Abstract
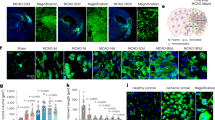
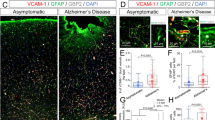
The acute phase of ischemic stroke is marked by a surge in matrix metalloproteinase-9 (MMP-9) activity. While integral to natural repair processes, MMP-9 exacerbates injury by breaking down the blood-brain barrier (BBB) and promoting edema and inflammation. MMP-9 is predominantly secreted by inflammatory cells such as neutrophils, macrophages and microglia soon after stroke onset. In this study we investigated the effects of MMP-9 inhibition via SB-3CT on astrocytic lipid metabolism, and its potential to enhance neuronal survival and recovery following ischemic stroke. Mice were subjected to transient middle cerebral artery occlusion (tMCAO) for 60 min, mice then were injected with SB-3CT (25 mg/kg, i.v.). On D3 post tMCAO, neurological outcomes were assessed, and whole brains were collected for analysis. Lipidomic analysis of brain tissue showed that SB-3CT treatment significantly restrained astrocytic cholesterol metabolism by modulating the sphingolipid and glycerophospholipid pathways. Specifically, SB-3CT reduced ceramide accumulation and promoted an increase in neuroprotective hexosylceramides, leading to enhanced neuronal survival and synaptic integrity. In addition, SB-3CT treatment reduced astrocytic and microglial reactivity, thereby mitigating neuroinflammation. In order to optimize the timing and dosage of MMP-9 inhibition to maximize the therapeutic efficacy, tMCAO mice were given three injections of SB-3CT on D0, D2 and D4 within 7 days after modeling. We found that prolonged MMP-9 inhibition alleviated astrogliosis, concurrently impaired neurological recovery and inhibited angiogenesis. These results demonstrate the critical role of lipid metabolism in MMP-9-mediated brain injury and the potential of SB-3CT as a therapeutic strategy for ischemic stroke by targeting astrocytic lipid metabolism.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Collaborators GBDS. Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:439–58.
Phipps MS, Cronin CA. Management of acute ischemic stroke. BMJ. 2020;368:l6983.
Gu Z, Cui J, Brown S, Fridman R, Mobashery S, Strongin AY, et al. A highly specific inhibitor of matrix metalloproteinase-9 rescues laminin from proteolysis and neurons from apoptosis in transient focal cerebral ischemia. J Neurosci. 2005;25:6401–8.
Cui J, Chen S, Zhang C, Meng F, Wu W, Hu R, et al. Inhibition of MMP-9 by a selective gelatinase inhibitor protects neurovasculature from embolic focal cerebral ischemia. Mol Neurodegener. 2012;7:21.
Sofroniew MV. Molecular dissection of reactive astrogliosis and glial scar formation. Trends Neurosci. 2009;32:638–47.
Asahi M, Asahi K, Jung JC, del Zoppo GJ, Fini ME, Lo EH. Role for matrix metalloproteinase 9 after focal cerebral ischemia: effects of gene knockout and enzyme inhibition with BB-94. J Cereb Blood Flow Metab. 2000;20:1681–9.
Mi Y, Qi G, Vitali F, Shang Y, Raikes AC, Wang T, et al. Loss of fatty acid degradation by astrocytic mitochondria triggers neuroinflammation and neurodegeneration. Nat Metab. 2023;5:445–65.
Chen ZP, Wang S, Zhao X, Fang W, Wang Z, Ye H, et al. Lipid-accumulated reactive astrocytes promote disease progression in epilepsy. Nat Neurosci. 2023;26:542–54.
Ioannou MS, Jackson J, Sheu SH, Chang CL, Weigel AV, Liu H, et al. Neuron-astrocyte metabolic coupling protects against activity-induced fatty acid toxicity. Cell. 2019;177:1522–35.e14.
Morant-Ferrando B, Jimenez-Blasco D, Alonso-Batan P, Agulla J, Lapresa R, Garcia-Rodriguez D, et al. Fatty acid oxidation organizes mitochondrial supercomplexes to sustain astrocytic ROS and cognition. Nat Metab. 2023;5:1290–302.
Li X, Zhang J, Li D, He C, He K, Xue T, et al. Astrocytic ApoE reprograms neuronal cholesterol metabolism and histone-acetylation-mediated memory. Neuron. 2021;109:957–70.e8.
Lee H, Cho S, Kim MJ, Park YJ, Cho E, Jo YS, et al. ApoE4-dependent lysosomal cholesterol accumulation impairs mitochondrial homeostasis and oxidative phosphorylation in human astrocytes. Cell Rep. 2023;42:113183.
Tcw J, Qian L, Pipalia NH, Chao MJ, Liang SA, Shi Y, et al. Cholesterol and matrisome pathways dysregulated in astrocytes and microglia. Cell. 2022;185:2213–33.e25.
Hernandez-Anzaldo S, Brglez V, Hemmeryckx B, Leung D, Filep JG, Vance JE, et al. Novel role for matrix metalloproteinase 9 in modulation of cholesterol metabolism. J Am Heart Assoc. 2016;5:e004228.
