Abstract
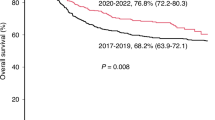
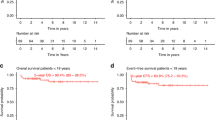
In this retrospective study, we evaluated long-term survival and late effects in 137 patients affected by thalassemia major (TM) who received an allogeneic hematopoietic cell transplantation (HCT). Median age at HCT was 10.1 years. After a median follow-up of 30 years, 114 (83.2%) patients are living and 108 (78.8%) are cured. The cumulative incidence of nonrelapse mortality and thalassemia recurrence was 9.5% at 1 year and 10.2% at 39 years respectively. The 39-years cumulative incidence of overall survival and disease-free survival were 81.4% and 74.5%. One hundred twenty-three patients who survived more than 2 years after HCT were evaluated for late effects concerning hematological disorders, iron burden, growth, obesity, diabetes mellitus, thyroid and gonadal function, eye, heart, liver, lung, kidney, gastrointestinal, neurologic and psychiatric system, osteoarticular system, secondary solid cancer (SSC), performance status, and Covid-19 infection. Fertility was preserved in 21 males whose partners delivered 34 neonates and 25 females who delivered 26 neonates. Fifteen cases of SSC were diagnosed for a 39-year cumulative incidence of 16.4%. HCT represents a definitive cure for the majority of TM patients at the price, however, of a non-negligible early and late mortality which in the long run affects survival and disease-free survival.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available upon reasonable request from the corresponding authors.
References
Angelucci E, Barosi G, Camaschella C, Cappellini MD, Cazzola M, Galanello R, et al. Italian Society of Hematology practice guidelines for the management of iron over- load in thalassemia major and related disorders. Haematologica. 2008;93:741–52.
Piga A, Perrotta S, Gamberini MP, Voskaridou E, Melpignano A, Filosa A, et al. Luspatercept improves hemoglobin levels and blood transfusion requirements in a study of patients with ß-thalassemia. Blood. 2019;133:1279–89.
Cappellini MD, Viprakasit V, Taher AT, Georgiev P, Kuo KHM, Coates T, et al. A Phase 3 Trial of Luspatercept in Patients with Transfusion-Dependent ß-Thalassemia. N. Engl J Med. 2020;382:1219–31.
Cavazzana-Calvo M, Payen E, Negre O, Wang G, Hehir K, Fusil F, et al. Transfusion independence and HMGA2 activation after gene therapy of human beta-thalassaemia. Nature. 2010;467:318–22.
Thompson AA, Walters MC, Kwiatkowski J, Rasko JEL, Ribeil J-A, Hongeng S, et al. Gene Therapy in Patients with Transfusion-Dependent ß-Thalassemia. N. Engl J Med. 2018;378:1479–93.
Locatelli F, Thompson AA, Kwiatkowski JL, Porter JB, Thrasher AJ, Hongeng S, et al. Betibeglogene Autotemcel Gene Therapy for Non- ß0/ ß0 Genotype ß-Thalassemia. N. Engl J Med. 2022;386:415–27.
Payen E. Efficacy and Safety of Gene Therapy for ß-Thalassemia. N. Engl J Med. 2022;386:488–90.
Thomas ED, Buckner CD, Sanders JE, Papayannopoulou T, Borgna-Pignatti C, De Stefano P, et al. Marrow transplantation for thalassaemia. Lancet. 1982;2:227–9.
Baronciani D, Angelucci E, Potschger U, Gaziev J, Yesillipek A, Zecca M, et al. Hemopoietic stem cell transplantation in thalassemia: a report from the European Society for Blood and Bone Marrow Transplantation Hemoglobinopathy Registry, 2000–2010. Bone Marrow Transpl. 2016;51:536–41.
Angelucci E. Hematopoietic stem cell transplantation in Thalassemia. Hematol Am Soc Hematol Educ Program. 2010;2010:456–62.
Li C, Mathews V, Kim S, George B, Hebert K, Jiang H, et al. Related and unrelated donor transplantation for ß-thalassemia major: results of an international survey. Blood Adv. 2019;3:2562–70.
Angelucci E, Matthes-Martin S, Baronciani D, Bernaudin F, Bonanomi S, Cappellini MD, et al. Hematopoietic stem cell transplantation in thalassemia major and sickle cell disease: indications and management recommendations from an international expert panel. Haematologica. 2014;99:811–20.
La Nasa G, Caocci G, Efficace F, Dessi C, Vacca A, Piras E. Long-term health-related quality of life evaluated more than 20 years after hematopoietic stem cell transplantation for thalassemia. Blood. 2013;122:2262–70.
Chaudhury S, Ayas M, Rosen C, Ma M, Viqaruddin M, Parikh S, et al. A Multicenter Retrospective Analysis stressing the importance of long-term follow-up after Hematopoietic cell transplantation for ß-Thalassemia. Biol Blood Marrow Transpl. 2017;23:1695–700.
Rahal I, Galambrun C, Bertrand Y, Garnier N, Paillard C, Frange P, et al. Late effects after hematopoietic stem cell transplantation for ß-thalassemia major: the French national experience. Haematologica. 2018;103:1143–9.
Caocci G, Orofino MG, Vacca A, Piroddi A, Piras E, Addari MC, et al. Long-term survival of beta thalassemia major patients treated with hematopoietic stem cell transplantation compared with survival with conventional treatment. Am J Hematol. 2017;92:1303–10.
Santarone S, Natale A, Olioso P, Onofrillo D, D’Incecco C, Parruti G, et al. Pregnancy outcome following hematopoietic cell transplantation for thalassemia major. Bone Marrow Transpl. 2017;52:388–93.
