Abstract
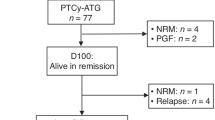
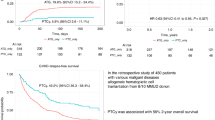
The reduced risk of chronic graft-versus-host-disease (GVHD) with posttransplant cyclophosphamide (ptCy) in the setting of haploidentical related donor and more recently, with HLA-matched related and matched and mismatched unrelated donor allogeneic transplantation has been established. There is, however, paucity of data to show if ptCy impacts chronic GVHD pathogenesis, its phenotype and evolution after HCT regardless of the donor status. We examined the differences in chronic GVHD incidence and presentation in 314 consecutive patients after receiving their first allogeneic transplantation (HCT) using ptCy-based GVHD prophylaxis (ptCy-HCT; n = 120; including 95 with haploidentical related donor) versus conventional calcineurin inhibitor-based prophylaxis (CNI-MUD; n = 194) between 2012 and 2019. The 1-year cumulative incidence of all-grade chronic GVHD and moderate/severe chronic GVHD was 24% and 12%, respectively, after ptCy-HCT and 40% and 23% in the CNI-MUD recipients (p = 0.0003 and 0.007). Multivariable analysis confirmed that use of CNI-based GVHD prophylaxis and peripheral blood stem cell graft as the risk factors for chronic GVHD. The cumulative incidence of visceral (involving ≥1 of the following organs: liver, lungs, gastrointestinal tract, serous membranes) chronic GVHD was significantly higher with CNI-MUD vs. ptCy-HCT (27% vs. 15% at 1 year, p = 0.009). The incidence of moderate/severe visceral chronic GVHD was 20% in CNI-MUD group vs. 7.7% in the ptCy-HCT group at 1 year (p = 0.002). In addition, significantly fewer ptCy-HCT recipients developed severe chronic GVHD in ≥3 organs (0.8%) vs. 8.8% in the CNI-MUD group at 1-year posttransplant (p = 0.004). There was no significant different in relapse, non-relapse mortality, and relapse-free and overall survival between the two groups. Further investigation is needed to confirm that reduced risk and severity of chronic GVHD, less visceral organ distribution with ptCy-HCT leads to improved quality of life.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Luznik L, Fuchs EJ. High-dose, post-transplantation cyclophosphamide to promote graft-host tolerance after allogeneic hematopoietic stem cell transplantation. Immunol Res. 2010;47:65–77.
Robinson TM, O’donnell PV, Fuchs EJ, Luznik L. Haploidentical bone marrow and stem cell transplantation: experience with post-transplantation cyclophosphamide. Semin Hematol. 2016;53:90–7.
Ciurea SO, Zhang M-J, Bacigalupo AA, Bashey A, Appelbaum FR, Aljitawi OS, et al. Haploidentical transplant with posttransplant cyclophosphamide vs matched unrelated donor transplant for acute myeloid leukemia. Blood. 2015;126:1033–40.
Ahmed S, Kanakry JA, Ahn KW, Litovich C, Abdel-Azim H, Aljurf M, et al. Lower graft-versus-host disease and relapse risk in post-transplant cyclophosphamide–based haploidentical versus matched sibling donor reduced-intensity conditioning transplant for Hodgkin lymphoma. Biol Blood Marrow Transplant. 2019;25:1859–68.
Ghosh N, Karmali R, Rocha V, Ahn KW, DiGilio A, Hari PN, et al. Reduced-intensity transplantation for lymphomas using haploidentical related donors versus HLA-matched sibling donors: A center for international blood and marrow transplant research analysis. J Clin Oncol. 2016;34:3141–9.
Kanate AS, Mussetti A, Kharfan-Dabaja MA, Ahn KW, DiGilio A, Beitinjaneh A, et al. Reduced-intensity transplantation for lymphomas using haploidentical related donors vs HLA-matched unrelated donors. Blood. 2016;127:938–47.
Gooptu M, Romee R, St Martin A, Arora M, Al Malki M, Antin JH, et al. HLA-haploidentical vs matched unrelated donor transplants with posttransplant cyclophosphamide-based prophylaxis. Blood. 2021;138:273–82.
