Abstract
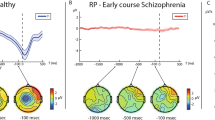
Synaptic dysfunction is a candidate mechanism in psychotic disorders, yet the precise underlying substrates remain elusive. We investigated how combining in vivo electroencephalography (EEG) and in vitro human cortical spheroid (hCS)-based methods can further our understanding of psychosis pathophysiology during fetal stages of neurodevelopment. Ten individuals with schizophrenia (SZ) or bipolar disorder (BD; 5 males and 5 females) and five controls (CTRL; 3 males and 2 females) underwent EEG assessments, including long-term potentiation (LTP)-like cortical plasticity and mismatch negativity (MMN). hCS were generated from induced pluripotent stem cells of all participants, and immunohistochemistry, Seahorse bioenergetics and patch-clamp recordings were performed. EEG-based LTP-like plasticity was reduced in individuals with SZ and BD. Basal respiration was decreased in BD hCS and VGLUT1 levels were reduced in both SZ and BD hCS. There was a positive association between EEG-based LTP-like plasticity and hCS basal respiration which survived correction. Our data provide further support for roles of mitochondrial and glutamatergic impairments in the synaptic dysfunction of psychosis and demonstrate the potential of combining EEG- and hCS-based methods for early development mechanistic studies of brain disorders.
Similar content being viewed by others
Data availability
De-identified data supporting the findings of this study are available from the corresponding author upon reasonable request. Access is subjected to approval by the relevant ethics committee and data protection regulations.
References
Freedman R. Schizophrenia. N Engl J Med. 2003;349:1738–49.
Belmaker RH. Bipolar disorder. N Engl J Med. 2004;351:476–86.
Lopez AD, Murray CC. The global burden of disease, 1990-2020. Nat Med. 1998;4:1241–3.
PGC. Genomic dissection of bipolar disorder and schizophrenia, including 28 subphenotypes. Cell. 2018;173:1705–15.e1716.
Trubetskoy V, Pardiñas AF, Qi T, Panagiotaropoulou G, Awasthi S, Bigdeli TB, et al. Mapping genomic loci implicates genes and synaptic biology in schizophrenia. Nature. 2022;604:502–8.
Mullins N, Forstner AJ, O’Connell KS, Coombes B, Coleman JRI, Qiao Z, et al. Genome-wide association study of more than 40,000 bipolar disorder cases provides new insights into the underlying biology. Nat Genet. 2021.
Luck SJ An Introduction to the Event-Related Potential Technique. The MIT Press: Cambridge, MA, 2005.
Cavus I, Reinhart RM, Roach BJ, Gueorguieva R, Teyler TJ, Clapp WC, et al. Impaired visual cortical plasticity in schizophrenia. Biol Psychiatry. 2012;71:512–20.
Cooke SF, Bear MF. Stimulus-selective response plasticity in the visual cortex: an assay for the assessment of pathophysiology and treatment of cognitive impairment associated with psychiatric disorders. Biol Psychiatry. 2012;71:487–95.
Normann C, Schmitz D, Furmaier A, Doing C, Bach M. Long-term plasticity of visually evoked potentials in humans is altered in major depression. Biol Psychiatry. 2007;62:373–80.
Elvsåshagen T, Moberget T, Boen E, Boye B, Englin NO, Pedersen PO, et al. Evidence for impaired neocortical synaptic plasticity in bipolar II disorder. Biol Psychiatry. 2012;71:68–74.
Valstad M, Roelfs D, Slapo NB, Timpe CMF, Rai A, Matziorinis AM, et al. Evidence for reduced long-term potentiation-like visual cortical plasticity in schizophrenia and bipolar disorder. Schizophr Bull. 2021;47:1751–60.
Naatanen R, Alho K. Mismatch negativity-a unique measure of sensory processing in audition. Int J Neurosci. 1995;80:317–37.
Thiebes S, Leicht G, Curic S, Steinmann S, Polomac N, Andreou C, et al. Glutamatergic deficit and schizophrenia-like negative symptoms: new evidence from ketamine-induced mismatch negativity alterations in healthy male humans. J Psychiatry Neurosci. 2017;42:273–83.
