Tuteja A, Khandelwal R, Megha T, Bamal R, Jain S, et al. Patient and provider delays in breast cancer patients attending a tertiary care centre: a prospective study. JRSM Short Rep. 2011;2:1–4.
Jassem J, Ozmen V, Bacanu F, Drobniene M, Eglitis J, Lakshmaiah KC, et al. Delays in diagnosis and treatment of breast cancer: a multinational analysis. Eur J Public Health. 2014;24:761–7.
Mistry T, Pal R, Ghosh S, Choudhury T, Mandal S, Nath P, et al. Impact of low BMI and nutritional status on quality of life and disease outcome in breast cancer patients: insights from a tertiary cancer center in India. Nutr Cancer. 2024;76:596–607.
Chen L, Wu F, Chen X, Chen Y, Deng L, Cai Q, et al. Impact of body mass index in therapeutic response for HER2 positive breast cancer treated with neoadjuvant targeted therapy: a multi-center study and meta-analysis. NPJ Breast Cancer. 2023;9:46.
Raman R, Mott SL, Schroeder MC, Phadke S, El Masri J, Thomas A. Effect of body mass index– and actual weight–based neoadjuvant chemotherapy doses on pathologic complete response in operable breast cancer. Clin Breast Cancer. 2016;16:480–6.
Singh P, Kapil U, Shukla NK, Deo SVS, Dwivedi SN. Association of overweight and obesity with breast cancer in India. Indian J Community Med. 2011;36:259–62.
Usiskin I, Li F, Irwin ML, Cartmel B, Sanft T. Association between pre-diagnosis BMI, physical activity, pathologic complete response, and chemotherapy completion in women treated with neoadjuvant chemotherapy for breast cancer. Breast Cancer. 2019;26:719–28.
Chang H, Rha SY, Jeung HC, Im CK, Ahn JB, Kwon WS, et al. Association of the ABCB1 gene polymorphisms 2677G>T/A and 3435C>T with clinical outcomes of paclitaxel monotherapy in metastatic breast cancer patients. Ann Oncol. 2009;20:272–7.
Chaturvedi P, Tulsyan S, Agarwal G, Lal P, Agarwal S, Mittal RD, et al. Influence of ABCB1 genetic variants in breast cancer treatment outcomes. Cancer Epidemiol. 2013;37:754–61.
Hlaváč V, Václavíková R, Brynychová V, Koževnikovová R, Kopečková K, Vrána D, et al. Role of genetic variation in ABC transporters in breast cancer prognosis and therapy response. Int J Mol Sci. 2020;21:1–17.
Abdul Aziz AA, Md Salleh MS, Mohamad I, Bhavaraju VMK, Yahya MM, Zakaria AD, et al. Genotypes and haplotypes of ABCB1 contribute to TAC chemotherapy response in Malaysian triple negative breast cancer patients. Meta Gene. 2018;16:21–27.
Lévy P, Gligorov J, Antoine M, Rezai K, Lévy E, Selle F, et al. Influence of ABCB1 polymorphisms and docetaxel pharmacokinetics on pathological response to neoadjuvant chemotherapy in breast cancer patients. Breast Cancer Res Treat. 2013;139:421–8.
Woo JS, Lee CH, Shim CK, Hwang SJ. Enhanced oral bioavailability of paclitaxel by coadministration of the p-glycoprotein inhibitor KR30031. Pharm Res. 2003;20:24–30.
Gutierrez-Rubio SA, Quintero-Ramos A, Durán-Cárdenas A, Franco-Topete RA, Franco-Topete RA, Castro-Cervantes JM, et al. 1236C/T and 3435C/T polymorphisms of the ABCB1 gene in Mexican breast cancer patients. Genet Mol Res. 2015;14:1250–9.
Mistry T, Nath P, Alam N, Nasare VD. Four year clinical outcomes: evaluating the efficacy of concomitant and sequential anthracycline-taxane chemotherapy in indian breast cancer patients – a regional cancer center study. J Curr Oncol Trends. 2024;1:110–9.
