Abstract
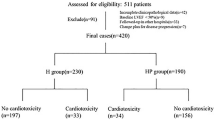
Fragment crystallizable gamma receptors (FcγRs) mediate various cellular responses with significant cardiovascular implications. They contribute to the anticancer activity of trastuzumab (TRZ), a recombinant humanized monoclonal antibody that interferes with human epidermal growth factor receptor 2 (HER2), thereby blocking its physiological function in cardiac cells. This is responsible for cardiac complications that hamper TRZ clinical application. In this study we investigated the involvement of FcγRs in the TRZ cardiotoxicity. We used a recombinant antigen-binding fragment (Fab) of TRZ (rFab-HER2) to examine whether the absence of the Fc region resulted in fewer cardiomyocyte toxicity while preserving TRZ’s ability to inhibit HER2. When exposed to rFab-HER2, AC16 human adult ventricular cardiomyocytes were less vulnerable to damage and death, than to TRZ. Specifically, TRZ exhibited cytotoxicity at a lower concentration (150 µg/mL, corresponding to ~1 µM) compared to rFab-HER2 (250 µg/mL, corresponding to ~5 µM). Like TRZ, rFab-HER2 negatively modulated HER2 levels in cardiomyocyte (without inducing cytotoxic activity in BJ human fibroblast cells that either did not express or express very low levels of HER2) and inhibited the downstream ERK/AKT cascades. But rFab-HER2 did not alter cardiomyocyte mitochondrial dynamic balance, and affect apoptosis and inflammation, while it limited cytosolic and mitochondrial ROS indicators. On contrary, the Fc region (50−250 μg/mL) exerted direct cytotoxic action on cardiomyocytes (but not on human fibroblasts that lacked Fc receptors). TRZ (150 μg/mL) markedly upregulated the expression level of FcγRIIA (a FcγRs strongly involved in TRZ-induced antibody-dependent cellular toxicity) in cardiomyocytes, whereas the Fab fragment (150 μg/mL) had no effect. Our results demonstrate that Fc region plays an important pathogenic role in TRZ-induced cardiomyocyte toxicity. In addition, targeting FcγRIIA might contribute to the off-target effects of TRZ therapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Sawyers C. Targeted cancer therapy. Nature. 2004;432:294–7.
Hahn VS, Zhang KW, Sun L, Narayan V, Lenihan DJ, Ky B. Heart failure with targeted cancer therapies: mechanisms and cardioprotection. Circ Res. 2021;128:1576–93.
Touyz RM, Herrmann J. Cardiotoxicity with vascular endothelial growth factor inhibitor therapy. Npj Precis Oncol. 2018;2:13.
Rocca C, De Francesco EM, Pasqua T, Granieri MC, De Bartolo A, Gallo Cantafio ME, et al. Mitochondrial determinants of anti-cancer drug-induced cardiotoxicity. Biomedicines. 2022;10:520.
Rocca C, Soda T, De Francesco EM, Fiorillo M, Moccia F, Viglietto G, et al. Mitochondrial dysfunction at the crossroad of cardiovascular diseases and cancer. J Transl Med. 2023;21:635.
Wang J, Xu B. Targeted therapeutic options and future perspectives for HER2-positive breast cancer. Signal Transduct Target Ther. 2019;4:34.
Moasser MM. The oncogene HER2: its signaling and transforming functions and its role in human cancer pathogenesis. Oncogene. 2007;26:6469–87.
Meric-Bernstam F, Johnson AM, Dumbrava EEI, Raghav K, Balaji K, Bhatt M, et al. Advances in HER2-targeted therapy: novel agents and opportunities beyond breast and gastric cancer. Clin Cancer Res. 2019;25:2033–41.
Romond EH, Jeong J-H, Rastogi P, Swain SM, Geyer CE, Ewer MS, et al. Seven-year follow-up assessment of cardiac function in NSABP B-31, a randomized trial comparing doxorubicin and cyclophosphamide followed by Paclitaxel (ACP) With ACP Plus Trastuzumab as adjuvant therapy for patients with node-positive, human epidermal Gr. J Clin Oncol. 2012;30:3792–9.
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of Chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344:783–92.
Hussain Y, Drill E, Dang CT, Liu JE, Steingart RM, Yu AF. Cardiac outcomes of trastuzumab therapy in patients with HER2-positive breast cancer and reduced left ventricular ejection fraction. Breast Cancer Res Treat. 2019;175:239–46.
Telli ML, Hunt SA, Carlson RW, Guardino AE. Trastuzumab-related cardiotoxicity: calling into question the concept of reversibility. J Clin Oncol. 2007;25:3525–33.