Santarone S, Pepe A, Meloni A, Natale A, Pistoia L, Olioso P, et al. Secondary solid cancer following hematopoietic cell transplantation in patients with thalassemia major. Bone Marrow Transpl. 2018;53:39–43.
Di Bartolomeo P, Santarone S, Di Bartolomeo E, Olioso P, Bavaro P, Papalinetti G, et al. Long-term results of survival in patients with thalassemia major treated with bone marrow transplantation. Am J Hematol. 2008;83:528–30.
Ishak K, Baptista A, Bianchi L, Callea F, De Groote J, Gudat F, et al. Histological grading and staging of chronic hepatitis. J Hepatol. 1995;22:696–9.
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA, et al. Clinical manifestations of graft-versus- host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974;18:295–304.
Lee SJ, Vogelsang G, Flowers ME. Chronic graft-versus-host disease. Biol Blood Marrow Transpl. 2003;9:215–33.
Oostdik K, Lenz K, Nye J, Schelling K, Yet D, Bruski S, et al. Developmental validation of the PowerPlex® Fusion System for analysis of casework and reference samples: A 24-locus multiplex for new database standards. Forensic Sci Int Gent. 2014;12:69–76.
European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C: Final update of the series. J Hepatol. 2020;73:1170–218.
Shenoy S, Gaziev J, Angelucci E, King A, Bhatia M, Smith A, et al. Late effects screening guidelines after Hematopoietic Cell Transplantation (HCT) for Hemoglobinopathy: Consensus Statement from the Second Pediatric Blood and Marrow Transplant Consortium International Conference on Late Effects after Pediatric HCT. Biol Blood Marrow Transpl. 2018;24:1313–21.
Galambrun C, Pondarrè C, Bertrand Y, Loundou A, Bordigoni P, Frange P, et al. French Multicenter 22 Year-Experience in Stem cell Transplantation for Beta-Thalassemia Major: Lessons and Future Directions. Biol Blood Marrow Transpl. 2013;19:62–8.
Andreani M, Manna M, Lucarelli G, Tonucci F, Agostinelli F, Ripalti M, et al. Persistence of Mixed Chimerism in Patients Transplanted for the Treatment of Thalassemia. Blood. 1996;87:3494–9.
Fouzia NA, Edison ES, Lakshmi KM, Korula A, Velayudhan SR, Balasubramanian P, et al. Long-term outcome of mixed chimerism after stem cell transplantation for thalassemia major conditioned with busulfan and cyclophosphamide. Bone Marrow Transpl. 2017;53:169–74.
Murdych T, Weisdorf DJ. Serious cardiac complications during bone marrow transplantation at the University of Minnesota, 1977–1997. Bone Marrow Transpl. 2001;28:283–7.
Modell B, Khan M, Darlison M. Survival in ß-thalassemia major in the UK: data from the UK Thalassemia Register. Lancet. 2000;355:2051–2.
Thuret I, Pondarrè C, Loundou A, Steschenko D, Girot R, Bachir D, et al. Complications and treatment of patients with ß-thalassemia in France: results of the National Registry. Haematologica. 2010;95:724–9.
Borgna-Pignatti C, Rugolotto S, De Stefano P, Zhao H, Cappellini MD, Del Vecchio GC, et al. Survival and complications in patients with thalassemia major treated with transfusion and deferoxamine. Haematologica. 2004;89:1187–93.
Neunert C, Terrel DR, Arnold DM, Buchanan G, Cines DB, Cooper N. American Society of Hematology guidelines for immune thrombocytopenia. Blood Adv. 2019;3:3829–66.
Terrel DR, Beebe LA, Vesely SK, Neas BR, Segal JB, George JN. The incidence of immune thrombocytopenic purpura in children and adults: a critical review of published report. Am J Hematol. 2010;85:174–80.
Zufferey A, Kapur R, Semple JW. Pathogenesis and Therapeutic Mechanisms in Immune Thrombocytopenia (ITP). J Clin Med. 2017;6:16–37.
Zanella S, Garani MC, Borgna-Pignatti C. Malignancies and thalassemia: a review of the literature. Ann N. Y Acad Sci. 2016;1368:140–8.
Mikulska M, Knelange N, Nicolini LA, Tridello G, Santarone S, Di Bartolomeo P, et al. Efficacy, safety and feasibility of treatment of chronic HCV infection with directly acting agents in hematopoietic stem cell transplant recipients – Study of infectious disease working party of EBMT. J Infect. 2022;84:71–9.
Acknowledgements
The authors thank all of the patients with their families and the outstanding team at the Bone Marrow Transplant Center, the UOSD Tissue Institute and Bio-Banks and the UOC Transfusion Center of the Department of Oncology Hematology at the Ospedale Civile of Pescara.
Author information
Authors and Affiliations
Contributions
SS, PDB contributed patients, designed the study, analyzed the data, and wrote the manuscript; SA performed statistical study and contributed to the interpretation of the results; AN, DV, RS, PC contributed to data acquisition, analyzed the data, and wrote the paper; FP performed HLA typing and evaluated the chimerism; EDL, GI performed the liver evaluation by transient elastography. All authors read and critically reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Santarone, S., Angelini, S., Natale, A. et al. Survival and late effects of hematopoietic cell transplantation in patients with thalassemia major. Bone Marrow Transplant 57, 1689–1697 (2022). https://doi.org/10.1038/s41409-022-01786-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-022-01786-4
This article is cited by
-
Late renal, liver, endocrine, and cardiac outcomes of bone marrow transplantation in Kurdish children with β-thalassemia major
International Journal of Hematology (2025)
-
Safety and effectiveness of controlled ovarian stimulation and oocyte retrieval during prepubertal and peripubertal period
Journal of Assisted Reproduction and Genetics (2024)