Bolaños-Meade J, Hamadani M, Wu J, Al Malki MM, Martens MJ, Runaas L, et al. Post-transplantation cyclophosphamide-based graft-versus-host disease prophylaxis. N Engl J Med. 2023;388:2338–48.
Solh MM, Baron J, Zhang X, Bashey A, Morris LE, Holland HK, et al. Differences in graft-versus-host disease characteristics between haploidentical transplantation using post-transplantation cyclophosphamide and matched unrelated donor transplantation using calcineurin inhibitors. Biol Blood Marrow Transplant. 2020;26:2082–8.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M, et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the Center for international blood and marrow transplant research. Biol Blood Marrow Transplant. 2009;15:367–9.
Raj RV, Hamadani M, Szabo A, Pasquini MC, Shah NN, Drobyski WR, et al. Peripheral blood grafts for T cell-replete haploidentical transplantation increase the incidence and severity of cytokine release syndrome. Biol Blood Marrow Transpl. 2018;24:1664–70.
Raj RV, Hari P, Pasquini M, Epperla N, D’Souza A, Fenske T, et al. Impact of haploidentical hematopoietic cell transplantation conditioning intensity on the incidence and severity of post-transplantation viral infections. Bone Marrow Transpl. 2016;51:1602–4.
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 Diagnosis and Staging Working Group report. Biol Blood Marrow Transplant. 2015;21:389–401.e1.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant. 1995;15:825–8.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9.
Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME, et al. Validation and refinement of the Disease Risk Index for allogeneic stem cell transplantation. Blood. 2014;123:3664–71.
Kanakry CG, Bolaños-Meade J, Kasamon YL, Zahurak M, Durakovic N, Furlong T, et al. Low immunosuppressive burden after HLA-matched related or unrelated BMT using posttransplantation cyclophosphamide. Blood. 2017;129:1389–93.
Kanakry CG, O’donnell PV, Furlong T, de Lima MJ, Wei W, Medeot M, et al. Multi-institutional study of post-transplantation cyclophosphamide as single-agent graft-versus-host disease prophylaxis after allogeneic bone marrow transplantation using myeloablative busulfan and fludarabine conditioning. J Clin Oncol. 2014;32:3497–505.
Luznik L, Bolaños-Meade J, Zahurak M, Chen AR, Smith BD, Brodsky R, et al. High-dose cyclophosphamide as single-agent, short-course prophylaxis of graft-versus-host disease. Blood. 2010;115:3224–30.
Saliba RM, Alousi AM, Pidala J, Arora M, Spellman SR, Hemmer MT, et al. Characteristics of Graft-Versus-Host Disease (GvHD) After Post-Transplantation Cyclophosphamide Versus Conventional GvHD Prophylaxis. Transplant Cell Ther. 2022;28:681–93.
Luznik L, O’donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14:641–50.
Dreger P, Sureda A, Ahn KW, Eapen M, Litovich C, Finel H, et al. PTCy-based haploidentical vs matched related or unrelated donor reduced-intensity conditioning transplant for DLBCL. Blood Adv. 2019;3:360–9.
Solh M, Zhang X, Connor K, Brown S, Solomon SR, Morris LE, et al. Factors predicting graft-versus-host disease–free, relapse-free survival after allogeneic hematopoietic cell transplantation: multivariable analysis from a single center. Biol Blood Marrow Transplant. 2016;22:1403–9.
Brunstein CG, Fuchs EJ, Carter SL, Karanes C, Costa LJ, Wu J, et al. Alternative donor transplantation after reduced intensity conditioning: results of parallel phase 2 trials using partially HLA-mismatched related bone marrow or unrelated double umbilical cord blood grafts. Blood. 2011;118:282–8.
Rashidi A, Hamadani M, Zhang M-J, Wang HL, Abdel-Azim H, Aljurf M, et al. Outcomes of haploidentical vs matched sibling transplantation for acute myeloid leukemia in first complete remission. Blood Adv. 2019;3:1826–36.