Rocca C, Pasqua T, Cerra MC, Angelone T. Cardiac damage in anthracyclines therapy: focus on oxidative stress and inflammation. Antioxid Redox Signal. 2020;32:1081–97.
Crone SA, Zhao YY, Fan L, Gu Y, Minamisawa S, Liu Y, et al. ErbB2 is essential in the prevention of dilated cardiomyopathy. Nat Med. 2002;8:459–65.
Clynes RA, Towers TL, Presta LG, Ravetch JV. Inhibitory Fc receptors modulate in vivo cytoxicity against tumor targets. Nat Med. 2000;6:443–6.
Méndez-Valdés G, Gómez-Hevia F, Bragato MC, Lillo-Moya J, Rojas-Solé C, Saso L, et al. Antioxidant protection against Trastuzumab cardiotoxicity in breast cancer therapy. Antioxidants. 2023;12:457.
Musolino A, Gradishar WJ, Rugo HS, Nordstrom JL, Rock EP, Arnaldez F, et al. Role of Fcγ receptors in HER2-targeted breast cancer therapy. J Immunother Cancer. 2022;10:e003171.
Wang D, Wei X, Wang Z, Lu Y, Shi S, Wang N, et al. FcγRIIA and IIIA polymorphisms predict clinical outcome of trastuzumab-treated metastatic gastric cancer. Onco Targets Ther. 2017;10:5065–76.
Musolino A, Naldi N, Bortesi B, Pezzuolo D, Capelletti M, Missale G, et al. Immunoglobulin G Fragment C receptor polymorphisms and clinical efficacy of Trastuzumab-based therapy in patients with HER-2/neu–positive metastatic breast cancer. J Clin Oncol. 2008;26:1789–96.
Staudt A, Eichler P, Trimpert C, Felix SB, Greinacher A. FcγReceptors IIa on cardiomyocytes and their potential functional relevance in dilated cardiomyopathy. J Am Coll Cardiol. 2007;49:1684–92.
Patel P, Michael JV, Naik UP, McKenzie SE. Platelet FcγRIIA in immunity and thrombosis: adaptive immunothrombosis. J Thromb Haemost. 2021;19:1149–60.
Kholodenko RV, Kalinovsky DV, Doronin II, Ponomarev ED, Kholodenko IV. Antibody fragments as potential biopharmaceuticals for cancer therapy: success and limitations. Curr Med Chem. 2019;26:396–426.
Selis F, Sandomenico A, Cantile M, Sanna R, Calvanese L, Falcigno L, et al. Generation and testing of engineered multimeric Fabs of trastuzumab. Int J Biol Macromol. 2020;164:4516–31.
Davidson M, Nesti C, Palenzuela L, Walker W, Hernandez E, Protas L, et al. Novel cell lines derived from adult human ventricular cardiomyocytes. J Mol Cell Cardiol. 2005;39:133–47.
Liang JL, Xiao DZ, Liu XY, Lin QX, Shan ZX, Zhu JN, et al. High glucose induces apoptosis in AC16 human cardiomyocytes via macrophage migration inhibitory factor and c-Jun N-terminal kinase. Clin Exp Pharmacol Physiol. 2010;37:969–73.
De Bartolo A, Pasqua T, Romeo N, Rago V, Perrotta I, Giordano F, et al. The redox-active defensive Selenoprotein T as a novel stress sensor protein playing a key role in the pathophysiology of heart failure. J Transl Med. 2024;22:375.
Zheng Y, Lakshmanan S. Dose-dependent efficacy of umbelliferone and gelatin-coated ZnO/ZnS core-shell nanoparticles: a novel arthritis agent for severe knee arthritis. Oxid Med Cell Longev. 2022;2022:1–15.
Grande F, De Bartolo A, Occhiuzzi MA, Caruso A, Rocca C, Pasqua T, et al. Carbazole and simplified derivatives: novel tools toward β-adrenergic receptors targeting. Appl Sci. 2021;11:5486.
Rocca C, De Bartolo A, Grande F, Rizzuti B, Pasqua T, Giordano F, et al. Cateslytin abrogates lipopolysaccharide-induced cardiomyocyte injury by reducing inflammation and oxidative stress through toll like receptor 4 interaction. Int Immunopharmacol. 2021;94:107487.
McQueen MJ. Optimal assay of LDH and α-HBD at 37 °C. Ann Clin Biochem Int J Lab Med. 1972;9:21–5.
Rocca C, De Bartolo A, Guzzi R, Crocco MC, Rago V, Romeo N, et al. Palmitate-induced cardiac lipotoxicity is relieved by the redox-active motif of SELENOT through improving mitochondrial function and regulating metabolic state. Cells. 2023;12:1042.
