Abstract
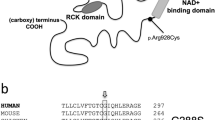
Patients suffering epilepsy caused by the gain-of-function mutants of the hKCNT1 potassium channels are drug refractory. In this study, we cloned a novel human KCNT1B channel isoform using the brain cDNA library and conducted patch-clamp and molecular docking analyses to characterize the pharmacological properties of the hKCNT1B channel using thirteen drugs. Among cinchona alkaloids, we found that hydroquinine exerted the strongest blocking effect on the hKCNT1B channel, especially the F313L mutant. In addition, we confirmed the antitussive drug tipepidine was also a potent inhibitor of the hKCNT1B channel. Subsequently, we proved that these two drugs produced an excellent therapeutic effect on the epileptic model of KCNT1 Y777H mutant male mice; thus, both could be ready-to-use anti-epileptic drugs. On the other hand, we demonstrated that the activation of the KCNT1 channel by loxapine and clozapine was through interacting with pore domain residues to reverse the run-down of the KCNT1 channel. Taken together, our results provide new insights into the mechanism of the modulators in regulating the KCNT1 channel activity as well as important candidates for clinical tests in the treatment of KCNT1 mutant-associated epilepsy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Yuan A, Santi CM, Wei A, Wang ZW, Pollak K, Nonet M, et al. The sodium-activated potassium channel is encoded by a member of the Slo gene family. Neuron. 2003;37:765–73.
Xu J, Lv YT, Zhao XY, Wang JJ, Shen ZS, Li J, et al. Identification of sodium- and chloride-sensitive sites in the Slack channel. J Neurosci. 2023;43:2665–81.
Hite RK, Yuan P, Li Z, Hsuing Y, Walz T, MacKinnon R. Cryo-electron microscopy structure of the Slo2.2 Na+-activated K+ channel. Nature. 2015;527:198–203.
Hite RK, MacKinnon R. Structural titration of Slo2.2, a Na+-dependent K+ channel. Cell. 2017;168:390–9.e11.
Martinez-Espinosa PL, Wu J, Yang C, Gonzalez-Perez V, Zhou H, Liang H, et al. Knockout of Slo2.2 enhances itch, abolishes KNa current, and increases action potential firing frequency in DRG neurons. Elife. 2015;4:e10013.1–27.
Joiner WJ, Tang MD, Wang LY, Dworetzky SI, Boissard CG, Gan L, et al. Formation of intermediate-conductance calcium-activated potassium channels by interaction of Slack and Slo subunits. Nat Neurosci. 1998;1:462–9.
Bhattacharjee A, Gan L, Kaczmarek LK. Localization of the Slack potassium channel in the rat central nervous system. J Comp Neurol. 2002;454:241–54.
Liu Y, Zhang FF, Song Y, Wang R, Zhang Q, Shen ZS, et al. The Slack channel deletion causes mechanical pain hypersensitivity in mice. Front Mol Neurosci. 2022;15:811441.
Shore AN, Colombo S, Tobin WF, Petri S, Cullen ER, Dominguez S, et al. Reduced GABAergic neuron excitability, altered synaptic connectivity, and seizures in a KCNT1 gain-of-function mouse model of childhood epilepsy. Cell Rep. 2020;33:108303.
Zhang Q, Gao SH, Shen ZS, Wang Y, Hu SW, Duan GB, et al. The Slack channel regulates anxiety-like behaviors via basolateral amygdala glutamatergic projections to ventral hippocampus. J Neurosci. 2022;42:3049–64.
Heron SE, Smith KR, Bahlo M, Nobili L, Kahana E, Licchetta L, et al. Missense mutations in the sodium-gated potassium channel gene KCNT1 cause severe autosomal dominant nocturnal frontal lobe epilepsy. Nat Genet. 2012;44:1188–90.
Kuchenbuch M, Barcia G, Chemaly N, Carme E, Roubertie A, Gibaud M, et al. KCNT1 epilepsy with migrating focal seizures shows a temporal sequence with poor outcome, high mortality and SUDEP. Brain. 2019;142:2996–3008.
Borlot F, Abushama A, Morrison-Levy N, Jain P, Puthenveettil Vinayan K, Abukhalid M, et al. KCNT1-related epilepsy: an international multicenter cohort of 27 pediatric cases. Epilepsia. 2020;61:679–92.
Hildebrand MS, Myers CT, Carvill GL, Regan BM, Damiano JA, Mullen SA, et al. A targeted resequencing gene panel for focal epilepsy. Neurology. 2016;86:1605–12.
