Abstract
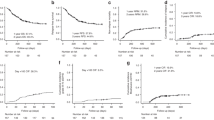
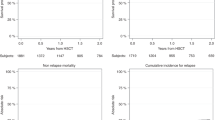
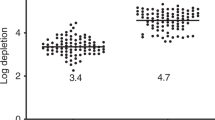
Efficacy of an ambulatory hematopoietic stem cell transplant (HSCT) program with a reduced intensity conditioning regimen (RIC) in malignant hematological diseases was assessed. We analyzed 217 patients who underwent HSCT from August 2013 to July 2017. There were 78 (35.9%) HLA-identical, 56 (25.8%) haploidentical, and 83 (38.2%) autologous transplants. Two-year transplant-related mortality (TRM) for HLA-identical, haploidentical, and auto grafts were 20%, 25%, and 2.5%; relapse/progression was 44%, 60%, and 55%; overall survival (OS) was 61%, 44.8%, and 78.0%; and disease-free survival (DFS) was 36.8%, 26.5%, and 43.5%, respectively. Factors associated with a high risk of TRM were male sex (HR = 2.62, P = 0.031), fever and neutropenia (HR = 3.30, P = 0.023), and cell dose < 5 × 106 CD34 +/kg (HR = 4.24, P = 0.001); cGVHD was a protective factor for TRM (HR = 0.29, P = 0.022). Transfusion was associated with increased risk of relapse/progression in univariate and multivariate analysis (HR = 3.10, P = 0.001 and HR = 3.30, P = 0.004); cGVHD was a protective factor (HR = 0.18, P = 0.001 and HR = 0.17, P = 0.002). In a multivariate analysis for allo-HSCT, infections were associated with high risk of mortality (HR = 3.90, P = 0.016) and transfusion with reduced DFS (HR = 2.76, P = 0.029); for haplo-HSCT, CD34 + < 5 × 106/kg was a risk factor for mortality and lower DFS (HR = 5.41, P = 0.001 and HR = 3.93, P = 0.001). Outcomes of our RIC-based outpatient transplant program are comparable to excellence centers in high-income countries.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Jaime-Perez JC, Heredia-Salazar AC, Cantu-Rodriguez OG, Gutierrez-Aguirre H, Villarreal-Villarreal CD, Mancias-Guerra C, et al. Cost structure and clinical outcome of a stem cell transplantation program in a developing country: the experience in Northeast Mexico. Oncologist. 2015;20:386–92.
Gratwohl A, Baldomero H, Aljurf M, Pasquini MC, Bouzas LFYA. et al. Hematopoietic stem cell transplantation: a global perspective. JAMA. 2010;303:1617–24.
Jaimovich G, Martinez Rolon J, Baldomero H, Rivas M, Hanesman I, Bouzas L, et al. Latin America: the next region for haematopoietic transplant progress. Bone Marrow Transplant. 2017;52:671–7.
Barrett AJ, Savani BN. Stem cell transplantation with reduced-intensity conditioning regimens: a review of ten years experience with new transplant concepts and new therapeutic agents. Leukemia. 2006;20:1661–72.
Ruiz-Argüelles GJ. Historia del trasplante de médula ósea en México. Rev Biomed. 2005;16:207–13.
Gomez-Almaguer D, Ruiz-Arguelles GJ, Ruiz-Arguelles A, Gonzalez-Llano O, Cantu OE, Hernandez NE. Hematopoietic stem cell allografts using a non-myeloablative conditioning regimen can be safely performed on an outpatient basis: report of four cases. Bone Marrow Transpl. 2000;25:131–3.
Jaime-Pérez JC, Villarreal-Villarreal CD, Méndez-Ramírez N, Vázquez-Garza E, Salazar-Riojas R, Gómez-Almaguer D. Assessment of immune reconstitution status in recipients of a successful hematopoietic stem cell transplant from peripheral blood after reduced intensity conditioning. Blood Cells Mol Dis. 2016;58:52–6.
Ruiz-Delgado GJ, Rodriguez-Romo L, Tarin-Arzaga LC, Lutz-Presno J, Gomez-Almaguer D, Ruiz-Arguelles GJ. Reduced-intensity allografting in childhood acute lymphoblastic leukemia. Biol Blood Marrow Transpl. 2011;17:439–40.
