Abstract
Forsythin extracted from Forsythiae Fructus is widely used to treat fever caused by the common cold or influenza in China, Japan and Korea. The present study aimed to analyze the pharmacokinetics, metabolism and excretion routes of forsythin in humans and determine the major enzymes and transporters involved in these processes. After a single oral administration, forsythin underwent extensive metabolism via hydrolysis and further sulfation. In total, 3 of the 13 metabolites were confirmed by comparison to reference substances, i.e., aglycone M1, M1 sulfate (M2), and M1 glucuronide (M7). Hydrolysis was the initial and main metabolic pathway of the parent compound, followed by extensive sulfation to form M2 and a reduced level of glucuronidation to form M7. In addition, the plasma exposure of M2 and M7 were 86- and 4.2-fold higher than that of forsythin. Within 48 h, ~75.1% of the administered dose was found in urine, with M2 accounting for 71.6%. Further phenotyping experiments revealed that sulfotransferase 1A1 and UDP-glucuronosyltransferase 1A8 were the most active hepatic enzymes involved in the formation of M2 and M7, respectively. The in vitro kinetic study provided direct evidence that M1 showed a preference for sulfation. Sulfated conjugate M2 was identified as a specific substrate of organic anion transporter 3, which could facilitate the renal excretion of M2. Altogether, our study demonstrated that sulfation dominated the metabolism and pharmacokinetics of forsythin, while the sulfate conjugate was excreted mainly in the urine.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Wang Z, Xia Q, Liu X, Liu W, Huang W, Mei X, et al. Phytochemistry, pharmacology, quality control and future research of forsythia suspensa (Thunb.) Vahl: a review. J Ethnopharmacol. 2018;210:318–39.
Ozaki Y, Rui J, Tang Y, Satake M. Antiinflammatory effect of forsythia suspensa vahl and its active fraction. Biol Pharm Bull. 1997;20:861–64.
Chinese Pharmacopoeia Commission. Pharmacopoeia of the People’s Republic of China. China Medical Science Press; 2015.
Han Z, Lei XL, Zhang H, Liu L, Chen ZS, Yang W, et al. Evaluating the safety of forsythin from forsythia suspensa leaves by acute and sub-chronic oral administration in rodent models. Asian Pac J Trop Med. 2017;10:47–51.
Rowland A, Miners JO, Mackenzie PI. The UDP-glucuronosyltransferases: their role in drug metabolism and detoxification. Int J Biochem Cell Biol. 2013;45:1121–32.
Suiko M, Kurogi K, Hashiguchi T, Sakakibara Y, Liu MC. Updated perspectives on the cytosolic sulfotransferases (SULTs) and SULT-mediated sulfation. Biosci Biotechnol Biochem. 2017;81:63–72.
Chinese Pharmacopoeia Commission. Guidance for bioanalytical method validation, Pharmacopoeia of the People’s Republic of China. China Med Sci Press. 2015;4:363–8.
Zhong K, Li XL, Xie C, Zhang YF, Zhong DF, Chen XY. Effects of renal impairment on the pharmacokinetics of morinidazole: uptake transporter-mediated renal clearance of the conjugated metabolites. Antimicrob Agents Chemother. 2014;58:4153–61.
Riches Z, Stanley EL, Bloomer JC, Coughtrie MW. Quantitative evaluation of the expression and activity of five major sulfotransferases (SULTs) in human tissues: the SULT “pie”. Drug Metab Dispos. 2009;37:2255–61.
Roberts MS, Magnusson BM, Burczynski FJ, Weiss M. Enterohpatic circulation. Clin Pharmacokinet. 2002;41:751–90.
Wu B, Kulkarni K, Basu S, Zhang S, Hu M. First-pass metabolism via UDP-glucuronosyltransferase: a barrier to oral bioavailability of phenolics. J Pharm Sci. 2011;100:3655–81.
Yang G, Ge S, Singh R, Basu S, Shatzer K, Zen M, et al. Glucuronidation: driving factors and their impact on glucuronide disposition. Drug Metab Rev. 2017;49:105–38.
