Abstract
Background
Fecal microbiota transplantation (FMT) has emerged as a key tool to explore the role of the microbiome-gut-brain axis in psychiatric disorders. However, the field is hindered by significant methodological inconsistencies.
Methods
A comprehensive literature search identified 31 studies performing FMT from human patients with psychiatric conditions into rodent models.
Results
None of the 31 studies followed an identical FMT protocol. Significant heterogeneity was observed across studies in rodent model selection, including germ-free, antibiotic-pretreated, or specific pathogen-free approaches, in antibiotic regimens, timing and microbiota depletion verification, as well as in FMT donor strategy, dosage, frequency, engraftment assessment, and behavioral testing schedules.
Conclusions
This review highlights the necessity for standardized methodologies in microbiome research. Evidence-based recommendations are provided to promote reproducibility in future work. Investigators are encouraged to publish transparent and rigorous protocols, to enhance the translational potential of microbiome-gut-brain axis research.
Similar content being viewed by others
Data availability
All data are available in the main text or the supplementary materials.
References
Grau-Del Valle C, Fernández J, Solá E, Montoya-Castilla I, Morillas C, Bañuls C. Association between gut microbiota and psychiatric disorders: a systematic review. Front Psychol. 2023;14:1215674.
Chen LL, Abbaspour A, Mkoma GF, Bulik CM, Rück C, Djurfeldt D. Gut microbiota in psychiatric disorders: A systematic review. Psychosom Med. 2021;83:679–92.
Nguyen TT, Kosciolek T, Eyler LT, Knight R, Jeste DV. Overview and systematic review of studies of microbiome in schizophrenia and bipolar disorder. J Psychiatr Res. 2018;99:50–61.
Bokoliya SC, Dorsett Y, Panier H, Zhou Y. Procedures for fecal microbiota transplantation in murine microbiome studies. Front Cell Infect Microbiol. 2021;11:711055.
Kelly JR, Borre Y, O’ Brien C, Patterson E, El Aidy S, Deane J, et al. Transferring the blues: Depression-associated gut microbiota induces neurobehavioural changes in the rat. J Psychiatr Res. 2016;82:109–18.
Gheorghe CE, Ritz NL, Martin JA, Wardill HR, Cryan JF, Clarke G. Investigating causality with fecal microbiota transplantation in rodents: applications, recommendations and pitfalls. Gut Microbes. 2021;13:1941711.
Jones J, Reinke SN, Ali A, Palmer DJ, Christophersen CT. Fecal sample collection methods and time of day impact microbiome composition and short chain fatty acid concentrations. Sci Rep. 2021;11:13964.
Nicco C, Paule A, Konturek P, Edeas M. From donor to patient: collection, preparation and cryopreservation of fecal samples for fecal microbiota transplantation. Diseases. 2020;8:9.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Liu P, Liu Z, Wang J, Wang J, Gao M, Zhang Y, et al. Immunoregulatory role of the gut microbiota in inflammatory depression. Nat Commun. 2024;15:3003.
Medina-Rodriguez EM, Watson J, Reyes J, Trivedi M, Beurel E. Th17 cells sense microbiome to promote depressive-like behaviors. Microbiome. 2023;11:92.
Yoo J-W, Shin Y-J, Ma X, Son Y-H, Jang H-M, Lee CK, et al. The alleviation of gut microbiota-induced depression and colitis in mice by anti-inflammatory probiotics NK151, NK173, and NK175. Nutrients. 2022;14:2080.
Zhang Y, Fan Q, Hou Y, Zhang X, Yin Z, Cai X, et al. Bacteroides species differentially modulate depression-like behavior via gut-brain metabolic signaling. Brain Behav Immun. 2022;102:11–22.
Liu Y, Wang H, Gui S, Zeng B, Pu J, Zheng P, et al. Proteomics analysis of the gut-brain axis in a gut microbiota-dysbiosis model of depression. Transl Psychiatry. 2021;11:568.
Li B, Guo K, Zeng L, Zeng B, Huo R, Luo Y, et al. Metabolite identification in fecal microbiota transplantation mouse livers and combined proteomics with chronic unpredictive mild stress mouse livers. Transl Psychiatry. 2018;8:34.