Burgess R, Wang S, McTague A, Boysen KE, Yang X, Zeng Q, et al. The genetic landscape of epilepsy of infancy with migrating focal seizures. Ann Neurol. 2019;86:821–31.
Ohba C, Kato M, Takahashi N, Osaka H, Shiihara T, Tohyama J, et al. De novo KCNT1 mutations in early-onset epileptic encephalopathy. Epilepsia. 2015;56:e121–8.
Ishii A, Shioda M, Okumura A, Kidokoro H, Sakauchi M, Shimada S, et al. A recurrent KCNT1 mutation in two sporadic cases with malignant migrating partial seizures in infancy. Gene. 2013;531:467–71.
Gertler TS, Thompson CH, Vanoye CG, Millichap JJ, George AL Jr. Functional consequences of a KCNT1 variant associated with status dystonicus and early-onset infantile encephalopathy. Ann Clin Transl Neurol. 2019;6:1606–15.
Shimada S, Hirano Y, Ito S, Oguni H, Nagata S, Shimojima K, et al. A novel KCNT1 mutation in a Japanese patient with epilepsy of infancy with migrating focal seizures. Hum Genome Var. 2014;1:14027.
Rizzo F, Ambrosino P, Guacci A, Chetta M, Marchese G, Rocco T, et al. Characterization of two de novoKCNT1 mutations in children with malignant migrating partial seizures in infancy. Mol Cell Neurosci. 2016;72:54–63.
Chen Y, Bao XH, Zhang QP, Wang JP, Wen YX, Yu SJ, et al. [Genetic and clinical analysis of children with early-onset epilepsy encephalopathy caused by KCNT1 gene mutation]. Zhonghua Er Ke Za Zhi. 2018;56:824–8.
Arai-Ichinoi N, Uematsu M, Sato R, Suzuki T, Kudo H, Kikuchi A, et al. Genetic heterogeneity in 26 infants with a hypomyelinating leukodystrophy. Hum Genet. 2016;135:89–98.
Martin HC, Kim GE, Pagnamenta AT, Murakami Y, Carvill GL, Meyer E, et al. Clinical whole-genome sequencing in severe early-onset epilepsy reveals new genes and improves molecular diagnosis. Hum Mol Genet. 2014;23:3200–11.
Jia Y, Lin Y, Li J, Li M, Zhang Y, Hou Y, et al. Quinidine therapy for Lennox-Gastaut syndrome with KCNT1 mutation. A case report and literature review. Front Neurol. 2019;10:64.
Moller RS, Heron SE, Larsen LH, Lim CX, Ricos MG, Bayly MA, et al. Mutations in KCNT1 cause a spectrum of focal epilepsies. Epilepsia. 2015;56:e114–20.
Numis AL, Nair U, Datta AN, Sands TT, Oldham MS, Patel A, et al. Lack of response to quinidine in KCNT1-related neonatal epilepsy. Epilepsia. 2018;59:1889–98.
Kawasaki Y, Kuki I, Ehara E, Murakami Y, Okazaki S, Kawawaki H, et al. Three cases of KCNT1 mutations: malignant migrating partial seizures in infancy with massive systemic to pulmonary collateral arteries. J Pediatr. 2017;191:270–4.
Zhang Q, Liu Y, Xu J, Teng Y, Zhang Z. The functional properties, physiological roles, channelopathy and pharmacological characteristics of the Slack (KCNT1) channel. Adv Exp Med Biol. 2021;1349:387–400.
Tang QY, Zhang FF, Xu J, Wang R, Chen J, Logothetis DE, et al. Epilepsy-related Slack channel mutants lead to channel over-activity by two different mechanisms. Cell Rep. 2016;14:129–39.
Bearden D, Strong A, Ehnot J, DiGiovine M, Dlugos D, Goldberg EM. Targeted treatment of migrating partial seizures of infancy with quinidine. Ann Neurol. 2014;76:457–61.
Milligan CJ, Li M, Gazina EV, Heron SE, Nair U, Trager C, et al. KCNT1 gain of function in 2 epilepsy phenotypes is reversed by quinidine. Ann Neurol. 2014;75:581–90.
Fukuoka M, Kuki I, Kawawaki H, Okazaki S, Kim K, Hattori Y, et al. Quinidine therapy for West syndrome with KCNTI mutation: a case report. Brain Dev. 2017;39:80–3.
