Abstract
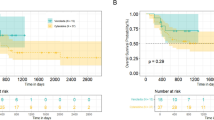
Outcomes after ASCT are highly variable making it difficult to predict risk of disease progression. We analyzed the impact of clinically available immune-related biomarkers on treatment-free survival (TFS) in 130 patients receiving Mel200 and ASCT. Absolute lymphocyte count (ALC), monocyte count (AMC), neutrophil count (ANC), and immunoglobulin (Ig) levels were collected on day −2 and 90 of ASCT. The lymphocyte–monocyte (LMR) and neutrophil–lymphocyte ratios (NLR) were then derived. At Day +90, we found that low ALC (18 versus 23 months, p = 0.04) or AMC (13 versus 25 months, p = 0.02) predicted for worse TFS. A low LMR predicted for worse TFS (16 versus 52 months, p = 0.004). Patients with two or three suppressed Ig levels had worse TFS (17 versus 51 months, p = 0.04). Median TFS for poor (low LMR and 2–3 suppressed Ig), intermediate, and good (high LMR and 0–1 suppressed Ig) risk groups was 7.5 versus 27 versus 79 months, respectively (p = 0.0004). In a multivariate analysis, a low LMR and suppressed Ig levels were strong independent predictors of poor TFS. We propose an immune score combining these available tests to stratify patients at risk for early progression and identify those who may benefit from intensified post-ASCT consolidation or immunotherapy based approaches.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
SEER. Cancer Stat Facts: Myeloma. National Cancer Institute; (Bethesda, Maryland, 2018).
Attal M, Lauwers-Cances V, Hulin C, Leleu X, Caillot D, Escoffre M, et al. Lenalidomide, bortezomib, and dexamethasone with transplantation for myeloma. N Engl J Med. 2017;376:1311–20. https://doi.org/10.1056/NEJMoa1611750.
Dhakal B, Szabo A, Chhabra S, Hamadani M, D’Souza A, Usmani SZ, et al. Autologous transplantation for newly diagnosed multiple myeloma in the era of novel agent induction: a systematic review and meta-analysis. JAMA Oncol. 2018;4:343–50. https://doi.org/10.1001/jamaoncol.2017.4600.
Attal M, Harousseau JL, Stoppa AM, Sotto JJ, Fuzibet JG, Rossi JF, et al. A prospective, randomized trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma. Intergroupe Francais du Myelome. N Engl J Med. 1996;335:91–7. https://doi.org/10.1056/NEJM199607113350204.
Child JA, Morgan GJ, Davies FE, Owen RG, Bell SE, Hawkins K, et al. High-dose chemotherapy with hematopoietic stem-cell rescue for multiple myeloma. N Engl J Med. 2003;348:1875–83. https://doi.org/10.1056/NEJMoa022340.
Martinez-Lopez J, Blade J, Mateos MV, Grande C, Alegre A, Garcia-Larana J, et al. Long-term prognostic significance of response in multiple myeloma after stem cell transplantation. Blood. 2011;118:529–34. https://doi.org/10.1182/blood-2011-01-332320.
Munshi NC, Avet-Loiseau H, Rawstron AC, Owen RG, Child JA, Thakurta A, et al. Association of minimal residual disease with superior survival outcomes in patients with multiple myeloma: a meta-analysis. JAMA Oncol. 2017;3:28–35. https://doi.org/10.1001/jamaoncol.2016.3160.
Moreau P, Attal M, Caillot D, Macro M, Karlin L, Garderet L, et al. Prospective evaluation of magnetic resonance imaging and [(18)F]fluorodeoxyglucose positron emission tomography-computed tomography at diagnosis and before maintenance therapy in symptomatic patients with multiple myeloma included in the IFM/DFCI 2009 trial: results of the IMAJEM study. J Clin Oncol. 2017;35:2911–8. https://doi.org/10.1200/JCO.2017.72.2975.
Pruzanski W, Gidon MS, Roy A. Suppression of polyclonal immunoglobulins in multiple myeloma: relationship to the staging and other manifestations at diagnosis. Clin Immunol Immunopathol. 1980;17:280–6.
Wang L, Young DC. Suppression of polyclonal immunoglobulin production by M-proteins shows isotype specificity. Ann Clin Lab Sci. 2001;31:274–8.
Heaney JLJ, Campbell JP, Iqbal G, Cairns D, Richter A, Child JA, et al. Characterisation of immunoparesis in newly diagnosed myeloma and its impact on progression-free and overall survival in both old and recent myeloma trials. Leukemia. 2018;32:1727–38. https://doi.org/10.1038/s41375-018-0163-4.