Javitt DC, Steinschneider M, Schroeder CE, Arezzo JC. Role of cortical N-methyl-D-aspartate receptors in auditory sensory memory and mismatch negativity generation: implications for schizophrenia. Proc Natl Acad Sci USA. 1996;93:11962–7.
de Sousa RT, Machado-Vieira R, Zarate CA Jr, Manji HK. Targeting mitochondrially mediated plasticity to develop improved therapeutics for bipolar disorder. Expert Opin Ther Targets. 2014;18:1131–47.
Hermens DF, Chitty KM, Kaur M. Mismatch negativity in bipolar disorder: A neurophysiological biomarker of intermediate effect?. Schizophr Res. 2018;191:132–9.
Erickson MA, Ruffle A, Gold JM. A meta-analysis of mismatch negativity in schizophrenia: from clinical risk to disease specificity and progression. Biol Psychiatry. 2016;79:980–7.
Light GA, Swerdlow NR, Thomas ML, Calkins ME, Green MF, Greenwood TA, et al. Validation of mismatch negativity and P3a for use in multi-site studies of schizophrenia: characterization of demographic, clinical, cognitive, and functional correlates in COGS-2. Schizophr Res. 2015;163:63–72.
Rangaraju V, Calloway N, Ryan TA. Activity-driven local ATP synthesis is required for synaptic function. Cell. 2014;156:825–35.
Logothetis NK, Pauls J, Augath M, Trinath T, Oeltermann A. Neurophysiological investigation of the basis of the fMRI signal. Nature. 2001;412:150–7.
Magistretti PJ, Allaman I. A cellular perspective on brain energy metabolism and functional imaging. Neuron. 2015;86:883–901.
Pellerin L, Magistretti PJ. Sweet sixteen for ANLS. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2012;32:1152–66.
Du F, Cooper AJ, Thida T, Sehovic S, Lukas SE, Cohen BM, et al. In vivo evidence for cerebral bioenergetic abnormalities in schizophrenia measured using 31P magnetization transfer spectroscopy. JAMA Psychiatry. 2014;71:19–27.
Du F, Yuksel C, Chouinard VA, Huynh P, Ryan K, Cohen BM, et al. Abnormalities in high-energy phosphate metabolism in first-episode bipolar disorder measured using (31)P-magnetic resonance spectroscopy. Biol Psychiatry. 2018;84:797–802.
Sarnyai Z, Ben-Shachar D. Schizophrenia, a disease of impaired dynamic metabolic flexibility: A new mechanistic framework. Psychiatry Res. 2024;342:116220.
McCullumsmith RE, Clinton SM, Meador-Woodruff JH. Schizophrenia as a disorder of neuroplasticity. Int Rev Neurobiol. 2004;59:19–45. pp.
Hjelm BE, Rollins B, Mamdani F, Lauterborn JC, Kirov G, Lynch G, et al. Evidence of mitochondrial dysfunction within the complex genetic etiology of schizophrenia. Mol Neuropsychiatry. 2015;1:201–19.
Breen MS, Dobbyn A, Li Q, Roussos P, Hoffman GE, Stahl E, et al. Global landscape and genetic regulation of RNA editing in cortical samples from individuals with schizophrenia. Nat Neurosci. 2019;22:1402–12.
Manji H, Kato T, Di Prospero NA, Ness S, Beal MF, Krams M, et al. Impaired mitochondrial function in psychiatric disorders. Nat Rev Neurosci. 2012;13:293–307.
Lancaster MA, Knoblich JA. Organogenesis in a dish: modeling development and disease using organoid technologies. Science (New York, NY). 2014;345:1247125.
Lancaster MA, Renner M, Martin CA, Wenzel D, Bicknell LS, Hurles ME, et al. Cerebral organoids model human brain development and microcephaly. Nature. 2013;501:373–9.
Paşca AM, Sloan SA, Clarke LE, Tian Y, Makinson CD, Huber N, et al. Functional cortical neurons and astrocytes from human pluripotent stem cells in 3D culture. Nat Methods. 2015;12:671–8.