Andersen G, Christrup L, Sjøgren P. Among morphine metabolism, pain and side effects during long-term treatment: an update. J Pain Symptom Manag. 2003;25:74–91.
Luo CF, Cai B, Hou N, Yuan M, Liu SM, Ji H, et al. UDP-glucuronosyltransferase 1A1 is the principal enzyme responsible for puerarin metabolism in human liver microsomes. Arch Toxicol. 2012;86:1681–90.
Tian X, Huo X, Dong P, Wu B, Wang X, Wang C, et al. Sulfation of melatonin: enzymatic characterization, differences of organs, species and genders, and bioactivity variation. Biochem Pharmacol. 2015;94:282–96.
Barbosa ACS, Feng Y, Yu C, Huang M, Xie W. Estrogen sulfotransferase in the metabolism of estrogenic drugs and in the pathogenesis of diseases. Expert Opin Drug Metab Toxicol. 2019;15:329–39.
Liu Y, Hu M. Absorption and metabolism of flavonoids in the Caco-2 cell culture model and a perused rat intestinal model. Drug Metab Dispos. 2002;30:370.
Hu M, Chen J, Lin H. Metabolism of flavonoids via enteric recycling: mechanistic studies of disposition of apigenin in the Caco-2 cell culture model. J Pharmacol Exp Ther. 2003;307:314–21.
J Carlini E, B Raftogianis R, Wood T, Jin F, Zheng W, Rebbeck T, et al. Sulfation pharmacogenetics: SULT1A1 and SULT1A2 allele frequencies in Caucasian, Chinese and African-American subjects. Pharmacogenetics. 2001;11:57–68.
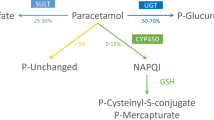
Rasool MI, Bairam AF, Gohal SA, El Daibani AA, Alherz FA, Abunnaja MS, et al. Effects of the human SULT1A1 polymorphisms on the sulfation of acetaminophen, O-desmethylnaproxen, and tapentadol. Pharmacol Rep. 2019;71:257–65.
Honma W, Shimada M, Sasano H, Ozawa S, Miyata M, Nagata K, et al. Phenol sulfotransferase, ST1A3, as the main enzyme catalyzing sulfation of troglitazone in human liver. Drug Metab Dispos. 2002;30:944–49.
Morrissey KM, Stocker SL, Wittwer MB, Xu L, Giacomini KM. Renal transporters in drug development. Annu Rev Pharmacol Toxicol. 2013;53:503–29.
Schwenk MH, Pai AB. Drug transporter function-implications in CKD. Adv Chronic Kidney Dis. 2016;23:76–81.
Kong FD, Pang XY, Zhong K, Guo ZT, Li XL, Zhong DF, et al. Increased plasma exposures of conjugated metabolites of morinidazole in renal failure patients: a critical role of uremic toxins. Drug Metab Dispos. 2017;45:593–603.
Kearney BP, Yale K, Shah J, Zhong L, Flaherty JF. Pharmacokinetics and dosing recommendations of tenofovir disoproxil fumarate in hepatic or renal impairment. Clin Pharmacokinet. 2006;45:1115–24.
Acknowledgements
This study was supported by the National Natural Science Foundation of China (grant nos. 81521005 and 81903701) and the National Key Research Project of the Chinese Academy of Sciences (grant no. XDA12050306).
Author information
Authors and Affiliations
Contributions
LLP, XXD, LF, and DFZ participated in research design. LLP and YY conducted experiments. MH, SW, and LF contributed new reagents or analytic tools. LLP and YY performed data analysis. YHD, CYL, and HZ participated in clinical trials. LLP, XXD, and DFZ contributed to the writing of the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests. The authors alone are responsible for the content and writing of this article.
Supplementary information
Rights and permissions
About this article
Cite this article
Pan, Ll., Yang, Y., Hui, M. et al. Sulfation predominates the pharmacokinetics, metabolism, and excretion of forsythin in humans: major enzymes and transporters identified. Acta Pharmacol Sin 42, 311–322 (2021). https://doi.org/10.1038/s41401-020-0481-8
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41401-020-0481-8