Abstract
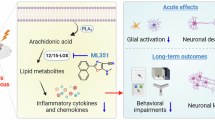
Pharmacoresistance remains intractable in epilepsy, necessitating in-depth mechanism investigations. Cumulative data have pointed to active neuroinflammation in pharmacoresistant epilepsy, but the process between neuroinflammation and pharmacoresistance remains unknown. In this study we investigated how severe neuroinflammation altered anti-seizure drugs (ASMs) pharmacology. Hippocampal kindling or kainic acid-induced temporal lobe epilepsy (TLE) models were established in mice that had received intra-hippocampal LPS injection. Acute hippocampal slices were prepared; current-clamp recording was made in hippocampal pyramidal neurons to assess the impact of ASMs on neuronal excitability and sodium channels. We showed that intra-hippocampal LPS injection resulted in higher inflammatory cytokine levels in the hippocampus. LPS induced-neuroinflammation significantly decreased the antiseizure efficacy of phenytoin (PHT), carbamazepine (CBZ) and rufinamide (RUF), all the ASMs tested were unable to alleviate the seizure severities. We observed the “off-target” phenomena of ASMs, i.e. ASMs’ loss of ability to suppress the firing of action potentials and the amplitudes of sodium currents in hippocampal pyramidal neurons from LPS-treated mice. We demonstrated that LPS induced-neuroinflammation promoted the degradation of spermine, an essential polyamine linked with ASM performance on sodium channels, through upregulating the catabolic enzyme spermidine/spermine N(1)-acetyltransferase (SSAT). Intra-hippocampal injection of SSAT agonist DENSPM mimicked LPS-induced “off-target” phenomena of ASMs, whereas injection of SSAT antagonist diminazene aceturate into hippocampus reversed the “off-target” phenomenon of ASMs in LPS-treated mice. Finally, intrahippocampal injection of spermine restored the efficacy of ASMs on action potential firings and sodium currents, resulting in the reversal of pharmacoresistance in LPS-treated TLE models. These results provide new evidence that neuroinflammation causes pharmacoresistance in TLE via promoting spermine degradation, and highlight spermine supplementation as a promising therapy for pharmacoresistant TLE.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Janmohamed M, Brodie MJ, Kwan P. Pharmacoresistance - epidemiology, mechanisms, and impact on epilepsy treatment. Neuropharmacology. 2020;168:107790.
Xu C, Gong Y, Wang Y, Chen Z. New advances in pharmacoresistant epilepsy towards precise management-from prognosis to treatments. Pharmacol Ther. 2022;233:108026.
Kalilani L, Sun X, Pelgrims B, Noack-Rink M, Villanueva V. The epidemiology of drug-resistant epilepsy: a systematic review and meta-analysis. Epilepsia. 2018;59:2179–93.
Loscher W, Potschka H, Sisodiya SM, Vezzani A. Drug resistance in epilepsy: clinical impact, potential mechanisms, and new innovative treatment options. Pharmacol Rev. 2020;72:606–38.
Bhalla D, Godet B, Druet-Cabanac M, Preux PM. Etiologies of epilepsy: a comprehensive review. Expert Rev Neurotherapeutics. 2011;11:861–76.
Ravizza T, Scheper M, Di Sapia R, Gorter J, Aronica E, Vezzani A. mTOR and neuroinflammation in epilepsy: implications for disease progression and treatment. Nat Rev Neurosci. 2024;25:334–50.
Singhi P. Infectious causes of seizures and epilepsy in the developing world. Dev Med child Neurol. 2011;53:600–9.
Vezzani A, Balosso S, Ravizza T. Neuroinflammatory pathways as treatment targets and biomarkers in epilepsy. Nat Rev Neurol. 2019;15:459–72.
Rana A, Musto AE. The role of inflammation in the development of epilepsy. J Neuroinflammation. 2018;15:144.
Tan CC, Zhang JG, Tan MS, Chen H, Meng DW, Jiang T, et al. NLRP1 inflammasome is activated in patients with medial temporal lobe epilepsy and contributes to neuronal pyroptosis in amygdala kindling-induced rat model. J Neuroinflammation. 2015;12:18.