Quadrato G, Nguyen T, Macosko EZ, Sherwood JL, Min Yang S, Berger DR, et al. Cell diversity and network dynamics in photosensitive human brain organoids. Nature. 2017;545:48–53.
Akkouh IA, Ueland T, Szabo A, Hughes T, Smeland OB, Andreassen OA. et al. Longitudinal transcriptomic analysis of human cortical spheroids identifies axonal dysregulation in the prenatal brain as a mediator of genetic risk for schizophrenia. Biol Psychiatry. 2024;95:687–98.
Yang G, Ullah HMA, Parker E, Gorsi B, Libowitz M, Maguire C. et al. Neurite outgrowth deficits caused by rare PLXNB1 mutation in pediatric bipolar disorder. Mol Psychiatry. 2023;28:2525–39.
Osete JR, Akkouh IA, Ievglevskyi O, Vandenberghe M, de Assis DR, Ueland T, et al. Transcriptional and functional effects of lithium in bipolar disorder iPSC-derived cortical spheroids. Mol Psychiatry. 2023;28:3033–43.
Notaras M, Lodhi A, Dündar F, Collier P, Sayles NM, Tilgner H, et al. Schizophrenia is defined by cell-specific neuropathology and multiple neurodevelopmental mechanisms in patient-derived cerebral organoids. Mol Psychiatry. 2022;27:1416–34.
Kathuria A, Lopez-Lengowski K, Jagtap SS, McPhie D, Perlis RH, Cohen BM, et al. Transcriptomic landscape and functional characterization of induced pluripotent stem cell-derived cerebral organoids in schizophrenia. JAMA Psychiatry. 2020;77:745–54.
Stachowiak EK, Benson CA, Narla ST, Dimitri A, Chuye LEB, Dhiman S, et al. Cerebral organoids reveal early cortical maldevelopment in schizophrenia-computational anatomy and genomics, role of FGFR1. Transl Psychiatry. 2017;7:6.
Kathuria A, Lopez-Lengowski K, Vater M, McPhie D, Cohen BM, Karmacharya R. Transcriptome analysis and functional characterization of cerebral organoids in bipolar disorder. Genome Med. 2020;12:34.
Simonsen C, Sundet K, Vaskinn A, Birkenaes AB, Engh JA, Faerden A, et al. Neurocognitive dysfunction in bipolar and schizophrenia spectrum disorders depends on history of psychosis rather than diagnostic group. Schizophr Bull. 2011;37:73–83.
Pentz AB, O’Connel KS, van Jole O, Timpe CMF, Slapo NB, Melle I, et al. Mismatch negativity and polygenic risk scores for schizophrenia and bipolar disorder. Schizophr Res. 2024;264:314–26.
Delorme A, Makeig S. EEGLAB: an open-source toolbox for analysis of single trial EEG dynamics. J Neurosci Methods. 2004;134:139–121.
Bigdely-Shamlo N, Mullen T, Kothe C, Su KM, Robbins KA. The PREP pipeline: standardized preprocessing for large-scale EEG analysis. Front Neuroinform. 2015;9:16.
Pion-Tonachini L, Kreutz-Delgado K, Makeig S. ICLabel: An automated electroencephalographic independent component classifier, dataset, and website. Neuroimage. 2019;198:181–97.
Valstad M, Moberget T, Roelfs D, Slapo NB, Timpe CMF, Beck D, et al. Experience-dependent modulation of the visual evoked potential: Testing effect sizes, retention over time, and associations with age in 415 healthy individuals. Neuroimage. 2020;223:117302.
Garrido MI, Friston KJ, Kiebel SJ, Stephan KE, Baldeweg T, Kilner JM. The functional anatomy of the MMN: a DCM study of the roving paradigm. Neuroimage. 2008;42:936–44.
Baldeweg T, Klugman A, Gruzelier J, Hirsch SR. Mismatch negativity potentials and cognitive impairment in schizophrenia. Schizophr Res. 2004;69:203–17.
Yoon SJ, Elahi LS, Pașca AM, Marton RM, Gordon A, Revah O, et al. Reliability of human cortical organoid generation. Nat Methods. 2019;16:75–8.