Mamounas EP, Bryant J, Lembersky B, Fehrenbacher L, Sedlacek SM, Fisher B, et al. Paclitaxel after doxorubicin plus cyclophosphamide as adjuvant chemotherapy for node-positive breast cancer: Results from NSABP B-28. J Clin Oncol. 2005;23:3686–96.
Cardoso F, Paluch-Shimon S, Senkus E, Curigliano G, Aapro MS, André F, et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann Oncol. 2020;31:1623–49.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Tamura M, Kondo M, Horio M, Ando M, Saito H, Yamamoto M, et al. Genetic polymorphisms of the adenosine triphosphate-binding cassette transporters (abcg2, abcb1) and gefitinib toxicity. Nagoya J Med Sci. 2012;74:133–40.
Tulsyan S, Chaturvedi P, Singh AK, Agarwal G, Lal P, Agrawal S, et al. Assessment of clinical outcomes in breast cancer patients treated with taxanes: multi-analytical approach. Gene. 2014;543:69–75.
Sathishkumar K, Chaturvedi M, Das P, Stephen S, Mathur P. Cancer incidence estimates for 2022 & projection for 2025: result from National Cancer Registry Programme, Indian J Med Res. 2022. https://doi.org/10.4103/ijmr.ijmr_1821_22.
Brewer HR, Jones ME, Schoemaker MJ, Ashworth A, Swerdlow AJ. Family history and risk of breast cancer: an analysis accounting for family structure. Breast Cancer Res Treat. 2017;165:193–200.
Choi JR, Kim JO, Kang DR, Shin JY, Zhang XH, Oh JE, et al. Genetic variations of drug transporters can influence on drug response in patients treated with docetaxel chemotherapy. Cancer Res Treat. 2015;47:509–17.
Leslie EM, Deeley RG, Cole SPC. Multidrug resistance proteins: role of P-glycoprotein, MRP1, MRP2, and BCRP (ABCG2) in tissue defense. Toxicol Appl Pharmacol. 2005;204:216–37.
Deeley RG, Westlake C, Cole SPC. Transmembrane transport of endo- and xenobiotics by mammalian ATP-binding cassette multidrug resistance proteins. Physiol Rev. 2006;86:849–99.
Zeliha KP, Dilek O, Ezgi O, Halil K, Cihan U, Gul O. Association between ABCB1, ABCG2 carrier protein and COX-2 enzyme gene polymorphisms and breast cancer risk in a Turkish population. Saudi Pharm J. 2020;28:215–9.
Acknowledgements
The authors would like to acknowledge the study participants and their respective guardians for their invaluable participation in this study. We also extend our gratitude to the Director of CNCI for providing the necessary infrastructure to facilitate this study and the funding agency (CSIR-HRDG, GOI; Grant no. 09/030(0085)/2019-EMR-I).
Funding
This study was funded by Council of Scientific and Industrial Research (CSIR)- Human Resource Development Group (HRDG), Government of India; Grant no. 09/030(0085)/2019-EMR-I awarded to Tanuma Mistry.
Author information
Authors and Affiliations
Contributions
Study concepts by TM, VDN; Study Design by TM, SSG, VDN; Data acquisition by TM, PN, NA; Quality control of data and algorithms by TM, PN, NA, VDN; Data analysis and interpretation by TM, SSG, RSK, NT, VDN; Statistical analysis TM, SSG, VDN, Manuscript preparation TM, SSG, VDN; Manuscript editing TM, SSG, RSK, NT, VDN; Manuscript reviewed by All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study protocol was reviewed and approved by Institutional Ethical Committee and was conducted according to Good Clinical Practice under the Declaration of Helsinki [Reference id: CNCI-IEC-DL-2020-6].
Consent to participate
All patients have provided written informed consent in their preferred language (Bengali/Hindi/English) before taking part in this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mistry, T., Sengupta, S., Kumar, R.S. et al. Impact of low BMI and ABCC2 genotype on the clinical response of sequential anthracycline-taxane chemotherapy receiving breast cancer patients: a hospital-based study. Pharmacogenomics J 25, 22 (2025). https://doi.org/10.1038/s41397-025-00380-3
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41397-025-00380-3