Dilena R, DiFrancesco JC, Soldovieri MV, Giacobbe A, Ambrosino P, Mosca I, et al. Early treatment with quinidine in 2 patients with epilepsy of infancy with migrating focal seizures (EIMFS) due to gain-of-function KCNT1 mutations: functional studies, clinical responses, and critical issues for personalized therapy. Neurotherapeutics. 2018;15:1112–26.
Mikati MA, Jiang YH, Carboni M, Shashi V, Petrovski S, Spillmann R, et al. Quinidine in the treatment of KCNT1-positive epilepsies. Ann Neurol. 2015;78:995–9.
Mullen SA, Carney PW, Roten A, Ching M, Lightfoot PA, Churilov L, et al. Precision therapy for epilepsy due to KCNT1 mutations: a randomized trial of oral quinidine. Neurology. 2018;90:e67–72.
Fitzgerald MP, Fiannacca M, Smith DM, Gertler TS, Gunning B, Syrbe S, et al. Treatment responsiveness in KCNT1-related epilepsy. Neurotherapeutics. 2019;16:848–57.
Abdelnour E, Gallentine W, McDonald M, Sachdev M, Jiang YH, Mikati MA. Does age affect response to quinidine in patients with KCNT1 mutations? Report of three new cases and review of the literature. Seizure. 2018;55:1–3.
Yoshitomi S, Takahashi Y, Yamaguchi T, Oboshi T, Horino A, Ikeda H, et al. Quinidine therapy and therapeutic drug monitoring in four patients with KCNT1 mutations. Epileptic Disord. 2019;21:48–54.
Madaan P, Jauhari P, Gupta A, Chakrabarty B, Gulati S. A quinidine non responsive novel KCNT1 mutation in an Indian infant with epilepsy of infancy with migrating focal seizures. Brain Dev. 2018;40:229–32.
McTague A, Nair U, Malhotra S, Meyer E, Trump N, Gazina EV, et al. Clinical and molecular characterization of KCNT1-related severe early-onset epilepsy. Neurology. 2018;90:e55–66.
Xu D, Chen S, Yang J, Wang X, Fang Z, Li M. Precision therapy with quinidine of KCNT1-related epileptic disorders: a systematic review. Br J Clin Pharmacol. 2022;88:5096–112.
Mori K, Saito T, Masuda Y, Nakaya H. Effects of class III antiarrhythmic drugs on the Na+-activated K+ channels in guinea-pig ventricular cells. Br J Pharmacol. 1996;119:133–41.
Mori K, Kobayashi S, Saito T, Masuda Y, Nakaya H. Inhibitory effects of class I and IV antiarrhythmic drugs on the Na+-activated K+ channel current in guinea pig ventricular cells. Naunyn Schmiedebergs Arch Pharmacol. 1998;358:641–8.
Yang B, Gribkoff VK, Pan J, Damagnez V, Dworetzky SI, Boissard CG, et al. Pharmacological activation and inhibition of Slack (Slo2.2) channels. Neuropharmacology. 2006;51:896–906.
Cole BA, Johnson RM, Dejakaisaya H, Pilati N, Fishwick CWG, Muench SP, et al. Structure-based identification and characterization of inhibitors of the epilepsy-associated KNa1.1 (KCNT1) potassium channel. iScience. 2020;23:101100.
Spitznagel BD, Mishra NM, Qunies AM, Prael FJ, 3rd, Du Y, Kozek KA, et al. VU0606170, a selective Slack channels inhibitor, decreases calcium oscillations in cultured cortical neurons. ACS Chem Neurosci. 2020;11:3658–71.
Griffin AM, Kahlig KM, Hatch RJ, Hughes ZA, Chapman ML, Antonio B, et al. Discovery of the first orally available, selective K(Na)1.1 inhibitor: in vitro and in vivo activity of an oxadiazole series. ACS Med Chem Lett. 2021;12:593–602.
Biton B, Sethuramanujam S, Picchione KE, Bhattacharjee A, Khessibi N, Chesney F, et al. The antipsychotic drug loxapine is an opener of the sodium-activated potassium channel slack (Slo2.2). J Pharmacol Exp Ther. 2012;340:706–15.
Evely KM, Pryce KD, Bhattacharjee A. The Phe932Ile mutation in KCNT1 channels associated with severe epilepsy, delayed myelination and leukoencephalopathy produces a loss-of-function channel phenotype. Neuroscience. 2017;351:65–70.
Wang GM, Zhong ZG, Du XR, Zhang FF, Guo Q, Liu Y, et al. Cloning and characterization of the rat Slo3 (K(Ca) 5.1) channel: from biophysics to pharmacology. Br J Pharmacol. 2020;177:3552–67.