Macrae IM. Preclinical stroke research-advantages and disadvantages of the most common rodent models of focal ischaemia. Br J Pharmacol. 2011;164:1062–78.
Ji Y, Gao Q, Ma Y, Wang F, Tan X, Song D, et al. An MMP-9 exclusive neutralizing antibody attenuates blood-brain barrier breakdown in mice with stroke and reduces stroke patient-derived MMP-9 activity. Pharm Res. 2023;190:106720.
Lopez T, Mustafa Z, Chen C, Lee KB, Ramirez A, Benitez C, et al. Functional selection of protease inhibitory antibodies. Proc Natl Acad Sci USA. 2019;116:16314–9.
Li Y, Chopp M, Chen J, Wang L, Gautam SC, Xu YX, et al. Intrastriatal transplantation of bone marrow nonhematopoietic cells improves functional recovery after stroke in adult mice. J Cereb Blood Flow Metab. 2000;20:1311–9.
Takao K, Kobayashi K, Hagihara H, Ohira K, Shoji H, Hattori S, et al. Deficiency of schnurri-2, an MHC enhancer binding protein, induces mild chronic inflammation in the brain and confers molecular, neuronal, and behavioral phenotypes related to schizophrenia. Neuropsychopharmacology. 2013;38:1409–25.
Dubal DB, Kashon ML, Pettigrew LC, Ren JM, Finklestein SP, Rau SW, et al. Estradiol protects against ischemic injury. J Cereb Blood Flow Metab. 1998;18:1253–8.
Carswell HV, Dominiczak AF, Macrae IM. Estrogen status affects sensitivity to focal cerebral ischemia in stroke-prone spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol. 2000;278:H290–4.
Ji YB, Wu YM, Ji Z, Song W, Xu SY, Wang Y, et al. Interrupted intracarotid artery cold saline infusion as an alternative method for neuroprotection after ischemic stroke. Neurosurgical Focus 2012; 33:E10.
Ji YB, Gao Q, Tan XX, Huang XW, Ma YZ, Fang C, et al. Lithium alleviates blood-brain barrier breakdown after cerebral ischemia and reperfusion by upregulating endothelial Wnt/beta-catenin signaling in mice. Neuropharmacology. 2021;186:108474.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–8.
Bouscary A, Quessada C, Rene F, Spedding M, Turner BJ, Henriques A, et al. Sphingolipids metabolism alteration in the central nervous system: Amyotrophic lateral sclerosis (ALS) and other neurodegenerative diseases. Semin Cell Dev Biol. 2021;112:82–91.
Limaye V, Li X, Hahn C, Xia P, Berndt MC, Vadas MA, et al. Sphingosine kinase-1 enhances endothelial cell survival through a PECAM-1-dependent activation of PI-3K/Akt and regulation of Bcl-2 family members. Blood. 2005;105:3169–77.
Mizugishi K, Yamashita T, Olivera A, Miller GF, Spiegel S, Proia RL. Essential role for sphingosine kinases in neural and vascular development. Mol Cell Biol. 2005;25:11113–21.
Kloska A, Malinowska M, Gabig-Ciminska M, Jakobkiewicz-Banecka J. Lipids and lipid mediators associated with the risk and pathology of ischemic stroke. Int J Mol Sci. 2020;21:3618.
Purroy F, Ois A, Jove M, Arque G, Sol J, Mauri-Capdevila G, et al. Lipidomic signature of stroke recurrence after transient ischemic attack. Sci Rep. 2023;13:13706.
Huang XX, Li L, Jiang RH, Yu JB, Sun YQ, Shan J, et al. Lipidomic analysis identifies long-chain acylcarnitine as a target for ischemic stroke. J Adv Res. 2024;61:133–49.
ElAli A, Doeppner TR, Zechariah A, Hermann DM. Increased blood-brain barrier permeability and brain edema after focal cerebral ischemia induced by hyperlipidemia: role of lipid peroxidation and calpain-1/2, matrix metalloproteinase-2/9, and RhoA overactivation. Stroke. 2011;42:3238–44.
Sofroniew MV, Vinters HV. Astrocytes: biology and pathology. Acta Neuropathol. 2010;119:7–35.
Kumar A, Fontana IC, Nordberg A. Reactive astrogliosis: A friend or foe in the pathogenesis of Alzheimer’s disease. J Neurochem. 2023;164:309–24.
Escartin C, Galea E, Lakatos A, O’Callaghan JP, Petzold GC, Serrano-Pozo A, et al. Reactive astrocyte nomenclature, definitions, and future directions. Nat Neurosci. 2021;24:312–25.
Hsu JY, Bourguignon LY, Adams CM, Peyrollier K, Zhang H, Fandel T, et al. Matrix metalloproteinase-9 facilitates glial scar formation in the injured spinal cord. J Neurosci. 2008;28:13467–77.