Knudsen JK, Michaelsen TY, Bundgaard-Nielsen C, Nielsen RE, Hjerrild S, Leutscher P, et al. Faecal microbiota transplantation from patients with depression or healthy individuals into rats modulates mood-related behaviour. Sci Rep. 2021;11:21869.
Zheng P, Zeng B, Zhou C, Liu M, Fang Z, Xu X, et al. Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host’s metabolism. Mol Psychiatry. 2016;21:786–96.
Jang H-M, Kim J-K, Joo M-K, Shin Y-J, Lee CK, Kim H-J, et al. Transplantation of fecal microbiota from patients with inflammatory bowel disease and depression alters immune response and behavior in recipient mice. Sci Rep. 2021;11:20406.
Liu L, Wang H, Rao X, Yu Y, Li W, Zheng P, et al. Comprehensive analysis of the lysine acetylome and succinylome in the hippocampus of gut microbiota-dysbiosis mice. J Adv Res. 2021;30:27–38.
Liu S, Guo R, Liu F, Yuan Q, Yu Y, Ren F. Gut microbiota regulates depression-like behavior in rats through the neuroendocrine-immune-mitochondrial pathway. Neuropsychiatr Dis Treat. 2020;16:859–69.
Chen S, Li M, Tong C, Wang Y, He J, Shao Q, et al. Regulation of miRNA expression in the prefrontal cortex by fecal microbiota transplantation in anxiety-like mice. Front Psychiatry. 2024;15:1323801.
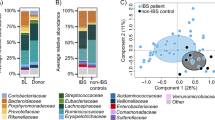
Ritz NL, Brocka M, Butler MI, Cowan CSM, Barrera-Bugueño C, Turkington CJR, et al. Social anxiety disorder-associated gut microbiota increases social fear. Proc Natl Acad Sci USA. 2024;121:e2308706120.
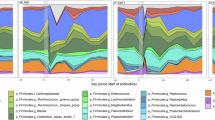
De Palma G, Lynch MDJ, Lu J, Dang VT, Deng Y, Jury J, et al. Transplantation of fecal microbiota from patients with irritable bowel syndrome alters gut function and behavior in recipient mice. Sci Transl Med. 2017;9:eaaf6397.
Fan Y, Støving RK, Berreira Ibraim S, Hyötyläinen T, Thirion F, Arora T, et al. The gut microbiota contributes to the pathogenesis of anorexia nervosa in humans and mice. Nat Microbiol. 2023;8:787–802.
Glenny EM, Fouladi F, Thomas SA, Bulik-Sullivan EC, Tang Q, Djukic Z, et al. Gut microbial communities from patients with anorexia nervosa do not influence body weight in recipient germ-free mice. Gut Microbes. 2021;13:1–15.
Hata T, Miyata N, Takakura S, Yoshihara K, Asano Y, Kimura-Todani T, et al. The gut microbiome derived from anorexia nervosa patients impairs weight gain and behavioral performance in female mice. Endocrinology. 2019;160:2441–52.
Wang C, Yan J, Du K, Liu S, Wang J, Wang Q, et al. Intestinal microbiome dysbiosis in alcohol-dependent patients and its effect on rat behaviors. mBio. 2023;14:e0239223.
Wolstenholme JT, Saunders JM, Smith M, Kang JD, Hylemon PB, González-Maeso J, et al. Reduced alcohol preference and intake after fecal transplant in patients with alcohol use disorder is transmissible to germ-free mice. Nat Commun. 2022;13:6198.
Leclercq S, Le Roy T, Furgiuele S, Coste V, Bindels LB, Leyrolle Q, et al. Gut microbiota-induced changes in β-Hydroxybutyrate metabolism are linked to altered sociability and depression in alcohol use disorder. Cell Rep. 2020;33:108238.
Zhao W, Hu Y, Li C, Li N, Zhu S, Tan X, et al. Transplantation of fecal microbiota from patients with alcoholism induces anxiety/depression behaviors and decreases brain mGluR1/PKC ε levels in mouse. BioFactors Oxf Engl. 2020;46:38–54.