Rocca C, Scavello F, Colombo B, Gasparri AM, Dallatomasina A, Granieri MC, et al. Physiological levels of chromogranin A prevent doxorubicin‐induced cardiotoxicity without impairing its anticancer activity. FASEB J. 2019;33:7734–47.
Rocca C, De Bartolo A, Granieri MC, Rago V, Amelio D, Falbo F, et al. The antioxidant selenoprotein T Mimetic, PSELT, induces preconditioning-like myocardial protection by relieving endoplasmic-reticulum stress. Antioxidants. 2022;11:571.
Gastaldi S, Rocca C, Gianquinto E, Granieri MC, Boscaro V, Blua F, et al. Discovery of a novel 1,3,4-oxadiazol-2-one-based NLRP3 inhibitor as a pharmacological agent to mitigate cardiac and metabolic complications in an experimental model of diet-induced metaflammation. Eur J Med Chem. 2023;257:115542.
Rocca C, Boukhzar L, Granieri MC, Alsharif I, Mazza R, Lefranc B, et al. A selenoprotein T‐derived peptide protects the heart against ischaemia/reperfusion injury through inhibition of apoptosis and oxidative stress. Acta Physiol. 2018;223:e13067.
Giustarini D, Rossi R, Milzani A, Dalle‐Donne I. Nitrite and nitrate measurement by griess reagent in human plasma: evaluation of interferences and standardization. Methods Enzymol. 2008;440:361–80.
Rocca C, Grande F, Granieri MC, Colombo B, De Bartolo A, Giordano F, et al. The chromogranin A 1‐373 fragment reveals how a single change in the protein sequence exerts strong cardioregulatory effects by engaging neuropilin‐1. Acta Physiol. 2021;231:e13570.
Kawakami T, Kawamura K, Fujimori K, Koike A, Amano F. Influence of the culture medium on the production of nitric oxide and expression of inducible nitric oxide synthase by activated macrophages in vitro. Biochem Biophys Rep. 2016;5:328–34.
Yan B, Sun Y, Wang J. Depletion of ubiA prenyltransferase domain containing 1 expression promotes angiotensin II-induced hypertrophic response in AC16 human myocardial cells via modulating the expression levels of coenzyme Q10 and endothelial nitric oxide synthase. Mol Med Rep. 2017;16:6910–5.
Kitani T, Ong SG, Lam CK, Rhee JW, Zhang JZ, Oikonomopoulos A, et al. Human-induced pluripotent stem cell model of Trastuzumab-induced cardiac dysfunction in patients with breast cancer. Circulation. 2019;139:2451–65.
Su Z, Liu S, Zou Y, Shan L, Yu M, Xie S, et al. Trastuzumab-induced human cardiomyocyte damage through the Notch2/JAK2/STAT3 pathway. Clinics. 2023;78:100268.
Arlein WJ, Shearer JD, Caldwell MD. Continuity between wound macrophage and fibroblast phenotype: analysis of wound fibroblast phagocytosis. Am J Physiol Integr Comp Physiol. 1998;275:R1041–8.
Boonnak K, Slike BM, Donofrio GC, Marovich MA. Human FcγRII cytoplasmic domains differentially influence antibody-mediated dengue virus infection. J Immunol. 2013;190:5659–65.
Bloom MW, Hamo CE, Cardinale D, Ky B, Nohria A, Baer L, et al. Cancer therapy–related cardiac dysfunction and heart failure. Circ Hear Fail. 2016;9:e002661.
Angelone T, Rocca C, Lionetti V, Penna C, Pagliaro P. Expanding the frontiers of guardian antioxidant selenoproteins in cardiovascular pathophysiology. Antioxid Redox Signal. 2024;40:369–432.
Omland T, Heck SL, Gulati G. The role of cardioprotection in cancer therapy cardiotoxicity. JACC CardioOncol. 2022;4:19–37.
Leyland-Jones B, Arnold A, Gelmon K, Verma S, Ayoub JP, Seidman A, et al. Pharmacologic insights into the future of trastuzumab. Ann Oncol. 2001;12:S43–7.
Quartino AL, Hillenbach C, Li J, Li H, Wada RD, Visich J, et al. Population pharmacokinetic and exposure–response analysis for trastuzumab administered using a subcutaneous “manual syringe” injection or intravenously in women with HER2-positive early breast cancer. Cancer Chemother Pharmacol. 2016;77:77–88.
Quartino AL, Li H, Kirschbrown WP, Mangat R, Wada DR, Garg A, et al. Population pharmacokinetic and covariate analyses of intravenous trastuzumab (Herceptin®), a HER2-targeted monoclonal antibody, in patients with a variety of solid tumors. Cancer Chemother Pharmacol. 2019;83:329–40.