Fecher C, Trovo L, Muller SA, Snaidero N, Wettmarshausen J, Heink S, et al. Cell-type-specific profiling of brain mitochondria reveals functional and molecular diversity. Nat Neurosci. 2019;22:1731–42.
Alaamery M, Albesher N, Aljawini N, Alsuwailm M, Massadeh S, Wheeler MA, et al. Role of sphingolipid metabolism in neurodegeneration. J Neurochem. 2021;158:25–35.
Ayub M, Jin HK, Bae JS. Novelty of sphingolipids in the central nervous system physiology and disease: focusing on the sphingolipid hypothesis of neuroinflammation and neurodegeneration. Int J Mol Sci. 2021;22:7353.
Dusaban SS, Chun J, Rosen H, Purcell NH, Brown JH. Sphingosine 1-phosphate receptor 3 and RhoA signaling mediate inflammatory gene expression in astrocytes. J Neuroinflammation. 2017;14:111.
Gupta P, Taiyab A, Hussain A, Alajmi MF, Islam A, Hassan MI. Targeting the sphingosine kinase/sphingosine-1-phosphate signaling axis in drug discovery for cancer therapy. Cancers. 2021;13:1898.
Candalija A, Cubi R, Ortega A, Aguilera J, Gil C. Trk receptors need neutral sphingomyelinase activity to promote cell viability. FEBS Lett. 2014;588:167–74.
Rosenberg GA, Estrada EY, Dencoff JE. Matrix metalloproteinases and TIMPs are associated with blood-brain barrier opening after reperfusion in rat brain. Stroke. 1998;29:2189–95.
Barr TL, Latour LL, Lee KY, Schaewe TJ, Luby M, Chang GS, et al. Blood-brain barrier disruption in humans is independently associated with increased matrix metalloproteinase-9. Stroke. 2010;41:e123–8.
Zhao BQ, Wang S, Kim HY, Storrie H, Rosen BR, Mooney DJ, et al. Role of matrix metalloproteinases in delayed cortical responses after stroke. Nat Med. 2006;12:441–5.
del Zoppo GJ, Frankowski H, Gu YH, Osada T, Kanazawa M, Milner R, et al. Microglial cell activation is a source of metalloproteinase generation during hemorrhagic transformation. J Cereb Blood Flow Metab. 2012;32:919–32.
Lee CZ, Yao JS, Huang Y, Zhai W, Liu W, Guglielmo BJ, et al. Dose-response effect of tetracyclines on cerebral matrix metalloproteinase-9 after vascular endothelial growth factor hyperstimulation. J Cereb Blood Flow Metab. 2006;26:1157–64.
Rosell A, Ortega-Aznar A, Alvarez-Sabin J, Fernandez-Cadenas I, Ribo M, Molina CA, et al. Increased brain expression of matrix metalloproteinase-9 after ischemic and hemorrhagic human stroke. Stroke. 2006;37:1399–406.
Montaner J, Molina CA, Monasterio J, Abilleira S, Arenillas JF, Ribo M, et al. Matrix metalloproteinase-9 pretreatment level predicts intracranial hemorrhagic complications after thrombolysis in human stroke. Circulation. 2003;107:598–603.
Acknowledgements
We would like to express our gratitude to Climb Technology Co., Ltd and Dr. Min Yao for their assistance with lipidomics analysis in our study.
Funding
This work was supported by the National Natural Science Foundation of China (31900704 to CF, 82273923 to YZM), Shandong Provincial Key Innovation Program (2019JZZY020909 to LDD) Guangdong Province Basic and Applied Basic Research Grant (2023A1515010467 to CF), Shenzhen Science and Technology Program (JCYJ20220531100203008 to YZM, JCYJ20230807140721043 to CF). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
YZM: Conceived and designed the research; supervised the project; contributed to data analysis and interpretation; wrote the manuscript. JYH: Contributed to experimental design; provided new reagents and resources; supervised lipidomic analysis. LDD: Performed animal surgeries and behavioral assessments; conducted immunofluorescence staining experiments; contributed to data collection. CF: Contributed to the design of lipidomic experiments; analyzed lipidomic data. ZYF: Assisted with experimental procedures and data collection; contributed to manuscript revision. YQW: Assisted with statistical analysis and interpretation of neurological recovery data. OFA: Conducted tissue collection and Western blot analysis; contributed to data interpretation. ZLG: Reviewed and commented on the manuscript; contributed to manuscript editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The experimental procedures performed on animals in this study were strictly in accordance with the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1996), and approved by the Institutional Animal Care and Use Committee (IACUC) of Shenzhen Institute of Advanced Technology, Chinese Academy of Sciences. All efforts were made to minimize animal suffering and to reduce the number of animals used.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Du, Ld., Fang, C., Wang, Yq. et al. MMP-9 inhibitor SB-3CT improves neurological outcomes in ischemic stroke mice by modulation of astrocytic lipid metabolism. Acta Pharmacol Sin 46, 2120–2135 (2025). https://doi.org/10.1038/s41401-025-01505-x
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41401-025-01505-x