Avolio E, Olivito I, Rosina E, Romano L, Angelone T, De Bartolo A, et al. Modifications of behavior and inflammation in mice following transplant with fecal microbiota from children with autism. Neuroscience. 2022;498:174–89.
Xiao L, Yan J, Yang T, Zhu J, Li T, Wei H, et al. Fecal microbiome transplantation from children with autism spectrum disorder modulates tryptophan and serotonergic synapse metabolism and induces altered behaviors in germ-free mice. mSystems. 2021;6:e01343–20.
Sharon G, Cruz NJ, Kang D-W, Gandal MJ, Wang B, Kim Y-M, et al. Human gut microbiota from autism spectrum disorder promote behavioral symptoms in mice. Cell. 2019;177:1600–1618.e17.
Tengeler AC, Dam SA, Wiesmann M, Naaijen J, van Bodegom M, Belzer C, et al. Gut microbiota from persons with attention-deficit/hyperactivity disorder affects the brain in mice. Microbiome. 2020;8:44.
Lai J, Zhang P, Jiang J, Mou T, Li Y, Xi C, et al. New evidence of gut microbiota involvement in the neuropathogenesis of bipolar depression by TRANK1 modulation: Joint clinical and animal data. Front Immunol. 2021;12:789647.
Yu H, Yang W-M, Chen Y-H, Guo L, Li R, Xue F, et al. The gut microbiome from middle-aged women with depression modulates depressive-like behaviors and plasma fatty acid metabolism in female middle-aged mice. J Psychiatr Res. 2024;173:139–50.
Wei N, Ju M, Su X, Zhang Y, Huang Y, Rao X, et al. Transplantation of gut microbiota derived from patients with schizophrenia induces schizophrenia-like behaviors and dysregulated brain transcript response in mice. Schizophr Heidelb Ger. 2024;10:44.
Zhu F, Guo R, Wang W, Ju Y, Wang Q, Ma Q, et al. Transplantation of microbiota from drug-free patients with schizophrenia causes schizophrenia-like abnormal behaviors and dysregulated kynurenine metabolism in mice. Mol Psychiatry. 2020;25:2905–18.
Zheng P, Zeng B, Liu M, Chen J, Pan J, Han Y, et al. The gut microbiome from patients with schizophrenia modulates the glutamate-glutamine-GABA cycle and schizophrenia-relevant behaviors in mice. Sci Adv. 2019;5:eaau8317.
Moreau CA, Raznahan A, Bellec P, Chakravarty M, Thompson PM, Jacquemont S. Dissecting autism and schizophrenia through neuroimaging genomics. Brain. 2021;144:1943–57.
Craddock N, Mynors-Wallis L. Psychiatric diagnosis: impersonal, imperfect and important. Br J Psychiatry. 2014;204:93–95.
Goldberg D. A dimensional model for common mental disorders. Br J Psychiatry. 1996;168:44–49.
Sun M, Chen H, Dong S, Zhang G, Zhou X, Cheng H. Alteration of gut microbiota in post-stroke depression patients with Helicobacter pylori infection. Neurobiol Dis. 2024;193:106458.
Hu X, Li Y, Wu J, Zhang H, Huang Y, Tan X, et al. Changes of gut microbiota reflect the severity of major depressive disorder: a cross sectional study. Transl Psychiatry. 2023;13:137.
Scaldaferri F, D’Onofrio AM, Calia R, Di Vincenzo F, Ferrajoli GF, Petito V, et al. Gut microbiota signatures are associated with psychopathological profiles in patients with ulcerative colitis: Results from an italian tertiary IBD center. Inflamm Bowel Dis. 2023;29:1805–18.
Çakici N, Sutterland AL, Penninx BWJH, Dalm VA, de Haan L, van Beveren NJM. Altered peripheral blood compounds in drug-naïve first-episode patients with either schizophrenia or major depressive disorder: a meta-analysis. Brain Behav Immun. 2020;88:547–58.
Çakici N, Sutterland AL, Penninx BWJH, de Haan L, van Beveren NJM. Changes in peripheral blood compounds following psychopharmacological treatment in drug-naïve first-episode patients with either schizophrenia or major depressive disorder: a meta-analysis. Psychol Med. 2021;51:538–49.