Kirschbrown WP, Wang B, Nijem I, Ohtsu A, Hoff PM, Shah MA, et al. Pharmacokinetic and exposure–response analysis of pertuzumab in patients with HER2-positive metastatic gastric or gastroesophageal junction cancer. Cancer Chemother Pharmacol. 2019;84:539–50.
Treish I, Schwartz R, Lindley C. Pharmacology and therapeutic use of trastuzumab in breast cancer. Am J Health Syst Pharmacol. 2000;57:2063–76. 2077–9
Lin NU, Pegram M, Sahebjam S, Ibrahim N, Fung A, Cheng A, et al. Pertuzumab plus high-dose Trastuzumab in patients with progressive brain metastases and HER2-positive metastatic breast cancer: primary analysis of a phase II study. J Clin Oncol. 2021;39:2667–75.
De Keulenaer GW, Doggen K, Lemmens K. The vulnerability of the heart as a pluricellular paracrine organ. Circ Res. 2010;106:35–46.
Giri DK, Ali-Seyed M, Li L-Y, Lee D-F, Ling P, Bartholomeusz G, et al. Endosomal transport of ErbB-2: Mechanism for nuclear entry of the cell surface receptor. Mol Cell Biol. 2005;25:11005–18.
Li LY, Chen H, Hsieh YH, Wang YN, Chu HJ, Chen YH, et al. Nuclear ErbB2 enhances translation and cell growth by activating transcription of ribosomal RNA genes. Cancer Res. 2011;71:4269–79.
Wang SC, Lien HC, Xia W, Chen IF, Lo HW, Wang Z, et al. Binding at and transactivation of the COX-2 promoter by nuclear tyrosine kinase receptor ErbB-2. Cancer Cell. 2004;6:251–61.
Mohan N, Shen Y, Endo Y, ElZarrad MK, Wu WJ. Trastuzumab, but not Pertuzumab, dysregulates HER2 signaling to mediate inhibition of autophagy and increase in reactive oxygen species production in human cardiomyocytes. Mol Cancer Ther. 2016;15:1321–31.
Eaton H, Timm KN. Mechanisms of trastuzumab induced cardiotoxicity – is exercise a potential treatment? Cardiooncology. 2023;9:22.
Kabel AM, Elkhoely AA. Targeting proinflammatory cytokines, oxidative stress, TGF-β1 and STAT-3 by rosuvastatin and ubiquinone to ameliorate trastuzumab cardiotoxicity. Biomed Pharmacother. 2017;93:17–26.
Cuomo A, Rodolico A, Galdieri A, Russo M, Campi G, Franco R, et al. Heart failure and cancer: mechanisms of old and new cardiotoxic drugs in cancer patients. Card Fail Rev. 2019;5:112–8.
Swain SM, Shastry M, Hamilton E. Targeting HER2-positive breast cancer: advances and future directions. Nat Rev Drug Discov. 2023;22:101–26.
Blaschke F, Bruemmer D, Yin F, Takata Y, Wang W, Fishbein MC, et al. C-Reactive protein induces apoptosis in human coronary vascular smooth muscle cells. Circulation. 2004;110:579–87.
Tanigaki K, Sundgren N, Khera A, Vongpatanasin W, Mineo C, Shaul PW. Fcγ receptors and ligands and cardiovascular disease. Circ Res. 2015;116:368–84.
Acknowledgements
The authors acknowledge Dr. Francesca Giordano (Department of Pharmacy, Health and Nutritional Sciences, University of Calabria, 87036 Arcavacata di Rende, Cosenza, Italy) for her technical support in the flow cytometry analysis. This research was supported by “SI.F.I.PA.CRO.DE. – Sviluppo e industrializzazione farmaci innovativi per terapia molecolare personalizzata PA.CRO.DE” (PON ARS01_00568).
Author information
Authors and Affiliations
Contributions
ADB, NR, AM, VR, MCG, MLV, AC, RR, MC, and RS performed the experiments, contributed to prepare, collect, and analyze the data; ADB and CR wrote the first draft of the manuscript; MCC and CI contributed to supervision of the experiments, review and edit the manuscript. CR and TA conceived the project, analyzed data, supervisioned and validated the experiments, reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
De Bartolo, A., Romeo, N., Marrone, A. et al. A recombinant fragment antigen-binding (Fab) of trastuzumab displays low cytotoxic profile in adult human cardiomyocytes: first evidence and the key implication of FcγRIIA receptor. Acta Pharmacol Sin 46, 618–631 (2025). https://doi.org/10.1038/s41401-024-01397-3
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41401-024-01397-3