Tang QY, Kolanos R, De Felice LJ, Glennon RA. Structural analysis of dopamine- and amphetamine-induced depolarization currents in the human dopamine transporter. ACS Chem Neurosci. 2015;6:551–8.
Xie C, Liu HW, Pan N, Ding JP, Yao J. The residue I257 at S4-S5 linker in KCNQ1 determines KCNQ1/KCNE1 channel sensitivity to 1-alkanols. Acta Pharmacol Sin. 2016;37:124–33.
Bitencourt-Ferreira G, Pintro VO, de Azevedo WF Jr. Docking with AutoDock4. Methods Mol Biol. 2019;2053:125–48.
Chou TC. Theoretical basis, experimental design, and computerized simulation of synergism and antagonism in drug combination studies. Pharmacol Rev. 2006;58:621–81.
Luttjohann A, Fabene PF, van Luijtelaar G. A revised Racine’s scale for PTZ-induced seizures in rats. Physiol Behav. 2009;98:579–86.
Liu J, Liu X, Zhou WY, Gan J, Wang J, Zhang Q, et al. The activation of GABAergic neurons in the hypothalamic tuberomammillary nucleus attenuates sevoflurane and propofol-induced anesthesia in mice. Front Pharmacol. 2023;14:1153735.
Yeste M, Llavanera M, Pérez G, Scornik F, Puig-Parri J, Brugada R, et al. Elucidating the role of K+ channels during in vitro capacitation of boar spermatozoa: do SLO1 channels play a crucial role? Int J Mol Sci. 2019;20:1–21.
Zhou Y, Tang QY, Xia XM, Lingle CJ. Glycine311, a determinant of paxilline block in BK channels: a novel bend in the BK S6 helix. J Gen Physiol. 2010;135:481–94.
Romoli M, Mazzocchetti P, D’Alonzo R, Siliquini S, Rinaldi VE, Verrotti A, et al. Valproic acid and epilepsy: from molecular mechanisms to clinical evidences. Curr Neuropharmacol. 2019;17:926–46.
Takase C, Shirai K, Matsumura Y, Watanabe T, Watanabe A, Hirasawa-Inoue A, et al. KCNT1-positive epilepsy of infancy with migrating focal seizures successfully treated with nonnarcotic antitussive drugs after treatment failure with quinidine: a case report. Brain Dev. 2020;42:607–11.
Schmiedl S, Peters D, Schmalz O, Mielke A, Rossmanith T, Diop S, et al. Loxapine for treatment of patients with refractory, chemotherapy-induced neuropathic pain: a prematurely terminated pilot study showing efficacy but limited tolerability. Front Pharmacol. 2019;10:838.
Tang QY, Zhang Z, Xia XM, Lingle CJ. Block of mouse Slo1 and Slo3 K+ channels by CTX, IbTX, TEA, 4-AP and quinidine. Channels. 2010;4:22–41.
Kirsch GE, Shieh CC, Drewe JA, Vener DF, Brown AM. Segmental exchanges define 4-aminopyridine binding and the inner mouth of K+ pores. Neuron. 1993;11:503–12.
Shieh CC, Kirsch GE. Mutational analysis of ion conduction and drug binding sites in the inner mouth of voltage-gated K+ channels. Biophys J. 1994;67:2316–25.
Choquet D, Korn H. Mechanism of 4-aminopyridine action on voltage-gated potassium channels in lymphocytes. J Gen Physiol. 1992;99:217–40.
Armstrong CM, Hollingworth S. Na+ and K+ channels: history and structure. Biophys J. 2021;120:756–63.
Lenaeus MJ, Vamvouka M, Focia PJ, Gross A. Structural basis of TEA blockade in a model potassium channel. Nat Struct Mol Biol. 2005;12:454–9.
Yellen G, Jurman ME, Abramson T, MacKinnon R. Mutations affecting internal TEA blockade identify the probable pore-forming region of a K+ channel. Science. 1991;251:939–42.
Mikov M, Kevresan S, Kuhajda K, Jakovljevic V, Vasovic V. 3Alpha,7alpha-dihydroxy-12-oxo-5beta-cholanate as blood-brain barrier permeator. Pol J Pharmacol. 2004;56:367–71.
Liu X, Van Natta K, Yeo H, Vilenski O, Weller PE, Worboys PD, et al. Unbound drug concentration in brain homogenate and cerebral spinal fluid at steady state as a surrogate for unbound concentration in brain interstitial fluid. Drug Metab Dispos. 2009;37:787–93.