Roseti C, van Vliet EA, Cifelli P, Ruffolo G, Baayen JC, Di Castro MA, et al. GABAA currents are decreased by IL-1beta in epileptogenic tissue of patients with temporal lobe epilepsy: implications for ictogenesis. Neurobiol Dis. 2015;82:311–20.
Husari KS, Dubey D. Autoimmune epilepsy. Neurotherapeutics. 2019;16:685–702.
Royeck M, Kelly T, Opitz T, Otte DM, Rennhack A, Woitecki A, et al. Downregulation of spermine augments dendritic persistent sodium currents and synaptic integration after status epilepticus. J Neurosci. 2015;35:15240–53.
Fu LY, Cummins TR, Moczydlowski EG. Sensitivity of cloned muscle, heart and neuronal voltage-gated sodium channels to block by polyamines A possible basis for modulation of excitability in vivo. Channels. 2012;6:41–9.
Fleidervish IA, Libman L, Katz E, Gutnick MJ. Endogenous polyamines regulate cortical neuronal excitability by blocking voltage-gated Na channels. Proc Natl Acad Sci USA. 2008;105:18994–9.
Beckonert NM, Opitz T, Pitsch J, Soares da Silva P, Beck H. Polyamine modulation of anticonvulsant drug response: a potential mechanism contributing to pharmacoresistance in chronic epilepsy. J Neurosci. 2018;38:5596–605.
Jiang J, Wang W, Sun F, Zhang Y, Liu Q, Yang D. Bacterial infection reinforces host metabolic flux from arginine to spermine for NLRP3 inflammasome evasion. Cell Rep. 2021;34:108832.
Herber DL, Maloney JL, Roth LM, Freeman MJ, Morgan D, Gordon MN. Diverse microglial responses after intrahippocampal administration of lipopolysaccharide. Glia. 2006;53:382–91.
Zhu F, Zhang L, Ding YQ, Zhao J, Zheng Y. Neonatal intrahippocampal injection of lipopolysaccharide induces deficits in social behavior and prepulse inhibition and microglial activation in rats: Implication for a new schizophrenia animal model. Brain Behav Immun. 2014;38:166–74.
Tret’yakova LV, Kvichansky AA, Barkovskaya ES, Manolova AO, Bolshakov AP, Gulyaeva NV. Ambiguous contribution of glucocorticosteroids to acute neuroinflammation in the hippocampus of rat. Int J Mol Sci. 2023;24:11147.
Shen Y, Gong Y, Da X, Gao S, Zhang S, Sun M, et al. Low-frequency stimulation at the subiculum prevents extensive secondary epileptogenesis in temporal lobe epilepsy. Neurosci Bull. 2024;40:564–576.
Paxinos G, Franklin KBJ. The mouse brain in stereotaxic coordinates, 2nd ed. London: Academic; 2001. pp. 264.
Racine RJ. Modification of seizure activity by electrical stimulation. II. Motor seizure. Electroencephalogr Clin Neurophysiol. 1972;32:281–94.
Ruan Y, Xu C, Lan J, Nao J, Zhang S, Fan F, et al. Low-frequency stimulation at the subiculum is anti-convulsant and anti-drug-resistant in a mouse model of lamotrigine-resistant temporal lobe epilepsy. Neurosci Bull. 2020;36:654–8.
Tian Y, Wang S, Wang B, Zhang J, Jiang R, Zhang W. Overexpression of SSAT by DENSPM treatment induces cell detachment and apoptosis in glioblastoma. Oncol Rep. 2012;27:1227–32.
Neidhart M, Karouzakis E, Jungel A, Gay RE, Gay S. Inhibition of spermidine/spermine N1-acetyltransferase activity: a new therapeutic concept in rheumatoid arthritis. Arthritis Rheumatol. 2014;66:1723–33.
Xu C, Zhang S, Gong Y, Nao J, Shen Y, Tan B, et al. Subicular caspase-1 contributes to pharmacoresistance in temporal lobe epilepsy. Ann Neurol. 2021;90:377–90.
Xu C, Wang Y, Zhang S, Nao J, Liu Y, Wang Y, et al. Subicular pyramidal neurons gate drug resistance in temporal lobe epilepsy. Ann Neurol. 2019;86:626–40.