Pentz AB, Timpe CMF, Normann EM, Slapo NB, Melle I, Lagerberg TV, et al. Mismatch negativity in schizophrenia spectrum and bipolar disorders: Group and sex differences and associations with symptom severity. Schizophr Res. 2023;261:80–93.
Moriyama Y, Yamamoto A. Glutamatergic chemical transmission: look! Here, there, and anywhere. J Biochem. 2004;135:155–63.
Wilson NR, Kang J, Hueske EV, Leung T, Varoqui H, Murnick JG, et al. Presynaptic regulation of quantal size by the vesicular glutamate transporter VGLUT1. J Neurosci. 2005;25:6221–34.
Liguz-Lecznar M, Skangiel-Kramska J. Vesicular glutamate transporters (VGLUTs): the three musketeers of glutamatergic system. Acta Neurobiol Exp (Wars). 2007;67:207–18.
Balschun D, Moechars D, Callaerts-Vegh Z, Vermaercke B, Van Acker N, Andries L, et al. Vesicular glutamate transporter VGLUT1 has a role in hippocampal long-term potentiation and spatial reversal learning. Cereb Cortex. 2010;20:684–93.
Berry CT, Sceniak MP, Zhou L, Sabo SL. Developmental up-regulation of vesicular glutamate transporter-1 promotes neocortical presynaptic terminal development. PLoS ONE. 2012;7:e50911.
Smith RE, Haroutunian V, Davis KL, Meador-Woodruff JH. Vesicular glutamate transporter transcript expression in the thalamus in schizophrenia. Neuroreport. 2001;12:2885–7.
Oni-Orisan A, Kristiansen LV, Haroutunian V, Meador-Woodruff JH, McCullumsmith RE. Altered Vesicular Glutamate Transporter Expression in the Anterior Cingulate Cortex in Schizophrenia. Biol Psychiatry. 2008;63:766–75.
Gilabert-Juan J, Varea E, Guirado R, Blasco-Ibáñez JM, Crespo C, Nácher J. Alterations in the expression of PSA-NCAM and synaptic proteins in the dorsolateral prefrontal cortex of psychiatric disorder patients. Neurosci Lett. 2012;530:97–102.
Eastwood SL, Harrison PJ. Decreased expression of vesicular glutamate transporter 1 and complexin II mRNAs in schizophrenia: further evidence for a synaptic pathology affecting glutamate neurons. Schizophr Res. 2005;73:159–72.
Uezato A, Meador-Woodruff JH, McCullumsmith RE. Vesicular glutamate transporter mRNA expression in the medial temporal lobe in major depressive disorder, bipolar disorder, and schizophrenia. Bipolar Disord. 2009;11:711–25.
Schoonover KE, Miller NE, Fish KN, Lewis DA. Scaling of smaller pyramidal neuron size and lower energy production in schizophrenia. Neurobiol Dis. 2024;191:106394.
Ni P, Noh H, Park GH, Shao Z, Guan Y, Park JM, et al. iPSC-derived homogeneous populations of developing schizophrenia cortical interneurons have compromised mitochondrial function. Mol Psychiatry. 2020;25:2873–88.
Kathuria A, Lopez-Lengowski K, McPhie D, Cohen BM, Karmacharya R. Disease-specific differences in gene expression, mitochondrial function and mitochondria-endoplasmic reticulum interactions in iPSC-derived cerebral organoids and cortical neurons in schizophrenia and bipolar disorder. Discover mental health. 2023;3:8.
Sullivan CR, Mielnik CA, Funk A, O’Donovan SM, Bentea E, Pletnikov M, et al. Measurement of lactate levels in postmortem brain, iPSCs, and animal models of schizophrenia. Sci Rep. 2019;9:5087.
Sakaguchi H, Ozaki Y, Ashida T, Matsubara T, Oishi N, Kihara S, et al. Self-organized synchronous calcium transients in a cultured human neural network derived from cerebral organoids. Stem Cell Reports. 2019;13:458–73.