Singh R, Bansal Y, Medhi B, Kuhad A. Antipsychotics-induced metabolic alterations: Recounting the mechanistic insights, therapeutic targets and pharmacological alternatives. Eur J Pharmacol. 2019;844:231–40.
Javdan B, Lopez JG, Chankhamjon P, Lee Y-CJ, Hull R, Wu Q, et al. Personalized mapping of drug metabolism by the human gut microbiome. Cell. 2020;181:1661–1679.e22.
Schulte S, Sukhova GK, Libby P. Genetically programmed biases in Th1 and Th2 immune responses modulate atherogenesis. Am J Pathol. 2008;172:1500–8.
Watanabe H, Numata K, Ito T, Takagi K, Matsukawa A. INNATE IMMUNE RESPONSE IN TH1- AND TH2-DOMINANT MOUSE STRAINS. Shock. 2004;22:460–6.
Sultana R, Ogundele OM, Lee CC. Contrasting characteristic behaviours among common laboratory mouse strains. R Soc Open Sci. 2019;6:190574.
Bothe GWM, Bolivar VJ, Vedder MJ, Geistfeld JG. Behavioral differences among fourteen inbred mouse strains commonly used as disease models. Comp Med. 2005;55:326–34.
Wahlsten D, Bachmanov A, Finn DA, Crabbe JC. Stability of inbred mouse strain differences in behavior and brain size between laboratories and across decades. Proc Natl Acad Sci. 2006;103:16364–9.
Moy S, Nadler J, Young N, Perez A, Holloway L, Barbaro R, et al. Mouse behavioral tasks relevant to autism: Phenotypes of 10 inbred strains. Behav Brain Res. 2007;176:4–20.
Sankoorikal GMV, Kaercher KA, Boon CJ, Lee JK, Brodkin ES. A mouse model system for genetic analysis of sociability: C57BL/6J versus BALB/cJ inbred mouse strains. Biol Psychiatry. 2006;59:415–23.
An X-L, Zou J-X, Wu R-Y, Yang Y, Tai F-D, Zeng S-Y, et al. Strain and sex differences in anxiety-like and social behaviors in C57BL/6J and BALB/cJ mice. Exp Anim. 2011;60:111–23.
Kurilshikov A, Medina-Gomez C, Bacigalupe R, Radjabzadeh D, Wang J, Demirkan A, et al. Large-scale association analyses identify host factors influencing human gut microbiome composition. Nat Genet. 2021;53:156–65.
Basson AR, Gomez-Nguyen A, Menghini P, Buttó LF, Di Martino L, Aladyshkina N, et al. Human gut microbiome transplantation in ileitis prone mice: A tool for the functional characterization of the microbiota in inflammatory bowel disease patients. Inflamm Bowel Dis. 2019:izz242.
Gururajan A, Reif A, Cryan JF, Slattery DA. The future of rodent models in depression research. Nat Rev Neurosci. 2019;20:686–701.
Monteggia LM, Heimer H, Nestler EJ. Meeting report: Can we make animal models of human mental illness?. Biol Psychiatry. 2018;84:542–5.
Higashiyama H, Uemura M, Igarashi H, Kurohmaru M, Kanai-Azuma M, Kanai Y. Anatomy and development of the extrahepatic biliary system in mouse and rat: a perspective on the evolutionary loss of the gallbladder. J Anat. 2018;232:134–45.
Lleal M, Sarrabayrouse G, Willamil J, Santiago A, Pozuelo M, Manichanh C. A single faecal microbiota transplantation modulates the microbiome and improves clinical manifestations in a rat model of colitis. EBioMedicine. 2019;48:630–41.
Wos-Oxley ML, Bleich A, Oxley APA, Kahl S, Janus LM, Smoczek A, et al. Comparative evaluation of establishing a human gut microbial community within rodent models. Gut Microbes. 2012;3:234–49.
Bugos O, Bhide M, Zilka N. Beyond the rat models of human neurodegenerative disorders. Cell Mol Neurobiol. 2009;29:859–69.
