Abstract
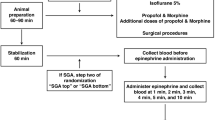
It is essential to monitor the end-tidal carbon dioxide (ETCO2) during general anesthesia and adjust the tidal volume and respiratory rate (RR). For the purpose of this study, we used a population pharmacodynamic modeling approach to establish the relationship between RR versus ETCO2 data during general anesthesia in children, and to identify the clinical variables affecting this relationship. A prospective observational study was designed to include 51 patients (aged ≤ 12 years), including users of antiepileptic drugs (levetiracetam, valproic, or phenobarbital (n = 21)) and non-users (n = 30), scheduled to receive general anesthesia during elective surgery. When the ETCO2 was at 40 mmHg, the RR was adjusted 1 breath per every 2 min until the ETCO2 was 30 mmHg and recovered to 40 mmHg. Pharmacodynamic analysis using a sigmoid Emax model was performed to assess the RR-ETCO2 relationship. As RR varied from 3 to 37 breaths per minute, the ETCO2 changed from 40 to 30 mmHg. Hysteresis between the RR and ETCO2 was observed and accounted for when the model was developed. The Ce50 (RR to achieve 50% of maximum decrease in ETCO2; i.e. 35 mmHg) was 20.5 in non-users of antiepileptic drugs and 14.9 in those on antiepileptic drug medication. The values of γ (the steepness of the concentration-response relation curve) and keo (the first-order rate constant determining the equilibration between the RR and ETCO2) were 7.53 and 0.467 min-1, respectively. The Ce50 and ETCO2 data fit to a sigmoid Emax model. In conclusion, the RR required to get the target ETCO2 was much lower in children patients taking antiepileptic drugs than that of non-user children patients during the general anesthesia.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Pi X, Cui Y, Wang C, Guo L, Sun B, Shi J, et al. Low tidal volume with PEEP and recruitment expedite the recovery of pulmonary function. Int J Clin Exp Pathol. 2015;8:14305–14.
Xie P, Li Z, Tian Z. The optimal combination of mechanical ventilator parameters under general anesthesia in obese patients undergoing laparoscopic surgery. J Clin Anesth. 2016;34:290–4.
Bhavani-Shankar K, Moseley H, Kumar AY, Delph Y. Capnometry and anaesthesia. Can J Anaesth. 1992;39:617–32.
Razi E, Moosavi GA, Omidi K, Khakpour Saebi A, Razi A. Correlation of end-tidal carbon dioxide with arterial carbon dioxide in mechanically ventilated patients. Arch Trauma Res. 2012;1:58–62.
Onodi C, Buhler PK, Thomas J, Schmitz A, Weiss M. Arterial to end-tidal carbon dioxide difference in children undergoing mechanical ventilation of the lungs during general anaesthesia. Anaesthesia. 2017;72:1357–64.
Schnider TW, Minto CF, Shafer SL, Gambus PL, Andresen C, Goodale DB, et al. The influence of age on propofol pharmacodynamics. Anesthesiology. 1999;90:1502–16.
Ki SH, Rhim JH, Park JH, Han YJ, Cho YP, Kwon TW, et al. Quantitative analysis of the effect of end-tidal carbon dioxide on regional cerebral oxygen saturation in patients undergoing carotid endarterectomy under general anaesthesia. Br J Clin Pharmacol. 2018;84:292–300.
Ross KR, Rosen CL. Sleep and respiratory physiology in children. Clin Chest Med. 2014;35:457–67.
Boiteux C, Vorobyov I, French RJ, French C, Yarov-Yarovoy V, Allen TW. Local anesthetic and antiepileptic drug access and binding to a bacterial voltage-gated sodium channel. Proc Natl Acad Sci USA. 2014;111:13057–62.
Zamponi GW. Targeting voltage-gated calcium channels in neurological and psychiatric diseases. Nat Rev Drug Discov. 2016;15:19–34.
Leo A, Citraro R, Constanti A, De Sarro G, Russo E. Are big potassium-type Ca(2+)-activated potassium channels a viable target for the treatment of epilepsy? Expert Opin Ther Targets. 2015;19:911–26.
Schousboe A, Wellendorph P, Frolund B, Clausen RP, Krogsgaard-Larsen P. Astrocytic GABA Transporters: Pharmacological Properties and Targets for Antiepileptic Drugs. Adv Neurobiol. 2017;16:283–96.
Brodie MJ, Covanis A, Gil-Nagel A, Lerche H, Perucca E, Sills GJ, et al. Antiepileptic drug therapy: does mechanism of action matter? Epilepsy Behav. 2011;21:331–41.
Ikemoto Y, Yamashita M, Yano T. Volatile anesthetics and a volatile convulsant differentially affect GABA(A) receptor-chloride channel complex. Toxicol Lett. 1998;100-101:225–31.
Martin DC, Abraham JE, Plagenhoef M, Aronstam RS. Volatile anesthetics and NMDA receptors. Enflurane inhibition of glutamate-stimulated [3H]MK-801 binding and reversal by glycine. Neurosci Lett. 1991;132:73–6.
Joseph JD, Peng Y, Mak DO, Cheung KH, Vais H, Foskett JK, et al. General anesthetic isoflurane modulates inositol 1,4,5-trisphosphate receptor calcium channel opening. Anesthesiology. 2014;121:528–37.
Kamatchi GL, Tiwari SN, Durieux ME, Lynch C 3rd. Effects of volatile anesthetics on the direct and indirect protein kinase C-mediated enhancement of alpha1E-type Ca(2+) current in Xenopus oocytes. J Pharmacol Exp Ther. 2000;293:360–9.