Ruiz-Argüelles GJ, Gómez-Almaguer D, Ruiz-Argüelles A, Gonzalez-Llano O, Cant OG, Jaime-Pérez JC. Results of an outpatient-based stem cell allotransplant program using nonmyeloablative conditioning regimens. Am J Hematol. 2001;66:241–4.
Howard CA, Fernandez-Vina MA, Appelbaum FR, Confer DL, Devine SM, Horowitz MM, et al. Recommendations for donor human leukocyte antigen assessment and matching for allogeneic stem cell transplantation: consensus opinion of the blood and marrow transplant clinical trials network (BMT CTN). Biol Blood Marrow Transplant. 2015;21:4–7.
Schiffer BCA, Anderson KC, Bennett CL, Bernstein S, Elting LS, Goldsmith M, et al. Platelet transfusion for patients with cancer: clinical practice guidelines of the American Society of Clinical Oncology. J Clin Oncol. 2001;19:1519–38.
Rizzo JD, Wingard JR, Tichelli A, Lee SJ, van Lint MT, Burns LJ, et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation: joint recommendations of the European Group for Blood and Marrow Transplantation, Center for International Blood and Marrow Transplant Research. Bone Marrow Transplant. 2006;37:249–61.
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, et al. National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: I. diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11:945–56.
DiPersio JF, Micallef IN, Stiff PJ, Bolwell BJ, Maziarz RT, Jacobsen E, et al. Phase III prospective randomized double-blind placebo-controlled trial of plerixafor plus granulocyte colony-stimulating factor compared with placebo plus granulocyte colony-stimulating factor for autologous stem-cell mobilization and transplantation for patients with non-Hodgkin's lymphoma. J Clin Oncol. 2009;27:4767–73.
Tiwari A, Arora D, Dara R, Dorwal P, Sood N, Misra R, et al. Newly established stem cell transplant program: 100 days follow-up of patients and its comparison with published Indian literature. Indian J Med Paediatr Oncol. 2016;37:168.
Pinkel D, Straume T, Gray JW. Cytogenetic analysis using quantitative, high-sensitivity, fluorescence hybridization. Proc Natl Acad Sci USA. 1986;83:2934–8.
Valcárcel D, Martino R, Caballero D, Mateos MV, Pérez-Simón JA, Canals C, et al. Chimerism analysis following allogeneic peripheral blood stem cell transplantation with reduced-intensity conditioning. Bone Marrow Transplant. 2003;31:387–92.
Olsson RF, Logan BR, Chaudhury S, Zhu X, Akpek G, Bolwell BJ, et al. Primary graft failure after myeloablative allogeneic hematopoietic cell transplantation for hematologic malignancies. Leukemia. 2015;29:1754–62.
Scrucca L, Santucci A, Aversa F. Competing risk analysis using R: an easy guide for clinicians. Bone Marrow Transplant. 2007;40:381–7.
O’Donnell PaulV, Eapen Mary, Horowitz MaryM, Logan BrentR, DiGilio Alyssa, Brunstein Claudio, et al. Comparable outcomes with marrow or peripheral blood as stem cell sources for hematopoietic cell transplantation from haploidentical donors after non-ablative conditioning: a matched-pair analysis. Bone Marrow Transplant. 2016;51:1599–601.
Pidala J, Anasetti C, Kharfan-Dabaja MA, Cutler C, Sheldon A, Djulbegovic B. Decision analysis of peripheral blood versus bone marrow hematopoietic stem cells for allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2009;15:1415–21.
Bensinger WI. Allogeneic transplantation: peripheral blood versus bone marrow. Curr Opin Oncol. 2012;24:191–6.
Raiola AM, Dominietto A, di Grazia C, Lamparelli T, Gualandi F, Ibatici A, et al. Unmanipulated haploidentical transplants compared with other alternative donors and matched sibling grafts. Biol Blood Marrow Transplant. 2014;20:1573–9.
Solh M, Zhang X, Connor K, Brown S, Solomon SR, Morris LE, et al. Post-relapse survival after haploidentical transplantation vs matched-related or matched-unrelated hematopoietic cell transplantation. Bone Marrow Transplant. 2016;51:949–54.
