Abstract
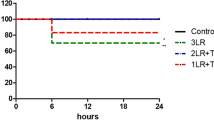
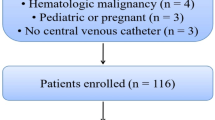
In order to maintain stable blood pressure and heart rate during surgery, anesthesiologists need to administer the appropriate amount of fluid with appropriate fluid type to the patient, then quantifying how fluid is distributed and eliminated from the body is useful for establishing a fluid administration strategy. In this study we characterized the volume kinetics of Ringer’s lactate solution in patients undergoing open gastrectomy. When propofol and remifentanil reached a pseudosteady state at the target concentration and blood pressure was stabilized following surgical stimulation, enrolled patients were administered 1000 mL of Ringer’s lactate solution for 20 min, followed by continuous infusion at a rate of 6 mL/kg/h until the time of the last blood collection for volume kinetic analysis. Arterial blood samples were collected to measure the hemoglobin concentration at different time points. The change in hemoglobin-derived plasma dilution induced by the administration of Ringer’s lactate solution was evaluated by nonlinear mixed effects modeling. Three hundred and twenty-three plasma dilution data points from 27 patients were used to determine the pharmacokinetic characteristics of Ringer’s lactate solution. A two-volume model best described the pharmacokinetics of Ringer’s lactate solution. The mean arterial pressure (MAP) and body weight (WT) were significant covariates for the elimination clearance (kr) and central volume of distribution at baseline (Vc0), respectively. The parameter estimates were as follows: kr (mL/min) = 124 + (MAP/70)14.2, Vc0 (mL) = 0.95 + 3440 × (WT/63), Vt0 (mL) = 2730, and kt (mL/min) = 181. A higher MAP was associated with a greater elimination clearance and, consequently, less water accumulation in the interstitium. As body weight increases, volume expansion in the blood vessels increases.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Aga Z, Machina M, McCluskey SA. Greater intravenous fluid volumes are associated with prolonged recovery after colorectal surgery: a retrospective cohort study. Br J Anaesth. 2016;116:804–10.
Li Y, He R, Ying X, Hahn RG. Ringer’s lactate, but not hydroxyethyl starch, prolongs the food intolerance time after major abdominal surgery; an open-labelled clinical trial. BMC Anesthesiol. 2015;15:72.
Schol PB, Terink IM, Lance MD, Scheepers HC. Liberal or restrictive fluid management during elective surgery: a systematic review and meta-analysis. J Clin Anesth. 2016;35:26–39.
Weinberg L, Ianno D, Churilov L, Chao I, Scurrah N, Rachbuch C, et al. Restrictive intraoperative fluid optimisation algorithm improves outcomes in patients undergoing pancreaticoduodenectomy: a prospective multicentre randomized controlled trial. PLoS ONE. 2017;12:e0183313.
Hahn RG. Volume kinetics for infusion fluids. Anesthesiology. 2010;113:470–81.
Stahle L, Nilsson A, Hahn RG. Modelling the volume of expandable body fluid spaces during i.v. fluid therapy. Br J Anaesth. 1997;78:138–43.
Choi BM, Lee YH, An SM, Lee SH, Lee EK, Noh GJ. Population pharmacokinetics and analgesic potency of oxycodone. Br J Clin Pharmacol. 2017;83:314–25.
Hahn RG. Arterial pressure and the rate of elimination of crystalloid fluid. Anesth Analg. 2017;124:1824–33.
Li Y, Xiaozhu Z, Guomei R, Qiannan D, Hahn RG. Effects of vasoactive drugs on crystalloid fluid kinetics in septic sheep. PLoS ONE. 2017;12:e0172361.
Kim YK, Chin JH, Kang SJ, Jun IG, Song JG, Jeong SM, et al. Association between central venous pressure and blood loss during hepatic resection in 984 living donors. Acta Anaesthesiol Scand. 2009;53:601–6.
Beal S, Sheiner L. NONMEM user’s guides introduction to NONMEM 7 Version 7.1.2. San Francisco: NONMEM Project Group, University of California; 2009. p. 9–10.
Svensen C, Hahn RG. Volume kinetics of Ringer solution, dextran 70, and hypertonic saline in male volunteers. Anesthesiology. 1997;87:204–12.
Mosteller RD. Simplified calculation of body-surface area. N Engl J Med. 1987;317:1098.
Janmahasatian S, Duffull SB, Ash S, Ward LC, Byrne NM, Green B. Quantification of lean bodyweight. Clin Pharmacokinet. 2005;44:1051–65.
Robinson JD, Lupkiewicz SM, Palenik L, Lopez LM, Ariet M. Determination of ideal body weight for drug dosage calculations. Am J Hosp Pharm. 1983;40:1016–9.
Choi BM, Lee HG, Byon HJ, Lee SH, Lee EK, Kim HS, et al. Population pharmacokinetic and pharmacodynamic model of propofol externally validated in children. J Pharmacokinet Pharmacodyn. 2015;42:163–77.
Wahlby U, Jonsson EN, Karlsson MO. Assessment of actual significance levels for covariate effects in NONMEM. J Pharmacokinet Pharmacodyn. 2001;28:231–52.
Marsh B, White M, Morton N, Kenny GN. Pharmacokinetic model driven infusion of propofol in children. Br J Anaesth. 1991;67:41–8.
Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, et al. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2005;24:466–77.
Myles PS, Bellomo R, Corcoran T, Forbes A, Peyton P, Story D, et al. Restrictive versus liberal fluid therapy for major abdominal surgery. N Engl J Med. 2018;378:2263–74.
Olsson J, Svensen CH, Hahn RG. The volume kinetics of acetated Ringer’s solution during laparoscopic cholecystectomy. Anesth Analg. 2004;99:1854–60. Table of contents.
Hahn RG, Drobin D, Zdolsek J. Distribution of crystalloid fluid changes with the rate of infusion: a population-based study. Acta Anaesthesiol Scand. 2016;60:569–78.
Hahn RG, Resby M. Volume kinetics of Ringer’s solution and dextran 3% during induction of spinal anaesthesia for caesarean section. Can J Anaesth. 1998;45:443–51.
Ewaldsson CA, Hahn RG. Volume kinetics of Ringer’s solution during induction of spinal and general anaesthesia. Br J Anaesth. 2001;87:406–14.
Acknowledgements
This study was supported by a Student Research Grant (17) from the University of Ulsan College of Medicine, Seoul, Korea. We thank Dr. Joon Seo Lim from the Scientific Publications Team at Asan Medical Center for his editorial assistance in preparing this manuscript.
Author contributions
J.-H.L., Y.-J.C., B.-M.C., and S.-H.L. designed the study; J.-H.R., Y.-H.L., S.T.Oh., and K.-T.C. collected the data; J.-H.L., Y.-J.C., B.-M.C., S.-H.L., and G.-J.N. performed the data analysis and interpretation. All authors contributed to the writing of the manuscript, provided critical revisions, and approved the final version.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Lee, JH., Choo, YJ., Lee, YH. et al. Population-based volume kinetics of Ringer’s lactate solution in patients undergoing open gastrectomy. Acta Pharmacol Sin 40, 710–716 (2019). https://doi.org/10.1038/s41401-018-0179-3
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41401-018-0179-3
Keywords
This article is cited by
-
Volume kinetics in a translational porcine model of stabilized sepsis with fluid accumulation
Critical Care (2025)
-
Effects of rapid fluid infusion on hemoglobin concentration: a systematic review and meta-analysis
Critical Care (2022)
-
Population-based volume kinetics of crystalloids and colloids in healthy volunteers
Scientific Reports (2019)