Rodent models in neuroscience research: is it a rat race? | Disease Models & Mechanisms | The Company of Biologists. https://journals.biologists.com/dmm/article/9/10/1079/3833/Rodent-models-in-neuroscience-research-is-it-a-rat. Accessed 17 August 2025.
Wildner G. Are rats more human than mice?. Immunobiology. 2019;224:172–6.
Williams SCP. Gnotobiotics. Proc Natl Acad Sci. 2014;111:1661–1661.
Curotto De Lafaille MA, Lafaille JJ. Natural and adaptive Foxp3+ regulatory T cells: More of the same or a division of labor?. Immunity. 2009;30:626–35.
Round JL, Mazmanian SK. The gut microbiota shapes intestinal immune responses during health and disease. Nat Rev Immunol. 2009;9:313–23.
Heijtz RD, Wang S, Anuar F, Qian Y, Björkholm B, Samuelsson A, et al. Normal gut microbiota modulates brain development and behavior. Proc Natl Acad Sci. 2011;108:3047–52.
De Palma G, Blennerhassett P, Lu J, Deng Y, Park AJ, Green W, et al. Microbiota and host determinants of behavioural phenotype in maternally separated mice. Nat Commun. 2015;6:7735.
Bongers KS, McDonald RA, Winner KM, Falkowski NR, Brown CA, Baker JM, et al. Antibiotics cause metabolic changes in mice primarily through microbiome modulation rather than behavioral changes. PLOS ONE. 2022;17:e0265023.
López-Sánchez A, Pérez-Cantero A, Torrado-Salmerón C, Martin-Vicente A, García-Herrero V, González-Nicolás MÁ, et al. Efficacy, biodistribution, and nephrotoxicity of experimental amphotericin B-deoxycholate formulations for pulmonary aspergillosis. Antimicrob Agents Chemother. 2018;62:e00489-18.
Lundberg R, Toft MF, August B, Hansen AK, Hansen CHF. Antibiotic-treated versus germ-free rodents for microbiota transplantation studies. Gut Microbes. 2016;7:68–74.
Le Roy T, Debédat J, Marquet F, Da-Cunha C, Ichou F, Guerre-Millo M, et al. Comparative evaluation of microbiota engraftment following fecal microbiota transfer in mice models: Age, kinetic and microbial status matter. Front Microbiol. 2019;9:3289.
Kim Y-G, Sakamoto K, Seo S-U, Pickard JM, Gillilland MG, Pudlo NA, et al. Neonatal acquisition of Clostridia species protects against colonization by bacterial pathogens. Science. 2017;356:315–9.
Rodriguez-Palacios A, Aladyshkina N, Ezeji JC, Erkkila HL, Conger M, Ward J, et al. ‘Cyclical Bias’ in microbiome research revealed by a portable germ-free housing system using nested isolation. Sci Rep. 2018;8:3801.
Porcari S, Benech N, Valles-Colomer M, Segata N, Gasbarrini A, Cammarota G, et al. Key determinants of success in fecal microbiota transplantation: From microbiome to clinic. Cell Host Microbe. 2023;31:712–33.
Andary CM, Al KF, Chmiel JA, Gibbons S, Daisley BA, Parvathy SN, et al. Dissecting mechanisms of fecal microbiota transplantation efficacy in disease. Trends Mol Med. 2024;30:209–22.
Dollive S, Chen Y-Y, Grunberg S, Bittinger K, Hoffmann C, Vandivier L, et al. Fungi of the murine gut: Episodic variation and proliferation during antibiotic treatment. PloS One. 2013;8:e71806.
Botschuijver S, Roeselers G, Levin E, Jonkers DM, Welting O, Heinsbroek SEM, et al. Intestinal fungal dysbiosis is associated with visceral hypersensitivity in patients with irritable bowel syndrome and rats. Gastroenterology. 2017;153:1026–39.
Chin VK, Yong VC, Chong PP, Amin Nordin S, Basir R, Abdullah M. Mycobiome in the gut: A multiperspective review. Mediators Inflamm. 2020;2020:9560684.