Gonzalez-Calle V, Cerda S, Labrador J, Sobejano E, Gonzalez-Mena B, Aguilera C, et al. Recovery of polyclonal immunoglobulins one year after autologous stem cell transplantation as a long-term predictor marker of progression and survival in multiple myeloma. Haematologica. 2017;102:922–31. https://doi.org/10.3324/haematol.2016.158345.
Pessoa de Magalhaes RJ, Vidriales MB, Paiva B, Fernandez-Gimenez C, Garcia-Sanz R, Mateos MV, et al. Analysis of the immune system of multiple myeloma patients achieving long-term disease control by multidimensional flow cytometry. Haematologica. 2013;98:79–86. https://doi.org/10.3324/haematol.2012.067272.
Dosani T, Covut F, Beck R, Driscoll JJ, de Lima M, Malek E. Significance of the absolute lymphocyte/monocyte ratio as a prognostic immune biomarker in newly diagnosed multiple myeloma. Blood Cancer J. 2017;7:e579. https://doi.org/10.1038/bcj.2017.60.
Kelkitli E, Atay H, Cilingir F, Guler N, Terzi Y, Ozatli D, et al. Predicting survival for multiple myeloma patients using baseline neutrophil/lymphocyte ratio. Ann Hematol. 2014;93:841–6. https://doi.org/10.1007/s00277-013-1978-8.
Romano A, Parrinello NL, Consoli ML, Marchionni L, Forte S, Conticello C, et al. Neutrophil to lymphocyte ratio (NLR) improves the risk assessment of ISS staging in newly diagnosed MM patients treated upfront with novel agents. Ann Hematol. 2015;94:1875–83. https://doi.org/10.1007/s00277-015-2462-4.
Shi L, Qin X, Wang H, Xia Y, Li Y, Chen X, et al. Elevated neutrophil-to-lymphocyte ratio and monocyte-to-lymphocyte ratio and decreased platelet-to-lymphocyte ratio are associated with poor prognosis in multiple myeloma. Oncotarget. 2017;8:18792–801. https://doi.org/10.18632/oncotarget.13320.
Shin SJ, Roh J, Kim M, Jung MJ, Koh YW, Park CS, et al. Prognostic significance of absolute lymphocyte count/absolute monocyte count ratio at diagnosis in patients with multiple myeloma. Korean J Pathol. 2013;47:526–33. https://doi.org/10.4132/KoreanJPathol.2013.47.6.526.
Wongrakpanich S, George G, Chaiwatcharayut W, Biso S, Candelario N, Mittal V, et al. The prognostic significance of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in patients with multiple myeloma. J Clin Lab Anal. 2016;30:1208–13. https://doi.org/10.1002/jcla.22004.
Palumbo A, Avet-Loiseau H, Oliva S, Lokhorst HM, Goldschmidt H, Rosinol L, et al. Revised international staging system for multiple myeloma: a report from international myeloma working group. J Clin Oncol. 2015;33:2863–9. https://doi.org/10.1200/JCO.2015.61.2267.
Onec B, Okutan H, Albayrak M, Saribacak Can E, Aslan V, Unver Koluman B, et al. The predictive role of the neutrophil/lymphocyte ratio in survival with multiple myeloma: a single center experience. J Clin Lab Anal. 2017; 31. https://doi.org/10.1002/jcla.22032.
Kastritis E, Zagouri F, Symeonidis A, Roussou M, Sioni A, Pouli A, et al. Preserved levels of uninvolved immunoglobulins are independently associated with favorable outcome in patients with symptomatic multiple myeloma. Leukemia. 2014;28:2075–9. https://doi.org/10.1038/leu.2014.110.
Romano A, Laura Parrinello N, Cerchione C, Letizia Consoli M, Parisi M, Calafiore V, et al. The NLR and LMR ratio in newly diagnosed MM patients treated upfront with novel agents. Blood Cancer J. 2017;7:649. https://doi.org/10.1038/s41408-017-0019-6.
Perez-Persona E, Vidriales MB, Mateo G, Garcia-Sanz R, Mateos MV, de Coca AG, et al. New criteria to identify risk of progression in monoclonal gammopathy of uncertain significance and smoldering multiple myeloma based on multiparameter flow cytometry analysis of bone marrow plasma cells. Blood. 2007;110:2586–92. https://doi.org/10.1182/blood-2007-05-088443.