Majhail NS. Long-term complications after hematopoietic cell transplantation. Hematol Oncol Stem Cell Ther. 2017;10:220–7.
Atilla E, Ataca P, Sinem A, Bozdag C, Demirer T. A review of infectious complications after haploidentical hematopoietic stem cell transplantations. Infection. 2017;45:403–4011.
Desjonqueres A, Illiaquer M, Duquesne A, Le Bris Y, Peterlin P, Guillaume T, et al. Longer delay of hematological recovery and increased transfusion needs after haploidentical compared to non-haploidentical stem cell transplantation. Bone Marrow Transplant. 2016;51:1150–2.
Christou G, Kekre N, Petrcich W, Tokessy M, Neurath D, Giulivi A, et al. Impact of platelet transfusion on toxicity and mortality after hematopoietic progenitor cell transplantation. Transfusion. 2015;55:253–8.
Gratwohl A, Brand R, Frassoni F, Rocha V, Niederwieser D, Reusser P, et al. Cause of death after allogeneic haematopoietic stem cell transplantation (HSCT) in early leukaemias: an EBMT analysis of lethal infectious complications and changes over calendar time. Bone Marrow Transplant. 2005;36:757–69.
Slade M, Goldsmith S, Romee R, DiPersio JF, Dubberke ER, Westervelt P, et al. Epidemiology of infections following haploidentical peripheral blood hematopoietic cell transplantation. Transpl Infect Dis. 2017;19. https://doi.org/10.1111/tid.12629.
Chantepie SP, Mear J-B, Parienti J-J, Bazin A, Benabed K, Cheze S, et al. Blood transfusion in hematologic intensive care unit. Transfusion. 2017;57:296–302.
Elemary M, Seghatchian J, Stakiw J, Bosch M, Sabry W, Goubran H. Transfusion challenges in hematology oncology and hematopoietic stem cell transplant – literature review and local experience. Transfus Apher Sci. 2017;56:317–21.
Jaime-Pérez JC, Villarreal-Villarreal CD, Salazar-Riojas R, Méndez-Ramírez N, Vázquez-Garza E, Gómez-Almaguer D. Increased bacterial infections after transfusion of leukoreduced non-irradiated blood products in recipients of allogeneic stem cell transplants after reduced-intensity conditioning. Biol Blood Marrow Transplant. 2015;21:526–30.
Jaime-Pérez JC, Colunga-Pedraza PR, Gó Mez-Almaguer D. Is the number of blood products transfused associated with lower survival in children with acute lymphoblastic leukemia? Pediatr Blood Cancer. 2011;57:217–23.
Sung AD, Chao NJ. Concise review: acute graft-versus-host disease: immunobiology, prevention, and treatment. Stem Cells Transl Med. 2013;2:25–32.
McCurdy SR, Kanakry CG, Kasamon YL, Bolanos Meade J, Tsai H-L, Showel MM, et al. Graft-versus-host disease (GVHD) and survival outcomes after HLA-haploidentical (Haplo) bone marrow transplant (BMT) compare favorably with matched related donor (MRD), and matched unrelated donor (MUD) BMT utilizing high-dose posttransplantation Cyclophosphamide (PTCy). Blood. 2014;124:730 LP–730.
Chang YJ, Zhao XY, Huo MR, Xu LP, Liu DH, Liu KY, et al. Immune reconstitution following unmanipulated HLA-Mismatched/Haploidentical transplantation compared with HLA-identical sibling transplantation. J Clin Immunol. 2012;32:268–80.
Blaise D, Fürst S, Crocchiolo R, El-cheikh J, Granata A, Harbi S, et al. Haploidentical T-cell replete transplantation with post-transplant cyclophosphamide for patients in or above the 6th decade of age compared with allogeneic hematopoietic stem cell transplantation from an HLA-matched related or unrelated donor. Biol Blood Marrow Transplant. 2016;22:119–24.
Boyiadzis M, Arora M, Klein JP, Hassebroek A, Hemmer M, Urbano-Ispizua A, et al. Impact of chronic graft-versus-host disease on late relapse and survival on 7489 patients after myeloablative allogeneic hematopoietic cell transplantation for leukemia. Clin Cancer Res. 2015;21:2020–8.