Wu D, Feng B, Dai Y, Wu X, Chen B, Xu C, et al. Intergenerational transmission of enhanced seizure susceptibility after febrile seizures. EBioMedicine. 2017;17:206–15.
Mantegazza M, Curia G, Biagini G, Ragsdale DS, Avoli M. Voltage-gated sodium channels as therapeutic targets in epilepsy and other neurological disorders. Lancet Neurol. 2010;9:413–24.
Chou MY, Lee CY, Liou HH, Pan CY. Phenytoin attenuates the hyper-exciting neurotransmission in cultured embryonic cortical neurons. Neuropharmacology. 2014;83:54–61.
Molnar P, Erdo SL. Vinpocetine is as potent as phenytoin to block voltage-gated Na+ channels in rat cortical neurons. Eur J Pharmacol. 1995;273:303–6.
Kaneda M, Oyama Y, Ikemoto Y, Akaike N. Blockade of the voltage-dependent sodium current in isolated rat hippocampal neurons by tetrodotoxin and lidocaine. Brain Res. 1989;484:348–51.
Xu YQ, Pickoff AS, Clarkson CW. Evidence for developmental changes in sodium channel inactivation gating and sodium channel block by phenytoin in rat cardiac myocytes. Circ Res. 1991;69:644–56.
Lucas PT, Meadows LS, Nicholls J, Ragsdale DS. An epilepsy mutation in the beta1 subunit of the voltage-gated sodium channel results in reduced channel sensitivity to phenytoin. Epilepsy Res. 2005;64:77–84.
Gastens AM, Brandt C, Bankstahl JP, Loscher W. Predictors of pharmacoresistant epilepsy: pharmacoresistant rats differ from pharmacoresponsive rats in behavioral and cognitive abnormalities associated with experimentally induced epilepsy. Epilepsia. 2008;49:1759–76.
Villasana-Salazar B, Vezzani A. Neuroinflammation microenvironment sharpens seizure circuit. Neurobiol Dis. 2023;178:106027.
Zhang S, Xie S, Zheng Y, Chen Z, Xu C. Current advances in rodent drug-resistant temporal lobe epilepsy models: Hints from laboratory studies. Neurochem Int. 2024;174:105699.
Berg AT, Langfitt J, Shinnar S, Vickrey BG, Sperling MR, Walczak T, et al. How long does it take for partial epilepsy to become intractable? Neurology. 2003;60:186–90.
Berg AT. The natural history of mesial temporal lobe epilepsy. Curr Opin Neurol. 2008;21:173–8.
Oliva M, Berkovic SF, Petrou S. Sodium channels and the neurobiology of epilepsy. Epilepsia. 2012;53:1849–59.
Ellis CA, Petrovski S, Berkovic SF. Epilepsy genetics: clinical impacts and biological insights. Lancet Neurol. 2020;19:93–100.
Barker BS, Nigam A, Ottolini M, Gaykema RP, Hargus NJ, Patel MK. Pro-excitatory alterations in sodium channel activity facilitate subiculum neuron hyperexcitability in temporal lobe epilepsy. Neurobiol Dis. 2017;108:183–94.
Loscher W, Klitgaard H, Twyman RE, Schmidt D. New avenues for anti-epileptic drug discovery and development. Nat Rev Drug Discov. 2013;12:757–76.
Tang X, Chen X, Li X, Cheng H, Gan J, Liu Z. The TLR4 mediated inflammatory signal pathway might be involved in drug resistance in drug-resistant epileptic rats. J Neuroimmunol. 2022;365:577802.
Chan PS, Zhang C, Zuo Z, Kwan P, Baum L. In vitro transport assays of rufinamide, pregabalin, and zonisamide by human P-glycoprotein. Epilepsy Res. 2014;108:359–66.
Owen A, Pirmohamed M, Tettey JN, Morgan P, Chadwick D, Park BK. Carbamazepine is not a substrate for P-glycoprotein. Br J Clin Pharmacol. 2001;51:345–9.
Li M, Sun X, Wang Z, Li Y. Caspase-1 affects chronic restraint stress-induced depression-like behaviors by modifying GABAergic dysfunction in the hippocampus. Transl Psychiatry. 2023;13:229.