Trujillo CA, Gao R, Negraes PD, Gu J, Buchanan J, Preissl S, et al. Complex oscillatory waves emerging from cortical organoids model early human brain network development. Cell Stem Cell. 2019;25:558–69.e557.
Pekkurnaz G, Wang X. Mitochondrial heterogeneity and homeostasis through the lens of a neuron. Nature Metabolism. 2022;4:802–12.
Inan M, Zhao M, Manuszak M, Karakaya C, Rajadhyaksha AM, Pickel VM, et al. Energy deficit in parvalbumin neurons leads to circuit dysfunction, impaired sensory gating and social disability. Neurobiol Dis. 2016;93:35–46.
Robicsek O, Ene HM, Karry R, Ytzhaki O, Asor E, McPhie D, et al. Isolated mitochondria transfer improves neuronal differentiation of schizophrenia-derived induced pluripotent stem cells and rescues deficits in a rat model of the disorder. Schizophr Bull. 2018;44:432–42.
Spooner RK, Taylor BK, Ahmad IM, Dyball KN, Emanuel K, Fox HS, et al. Neural oscillatory activity serving sensorimotor control is predicted by superoxide-sensitive mitochondrial redox environments. Proc Natl Acad Sci USA. 2021;118:e2104569118.
Birnbaum R, Weinberger DR. Genetic insights into the neurodevelopmental origins of schizophrenia. Nat Rev Neurosci. 2017;18:727–40.
Kloiber S, Rosenblat JD, Husain MI, Ortiz A, Berk M, Quevedo J, et al. Neurodevelopmental pathways in bipolar disorder. Neurosci Biobehav Rev. 2020;112:213–26.
Chung DW, Geramita MA, Lewis DA. Synaptic variability and cortical gamma oscillation power in schizophrenia. Am J Psychiatry. 2022;179:277–87.
Van Derveer AB, Bastos G, Ferrell AD, Gallimore CG, Greene ML, Holmes JT, et al. A role for somatostatin-positive interneurons in neuro-oscillatory and information processing deficits in schizophrenia. Schizophr Bull. 2021;47:1385–98.
Dienel SJ, Fish KN, Lewis DA The nature of prefrontal cortical GABA neuron alterations in schizophrenia: markedly lower somatostatin and parvalbumin gene expression without missing neurons. The American journal of psychiatry 2023: 180:495-507.
Javitt DC, Kantrowitz JT. The glutamate/N-methyl-d-aspartate receptor (NMDAR) model of schizophrenia at 35: On the path from syndrome to disease. Schizophr Res. 2022;242:56–61.
Booker SA, Wyllie DJA. NMDA receptor function in inhibitory neurons. Neuropharmacology. 2021;196:108609.
Acknowledgements
The research leading to these results has received funding from the South-Eastern Norway Regional Health Authority (#2018094, #2022087), EU’s Horizon Psych-STRATA project (#101057454), and the Research Council of Norway (#223273, #248828, #274359, #295679). D.R.A. has received funding from the European Union’s Horizon 2020 Research and Innovation Programme under the Marie Skłodowska-Curie Grant Agreement No 801133. We acknowledge the Norwegian Core Facility for Human Pluripotent Stem Cells Research Centre for the reprogramming of iPSC and for the use of their LSM700 confocal microscope.
Author information
Authors and Affiliations
Contributions
Conceived and designed the analysis, DRA., SD, and TE; Collected the data, EK, DRA, ABP, JRO, OI, and MV Performed the analysis, EK, DRA, ABP, OI, JRO and MV; Writing and editing of the paper, DRA, ABP, JRO, OI, IAA, TMM, EGJ, OAA, SD, EK, TE; Supervision and funding acquisition, TE, SD and OAA All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
TE is a consultant to Sumitomo Pharma America and received speaker’s honoraria from Lundbeck and Janssen Cilag. OAA is a consultant to HealthLytix and received speaker’s honoraria from Lundbeck. The other authors declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Reis de Assis, D., Pentz, A.B., Requena Osete, J. et al. Investigating neural impairments in psychotic disorders using electroencephalography and cortical spheroids. Transl Psychiatry (2026). https://doi.org/10.1038/s41398-026-03863-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-026-03863-4