Itonaga H, Iwanaga M, Aoki K, Aoki J, Ishiyama K, Ishikawa T, et al. Impacts of graft-versus-host disease on outcomes after allogeneic hematopoietic stem cell transplantation for chronic myelomonocytic leukemia: a nationwide retrospective study. Leuk Res. 2016;41:48–55.
Ghosh N, Karmali R, Rocha V, Ahn KW, DiGilio A, Hari PN, et al. Reduced-intensity transplantation for lymphomas using haploidentical related donors versus HLA-matched sibling donors: a center for international blood and marrow transplant research analysis. J Clin Oncol. 2016;34:3141–9.
Brammer JE, Stentz A, Gajewski J, Curtin P, Hayes-Lattin B, Kovacsovics T, et al. Nonmyeloablative allogeneic hematopoietic stem cell transplant for the treatment of patients with hematologic malignancies using busulfan, fludarabine, and total body irradiation conditioning is effective in an elderly and infirm population. Biol Blood Marrow Transplant. 2015;21:89–96.
Long H, Lu ZG, Song CY, Huang YX, Xu JH, Xu JX, et al. Long-term outcomes of HLA-haploidentical stem cell transplantation based on an FBCA conditioning regimen compared with those of HLA-identical sibling stem cell transplantation for haematologic malignancies. Bone Marrow Transplant. 2016;51:1470–5.
Bittencourt H, Rocha V, Chevret S, Socié G, Espérou H, Devergie A, et al. Association of CD34 cell dose with hematopoietic recovery, infections, and other outcomes after HLA-identical sibling bone marrow transplantation. Blood. 2002;99:2726–33.
Gómez-Almaguer Gómez-PeñaÁ, Jaime-Pérez JC, Gómez-Guijosa MÁ, Cantú-Rodríguez OG-AH, et al. Higher doses of CD341 progenitors are associated with improved overall survival without increasing GVHD in reduced intensity conditioning allogeneic transplant recipients with clinically advanced disease. J Clin Apher. 2013;28:349–55.
G Rondón, RM Saliba, I Khouri, S Giralt, K Chan, E Jabbour, et al. Long term follow up of patients who experienced graft failure post allogeneic progenitor cell transplantation. Results of a single institution analysis. Biol Blood Marrow Transpl. 2008;14:859–66.
Ali N, Adil SN, Shaikh MU. Autologous hematopoietic stem cell transplantation 10 years of data from a developing country. Stem Cells Transl Med. 2015;4:873–7.
Klyuchnikov E, Bacher U, Ahn KW, Carreras J, Nicolaus M, Hari PN, et al. Long-term survival outcomes of reduced-intensity allogeneic or autologous transplantation in relapsed grade 3 follicular lymphoma. Bone Marrow Transpl. 2016;51:58–66.
Lazarus HM, Zhang M, Carreras J, Hayes BM, Ataergin AS, Bitran JD, et al. Comparison of autologous and allogeneic hematopoietic stem cell transplantation for 140 patients with de novo acute leukemia in first complete remission. Blood. 2011;16:35–45.
Hsieh SI, Johantgen M, Hsu LL, Kuo MC, Lu TH. Are structural characteristics of programs and hospitals associated with 100-day readmission of hematopoietic SCTs in Taiwan. Bone Marrow Transplant. 2011;46:1203–9.
Acknowledgements
We thank Dr. José Javier Sánchez-Hernández for his review of the statistical analysis. We thank Sergio Lozano-Rodriguez, M.D., for his help in editing the manuscript.
Funding:
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Jaime-Pérez, J.C., Salazar-Cavazos, L., Aguilar-Calderón, P. et al. Assessing the efficacy of an ambulatory peripheral blood hematopoietic stem cell transplant program using reduced intensity conditioning in a low-middle-income country. Bone Marrow Transplant 54, 828–838 (2019). https://doi.org/10.1038/s41409-018-0338-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-018-0338-7
This article is cited by
-
Outpatient transplantation in the COVID-19 era: a single-center Latin American experience
Bone Marrow Transplantation (2021)