Xu D, Liu J, Meng S, Sun M, Chen Y, Hong Y. Isoflurane-induced neuroinflammation and NKCC1/KCC2 dysregulation result in long-term cognitive disorder in neonatal mice. BMC Anesthesiol. 2024;24:200.
Malaguarnera M, Balzano T, Castro MC, Llansola M, Felipo V. The dual role of the GABA(A) receptor in peripheral inflammation and neuroinflammation: a study in hyperammonemic rats. Int J Mol Sci. 2021;22:6772.
Zhao J, Zheng Y, Liu K, Chen J, Lai N, Fei F, et al. HMGB1 is a therapeutic target and biomarker in diazepam-refractory status epilepticus with wide time window. Neurotherapeutics. 2020;17:710–21.
Li MX, Zheng HL, Luo Y, He JG, Wang W, Han J, et al. Gene deficiency and pharmacological inhibition of caspase-1 confers resilience to chronic social defeat stress via regulating the stability of surface AMPARs. Mol Psychiatry. 2018;23:556–68.
Taraschenko O, Fox HS, Eldridge E, Heliso P, Al-Saleem F, Dessain S, et al. MyD88-mediated signaling is critical for the generation of seizure responses and cognitive impairment in a model of anti-N-methyl-D-aspartate receptor encephalitis. Epilepsia. 2024;65:1475–87.
Li QY, Chen SX, Liu JY, Yao PW, Duan YW, Li YY, et al. Neuroinflammation in the anterior cingulate cortex: the potential supraspinal mechanism underlying the mirror-image pain following motor fiber injury. J Neuroinflammation. 2022;19:162.
Huang CJ, Moczydlowski E. Cytoplasmic polyamines as permeant blockers and modulators of the voltage-gated sodium channel. Biophys J. 2001;80:1262–79.
Xu W, Gao L, Li T, Shao A, Zhang J. Neuroprotective role of agmatine in neurological diseases. Curr Neuropharmacol. 2018;16:1296–305.
Ragsdale DS, McPhee JC, Scheuer T, Catterall WA. Molecular determinants of state-dependent block of Na+ channels by local anesthetics. Science. 1994;265:1724–8.
Ragsdale DS, McPhee JC, Scheuer T, Catterall WA. Common molecular determinants of local anesthetic, antiarrhythmic, and anticonvulsant block of voltage-gated Na+ channels. Proc Natl Acad Sci USA. 1996;93:9270–5.
Xu TT, Li H, Dai Z, Lau GK, Li BY, Zhu WL, et al. Spermidine and spermine delay brain aging by inducing autophagy in SAMP8 mice. Aging. 2020;12:6401–14.
Gupta VK, Scheunemann L, Eisenberg T, Mertel S, Bhukel A, Koemans TS, et al. Restoring polyamines protects from age-induced memory impairment in an autophagy-dependent manner. Nat Neurosci. 2013;16:1453–60.
Fisher RS. Deep brain stimulation of thalamus for epilepsy. Neurobiol Dis. 2023;179:106045.
Sheng J, Liu S, Qin H, Li B, Zhang X. Drug-resistant epilepsy and surgery. Curr Neuropharmacol. 2018;16:17–28.
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (No. 82173796, 82374064, 82330116), the Natural Science Foundation of Zhejiang Province (No. LQ24H310002), and the Research Project of Zhejiang Chinese Medical University (2023JKZDZC04).
Author information
Authors and Affiliations
Contributions
CLX, ZC and MQY designed research. MQY, XYQ, SZ and XMY performed research. MQY, XYQ, SZ, XMY, MJS, YZY, YWG, SZ, MHL and FF analyzed data. MQY, ZC and CLX wrote the paper. YD, YW, and YYT revised the paper. YYT, CZ and CXL supervised this study.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yan, Mq., Qiu, Xy., Zhang, S. et al. Neuroinflammation leads to pharmacoresistance in temporal lobe epilepsy via promoting spermine degradation. Acta Pharmacol Sin 46, 2908–2923 (2025). https://doi.org/10.1038/s41401-025-01594-8
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41401-025-01594-8
Keywords
This article is cited by
-
The Thalamic Reticular Ultimatum: Carbamazepine’s Betrayal in Absence Epileptic Seizures
Neuroscience Bulletin (2025)