Herold KF, Sanford RL, Lee W, Schultz MF, Ingolfsson HI, Andersen OS, et al. Volatile anesthetics inhibit sodium channels without altering bulk lipid bilayer properties. J Gen Physiol. 2014;144:545–60.
Magyar J, Szabo G. Effects of volatile anesthetics on the G protein-regulated muscarinic potassium channel. Mol Pharmacol. 1996;50:1520–8.
Kaisti KK, Langsjo JW, Aalto S, Oikonen V, Sipila H, Teras M, et al. Effects of sevoflurane, propofol, and adjunct nitrous oxide on regional cerebral blood flow, oxygen consumption, and blood volume in humans. Anesthesiology. 2003;99:03–13.
Bazzigaluppi P, Ebrahim AA, Weisspapir I, Stefanovic B, Carlen PL. Hungry neurons: metabolic insights on seizure dynamics. Int J Mol Sci. 2017;18:2269–82.
Miller RD, Cohen NH, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Young WL. Miller’s anesthesia. Philadelphia, PA: Elsevier/Saunders; 2015.
Author contributions
JHL and HSK designed the study; JHL, EHK, YEJ, and JTK conducted the study and collected data; JHL and HSK analyzed the data; PYK, JHL, and HSK wrote the paper; and all authors revised the paper. Population pharmacodynamic modeling reveals the impact of antiepileptic drugs on the relationship between RR and ETCO2 values during general anesthesia in children.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Appendix 1
Appendix 1
NONMEM control code
$PROB RUN# 60101 (Direct PD fit for RR vs CO2)
$DATA AED_2.csv IGNORE = #
$INPUT ID TIME CP DV GROUP SEX AGE HT WT; TIME: min; CP: respiratory rate; DV: end-tidal CO2; Group: 0 = normal group, 1 = antiepileptic group; SEX: 0 = male, 1 = female; AGE: yr; HT: cm; WT: kg
$PRED
TH1 = THETA(1)
TH2 = THETA(2)
TH3 = THETA(3)
TH4 = THETA(4)
TH5 = THETA(5)
TH6 = THETA(6)
E0 = TH1*EXP(ETA(1))
EMAX = TH2*EXP(ETA(2))
CE50 = (TH3*GROUP + TH6*(1-GROUP))*EXP(ETA(3))
GAM = TH4*EXP(ETA(4))
KE0 = TH5*EXP(ETA(5))
IF (TIME.EQ.0.OR.CP.EQ.0) THEN
CE = 0
PTIME = 0
PCP = 0
PCE = 0
ENDIF
DT = TIME-PTIME
IF (DT.EQ.0.OR.CP.EQ.0) THEN
DT1 = 1
ELSE
DT1 = DT
ENDIF
IF(CP.GT.0.AND.CP.GE.PCP) THEN
SLOPE = (CP-PCP)/DT1
DELT = DT1*SLOPE + (KE0*PCP-SLOPE)*(1-EXP(-KE0*DT1))/KE0
ENDIF
IF(CP.GT.0.AND.CP.LT.PCP) THEN
SLOPE = (LOG(CP)-LOG(PCP))/DT1
DELT = PCP*KE0/(KE0 + SLOPE)*(EXP(DT1*SLOPE)-EXP(-KE0*DT1))
ENDIF
IF (CP.GT.0.AND.DT.GT.0) THEN
CE = PCE*EXP(-KE0*DT) + DELT
ELSE
CE = PCE
ENDIF
IPRED = E0 + (EMAX - E0)*CE**GAM/(CE**GAM + CE50**GAM)
PTIME = TIME
PCP = CP
PCE = CE
W = 1
IRES = DV - IPRED
IWRES = IRES / W
Y = IPRED + W*EPS(1)
$THETA;#6
(20, 40); E0
(10, 30); EMAx
(1, 15); CE50_antiepileptic group
(1, 3); GAM
(0, 0.1); KE0
(1, 15); CE50_normal group
$OMEGA;#5
0.2; IIV_E0
0.2; IIV_EMAX
0.2; IIV_CE50
0.2; IIV_GAM
0.2; IIV_KE0
$SIGMA;#1
16; EPS
$ESTIMATION NOTBT NOOBT NOSBT SIGL = 3 NSIG = 1 MAXEVAL = 9999 PRINT = 5 METHOD = 1 INTER MSFO = 60101.MSF NOABORT
$COVARIANCE PRINT = E
$TABLE ID ETA(1) ETA(2) ETA(3) ETA(4) ETA(5)
FILE = 60101.ETA NOPRINT FIRSTONLY NOAPPEND
$TABLE ID E0 EMAX CE50 GAM KE0
FILE = 60101.PAR NOPRINT ONEHEADER NOAPPEND
$TABLE ID TIME GROUP IPRED IWRES CWRES
FILE = sdtab60101 NOPRINT ONEHEADER
$TABLE ID E0 EMAX CE50 GAM KE0 ETA(1) ETA(2) ETA(3) ETA(4) ETA(5)
FILE = patab60101 NOPRINT ONEHEADER NOAPPEND
$TABLE ID AGE HT WT
FILE = cotab60101 NOPRINT ONEHEADER NOAPPEND
$TABLE ID SEX GROUP
FILE = catab60101 NOPRINT ONEHEADER NOAPPEND
Rights and permissions
About this article
Cite this article
Lee, JH., Kang, PY., Jang, YE. et al. A pharmacodynamic model of respiratory rate and end-tidal carbon dioxide values during anesthesia in children. Acta Pharmacol Sin 40, 642–647 (2019). https://doi.org/10.1038/s41401-018-0156-x
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41401-018-0156-x
Keywords
This article is cited by
-
A pharmacodynamic model of tidal volume and inspiratory sevoflurane concentration in children during spontaneous breathing
Journal of Pharmacokinetics and Pharmacodynamics (2021)