Costa-Jussa FR, Jacobs JM. The pathology of amiodarone neurotoxicity. I. Experimental studies with reference to changes in other tissues. Brain. 1985;108:735–52.
Brien JF, Jimmo S, Brennan FJ, Ford SE, Armstrong PW. Distribution of amiodarone and its metabolite, desethylamiodarone, in human tissues. Can J Physiol Pharmacol. 1987;65:360–4.
Brien JF, Jimmo S, Brennan FJ, Armstrong PW, Abdollah H. Disposition of amiodarone and its proximate metabolite, desethylamiodarone, in the dog for oral administration of single-dose and short-term drug regimens. Drug Metab Dispos. 1990;18:846–51.
Singh BN. Bepridil therapy: guidelines for patient selection and monitoring of therapy. Am J Cardiol. 1992;69:79D–85D.
Wei YL, Lei YQ, Ye ZJ, Zhuang XD, Zhu LP, Wang XR, et al. Effects of bepridil on early cardiac development of zebrafish. Cell Tissue Res. 2023;391:375–91.
Kojima A, Ito Y, Ding WG, Kitagawa H, Matsuura H. Interaction of propofol with voltage-gated human Kv1.5 channel through specific amino acids within the pore region. Eur J Pharmacol. 2015;764:622–32.
Yang L, Liu H, Sun HY, Li GR. Intravenous anesthetic propofol inhibits multiple human cardiac potassium channels. Anesthesiology. 2015;122:571–84.
Zanatta G, Sula A, Miles AJ, Ng LCT, Torella R, Pryde DC, et al. Valproic acid interactions with the NavMs voltage-gated sodium channel. Proc Natl Acad Sci USA. 2019;116:26549–54.
Miki R, Honda I, Hamasaki R, Kawahara R, Soeda F, Shirasaki T, et al. Effects of tipepidine on MK-801-induced cognitive impairment in mice. Brain Res. 2019;1710:230–6.
Aylward M, Maddock J, Davies DE, Protheroe DA, Leideman T. Dextromethorphan and codeine: comparison of plasma kinetics and antitussive effects. Eur J Respir Dis. 1984;65:283–91.
Nanou E, Kyriakatos A, Bhattacharjee A, Kaczmarek LK, Paratcha G, El Manira A. Na+-mediated coupling between AMPA receptors and KNa channels shapes synaptic transmission. Proc Natl Acad Sci USA. 2008;105:20941–6.
Nguyen L, Matsumoto RR. Involvement of AMPA receptors in the antidepressant-like effects of dextromethorphan in mice. Behav Brain Res. 2015;295:26–34.
Egan TM, Dagan D, Kupper J, Levitan IB. Properties and rundown of sodium-activated potassium channels in rat olfactory bulb neurons. J Neurosci. 1992;12:1964–76.
Acknowledgements
This work was supported by a Natural Science Foundation of China (NSFC) grant to ZZ (81471314 and 81671090), Natural Science Foundation of Jiangsu Province to ZZ (SBK201502515), Xuzhou Science and Technology Program (KC19036) to ZZ and (KC16H0230) to QYT, an NSFC grant to QYT (82371233). The Important Project of Natural Science in Colleges and Universities in Jiangsu Province to ZZ (14KJA320002), Jiangsu specially appointed professor to ZZ and QYT, We also appreciate the grant support from the Priority Academic Program Development of Jiangsu Higher Education Institutions and the Jiangsu Provincial Special Program of Medical Science (BL2014029). Jiangsu Province College Students’ Innovative Entrepreneurial Training Plan Program to YMW (202110313072). The general project of the developing grant for the Affiliated Hospital of Xuzhou Medical University to MJK (XYFM202330).
Author information
Authors and Affiliations
Contributions
QG, JG, EZW, and YMW performed research and analyzed the data. FFZ cloned the hKCNT1 channel. YX tested the electrophysiological property of the hKCNT1 channel. JX and MC generated the modeling structure. MJK and MXJ provided useful suggestions and supervised surgery. QYT and ZZ designed the experiment and wrote the paper. All authors have approved the final version of this manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guo, Q., Gan, J., Wang, Ez. et al. Electrophysiological characterization of human KCNT1 channel modulators and the therapeutic potential of hydroquinine and tipepidine in KCNT1 mutation-associated epilepsy mouse model. Acta Pharmacol Sin 46, 1190–1204 (2025). https://doi.org/10.1038/s41401-024-01457-8
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41401-024-01457-8