Sorrig R, Klausen TW, Salomo M, Vangsted AJ, Ostergaard B, Gregersen H, et al. Smoldering multiple myeloma risk factors for progression: a Danish population-based cohort study. Eur J Haematol. 2016;97:303–9. https://doi.org/10.1111/ejh.12728.
Rajkumar SV, Landgren O, Mateos MV. Smoldering multiple myeloma. Blood. 2015;125:3069–75. https://doi.org/10.1182/blood-2014-09-568899.
Romano A, Conticello C, Cavalli M, Vetro C, La Fauci A, Parrinello NL, et al. Immunological dysregulation in multiple myeloma microenvironment. Biomed Res Int. 2014;2014:198539. https://doi.org/10.1155/2014/198539.
Berardi S, Ria R, Reale A, De Luisi A, Catacchio I, Moschetta M, et al. Multiple myeloma macrophages: pivotal players in the tumor microenvironment. J Oncol. 2013;2013:183602. https://doi.org/10.1155/2013/183602.
Asimakopoulos F, Kim J, Denu RA, Hope C, Jensen JL, Ollar SJ, et al. Macrophages in multiple myeloma: emerging concepts and therapeutic implications. Leuk Lymphoma. 2013;54:2112–21. https://doi.org/10.3109/10428194.2013.778409.
Malek E, de Lima M, Letterio JJ, Kim BG, Finke JH, Driscoll JJ, et al. Myeloid-derived suppressor cells: The green light for myeloma immune escape. Blood Rev. 2016;30:341–8. https://doi.org/10.1016/j.blre.2016.04.002.
Gorgun GT, Whitehill G, Anderson JL, Hideshima T, Maguire C, Laubach J, et al. Tumor-promoting immune-suppressive myeloid-derived suppressor cells in the multiple myeloma microenvironment in humans. Blood. 2013;121:2975–87. https://doi.org/10.1182/blood-2012-08-448548.
Beider K, Bitner H, Leiba M, Gutwein O, Koren-Michowitz M, Ostrovsky O, et al. Multiple myeloma cells recruit tumor-supportive macrophages through the CXCR4/CXCL12 axis and promote their polarization toward the M2 phenotype. Oncotarget. 2014;5:11283–96. https://doi.org/10.18632/oncotarget.2207.
Zheng Y, Cai Z, Wang S, Zhang X, Qian J, Hong S, et al. Macrophages are an abundant component of myeloma microenvironment and protect myeloma cells from chemotherapy drug-induced apoptosis. Blood. 2009;114:3625–8. https://doi.org/10.1182/blood-2009-05-220285.
Jimenez-Zepeda VH, Reece DE, Trudel S, Chen C, Franke N, Winter A, et al. Absolute lymphocyte count as predictor of overall survival for patients with multiple myeloma treated with single autologous stem cell transplant. Leuk Lymphoma. 2015;56:2668–73. https://doi.org/10.3109/10428194.2014.1003057.
Kim H, Sohn HJ, Kim S, Lee JS, Kim WK, Suh C. Early lymphocyte recovery predicts longer survival after autologous peripheral blood stem cell transplantation in multiple myeloma. Bone Marrow Transplant. 2006;37:1037–42. https://doi.org/10.1038/sj.bmt.1705373.
Porrata LF. Autologous graft-versus-tumor effect: reality or fiction? Adv Hematol. 2016;2016:5385972. https://doi.org/10.1155/2016/5385972.
Chung DJ, Pronschinske KB, Shyer JA, Sharma S, Leung S, Curran SA, et al. T-cell exhaustion in multiple myeloma relapse after autotransplant: optimal timing of immunotherapy. Cancer Immunol Res. 2016;4:61–71. https://doi.org/10.1158/2326-6066.CIR-15-0055.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
PP receives honoraria from Celgene, Janssen and Amgen and consulting fees from Celgene and Amgen. The other authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sweiss, K., Lee, J., Mahmud, N. et al. Combined immune score of lymphocyte to monocyte ratio and immunoglobulin levels predicts treatment-free survival of multiple myeloma patients after autologous stem cell transplant. Bone Marrow Transplant 55, 199–206 (2020). https://doi.org/10.1038/s41409-019-0681-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-019-0681-3
This article is cited by
-
Clinical significance of the lymphocyte-to-monocyte ratio in multiple myeloma patients with negative minimal residual disease: a single-center retrospective analysis
International Journal of Hematology (2021)