Karimzadeh I, Sepehr-Sobhani A, Khoshnoud MJ, Sagheb MM, Vejdani R, Jalali A, et al. Comparison of intravenous sodium bicarbonate and sodium chloride combination versus intravenous sodium chloride hydration alone in reducing amphotericin B nephrotoxicity: a randomized clinical trial. Res Pharm Sci. 2020;15:583–91.
Tonomura Y, Yamamoto E, Kondo C, Itoh A, Tsuchiya N, Uehara T, et al. Amphotericin B-induced nephrotoxicity: characterization of blood and urinary biochemistry and renal morphology in mice. Hum Exp Toxicol. 2009;28:293–300.
Thanki K, Date T, Jain S. Improved oral bioavailability and gastrointestinal stability of amphotericin B through fatty acid conjugation approach. Mol Pharm. 2019;16:4519–29.
Alam A, Levanduski E, Denz P, Villavicencio HS, Bhatta M, Alhorebi L, et al. Fungal mycobiome drives IL-33 secretion and type 2 immunity in pancreatic cancer. Cancer Cell. 2022;40:153–.e11.
Alam A, Comer S, Levanduski E, Dey P. Fungal ablation and transplantation of specific fungal species into PDAC tumor-bearing mice. STAR Protoc. 2022;3:101644.
Reikvam DH, Erofeev A, Sandvik A, Grcic V, Jahnsen FL, Gaustad P, et al. Depletion of murine intestinal microbiota: effects on gut mucosa and epithelial gene expression. PLOS ONE. 2011;6:e17996.
Tirelle P, Breton J, Riou G, Déchelotte P, Coëffier M, Ribet D. Comparison of different modes of antibiotic delivery on gut microbiota depletion efficiency and body composition in mouse. BMC Microbiol. 2020;20:340.
Ritz NL, Draper LA, Bastiaanssen TFS, Turkington CJR, Peterson VL, van de Wouw M, et al. The gut virome is associated with stress-induced changes in behaviour and immune responses in mice. Nat Microbiol. 2024;9:359–76.
Ochoa-Repáraz J, Mielcarz DW, Ditrio LE, Burroughs AR, Foureau DM, Haque-Begum S, et al. Role of gut commensal microflora in the development of experimental autoimmune encephalomyelitis. J Immunol Baltim Md 1950. 2009;183:6041–50.
Hill DA, Hoffmann C, Abt MC, Du Y, Kobuley D, Kirn TJ, et al. Metagenomic analyses reveal antibiotic-induced temporal and spatial changes in intestinal microbiota with associated alterations in immune cell homeostasis. Mucosal Immunol. 2010;3:148–58.
Zarrinpar A, Chaix A, Xu ZZ, Chang MW, Marotz CA, Saghatelian A, et al. Antibiotic-induced microbiome depletion alters metabolic homeostasis by affecting gut signaling and colonic metabolism. Nat Commun. 2018;9:2872.
Arantes-Rodrigues R, Henriques A, Pinto-Leite R, Faustino-Rocha A, Pinho-Oliveira J, Teixeira-Guedes C, et al. The effects of repeated oral gavage on the health of male CD-1 mice. Lab Anim. 2012;41:129–34.
Germann PG, Ockert D. Granulomatous inflammation of the oropharyngeal cavity as a possible cause for unexpected high mortality in a Fischer 344 rat carcinogenicity study. Lab Anim Sci. 1994;44:338–43.
Murphy SJ, Smith P, Shaivitz AB, Rossberg MI, Hurn PD. The effect of brief halothane anesthesia during daily gavage on complications and body weight in rats. Contemp Top Lab Anim Sci. 2001;40:9–12.
Amorim N, McGovern E, Raposo A, Khatiwada S, Shen S, Koentgen S, et al. Refining a protocol for faecal microbiota engraftment in animal models after successful antibiotic-induced gut decontamination. Front Med. 2022;9:770017.
Reygner J, Delannoy J, Barba-Goudiaby M-T, Gasc C, Levast B, Gaschet E, et al. Reduction of product composition variability using pooled microbiome ecosystem therapy and consequence in two infectious murine models. Appl Environ Microbiol. 2024;90:e00016-24.
Levast B, Fontaine M, Nancey S, Dechelotte P, Doré J, Lehert P. Single-Donor and pooling strategies for fecal microbiota transfer product preparation in ulcerative colitis: A systematic review and meta-analysis. Clin Transl Gastroenterol. 2023;14:e00568.
Kazerouni A, Wein LM. Exploring the efficacy of pooled stools in fecal microbiota transplantation for microbiota-associated chronic diseases. PLOS ONE. 2017;12:e0163956.
Walter J, Armet AM, Finlay BB, Shanahan F. Establishing or exaggerating causality for the gut microbiome: lessons from human microbiota-associated rodents. Cell. 2020;180:221–32.
Lazic SE, Clarke-Williams CJ, Munafò MR. What exactly is ‘N’ in cell culture and animal experiments?. PLOS Biol. 2018;16:e2005282.
Wrzosek L, Ciocan D, Borentain P, Spatz M, Puchois V, Hugot C, et al. Transplantation of human microbiota into conventional mice durably reshapes the gut microbiota. Sci Rep. 2018;8:6854.
Choo JM, Rogers GB. Establishment of murine gut microbiota in gnotobiotic mice. iScience. 2021;24:102049.
El Aidy S, Van Baarlen P, Derrien M, Lindenbergh-Kortleve DJ, Hooiveld G, Levenez F, et al. Temporal and spatial interplay of microbiota and intestinal mucosa drive establishment of immune homeostasis in conventionalized mice. Mucosal Immunol. 2012;5:567–79.
Herman C, Barker BM, Bartelli TF, Chandra V, Krajmalnik-Brown R, Jewell M, et al. A review of engraftment assessments following fecal microbiota transplant. Gut Microbes. 2025;17:2525478.
Yadegar A, Bar-Yoseph H, Monaghan TM, Pakpour S, Severino A, Kuijper EJ, et al. Fecal microbiota transplantation: current challenges and future landscapes. Clin Microbiol Rev. 2024;37:e0006022.
Shi Y, Zhang L, Peterson CB, Do K-A, Jenq RR. Performance determinants of unsupervised clustering methods for microbiome data. Microbiome. 2022;10:25.
Hintze KJ, Cox JE, Rompato G, Benninghoff AD, Ward RE, Broadbent J, et al. Broad scope method for creating humanized animal models for animal health and disease research through antibiotic treatment and human fecal transfer. Gut Microbes. 2014;5:183–91.
Brown AP, Dinger N, Levine BS. Stress produced by gavage administration in the rat. Contemp Top Lab Anim Sci. 2000;39:17–21.
Balcombe JP, Barnard ND, Sandusky C. Laboratory routines cause animal stress. Contemp Top Lab Anim Sci. 2004;43:42–51.
Bonnichsen M, Dragsted N, Hansen A. The welfare impact of gavaging laboratory rats. Anim Welf. 2005;14:223–7.
Walker MK, Boberg JR, Walsh MT, Wolf V, Trujillo A, Duke MS, et al. A less stressful alternative to oral gavage for pharmacological and toxicological studies in mice. Toxicol Appl Pharmacol. 2012;260:65–69.
Jones CP, Boyd KL, Wallace JM. Evaluation of mice undergoing serial oral gavage while awake or anesthetized. J Am Assoc Lab Anim Sci JAALAS. 2016;55:805–10.
Funding
A.G.N. and F.C. were supported by the National Institute of Diabetes and Digestive and Kidney Diseases, NIDDK097948. A.B. was supported by R01AG085316, 5R03AG080175-02, and Target ALS New Academic Investigators Award.
Author information
Authors and Affiliations
Contributions
A.M.D. and A.G.N. conceptualized the study, performed the literature search, wrote the main manuscript text, and prepared figures. A.B., G.C., F.S., and F.C. provided expertise contributing to the final recommendations and edited the manuscript. All authors read and reviewed the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
“All models are wrong, some are useful.”
George E. P. Box, 1976
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
D’Onofrio, A.M., Gomez-Nguyen, A., Camardese, G. et al. Fecal microbiota transplantation from psychiatric patients to mice - systematic review of methodologies and a call for standardization. Transl Psychiatry (2026). https://doi.org/10.1038/s41398-026-03847-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-026-03847-4