Shaw BE, Jimenez-Jimenez AM, Burns LJ, Logan BR, Khimani F, Shaffer BC, et al. National marrow donor program-sponsored multicenter, phase II trial of HLA-mismatched unrelated donor bone marrow transplantation using post-transplant cyclophosphamide. J Clin Oncol. 2021;39:1971–82.
Bolaños-Meade J, Reshef R, Fraser R, Fei M, Abhyankar S, Al-Kadhimi Z, et al. Three prophylaxis regimens (tacrolimus, mycophenolate mofetil, and cyclophosphamide; tacrolimus, methotrexate, and bortezomib; or tacrolimus, methotrexate, and maraviroc) versus tacrolimus and methotrexate for prevention of graft-versus-host disease with haemopoietic cell transplantation with reduced-intensity conditioning: a randomised phase 2 trial with a non-randomised contemporaneous control group (BMT CTN 1203). Lancet Haematol. 2019;6:e132–43.
Broers AEC, de Jong CN, Bakunina K, Hazenberg MD, van Marwijk Kooy M, de Groot MR, et al. Posttransplant cyclophosphamide for prevention of graft-versus-host disease: results of the prospective randomized HOVON-96 trial. Blood Adv. 2022;6:3378–85.
Im A, Rashidi A, Wang T, Hemmer M, MacMillan ML, Pidala J, et al. Risk factors for graft-versus-host disease in haploidentical hematopoietic cell transplantation using post-transplant cyclophosphamide. Biol Blood Marrow Transplant. 2020;26:1459–68.
Zeiser R, von Bubnoff N, Butler J, Mohty M, Niederwieser D, Or R, et al. Ruxolitinib for glucocorticoid-refractory acute graft-versus-host disease. N Engl J Med. 2020;382:1800–10.
Cutler C, Lee SJ, Arai S, Rotta M, Zoghi B, Lazaryan A, et al. Belumosudil for chronic graft-versus-host disease after 2 or more prior lines of therapy: the ROCKstar Study. Blood. 2021;138:2278–89.
Author information
Authors and Affiliations
Contributions
SC, JJ, AS, and MH designed the study. KM and JJ acquired the data. SC, JJ, KM, AS, and MH analyzed and interpreted the data. SC and JJ drafted the manuscript. All authors reviewed, critically revised and approved the final manuscript. SC and JJ contributed equally as primary co-authors of the manuscript.
Corresponding author
Ethics declarations
Competing interests
SC: Honorarium from Janssen, Sanofi, GSK, and institutional research funding from Janssen, Takda, C4 Therapeutics, Abbvie. JHJ: Honorarium from Omeros. SA: Research Funding from Incyte, AltruBio, Actinium Pharmaceutical; Consultancy/Honoraria from AbbVie, Daichii Sankyo, Servier. NNS: Participation on advisory boards and/or consultancy for Kite Pharma, BMS-Juno, Miltenyi Biotec, Lilly Oncology, Epizyme, Incyte, Novartis, Seattle Genetics, Abbvie, and Gallapagos; Research funding, travel support, and honoraria from Lilly Oncology and Miltenyi Biotec; Scientific advisory board for Tundra Therapeutics. TSF: Consultancy, Speakers Bureau: Beigene, Kite (Gilead), Servier Pharmaceuticals, MorphoSys, TG Therapeutics, SeaGen, Adaptive Biotechnologies, Astrazeneca, Pharmacyclics (AbbVie), Sanofi. MCP: Research Funding: Novartis, Bristol Myers Squibb, Kite, a Gilead Company, Janssen; Consultancy: Bristol Myers Squibb; Honoraria: Kite, a Gilead Company, Kite Brazil. BES: Institutional payments from Mallinkrodt, Orcabio. AD: Membership on an entity’s Board of Directors or advisory committees: Imbrium, Pfizer; Consultancy: Bristol Myers Squibb; Janssen, Prothena; Research Funding: Abbvie, Sanofi, Takeda, TeneoBio, Caelum, Prothena. MM: Honoraria: MashupMD, Blood Cancer Today, MJH life sciences, Bristol-Myers Squibb Company; Consultancy: Sanofi S.A; Research Funding: Sanofi. S.A, Amgen Inc, Institutional KL2 Award, Celgene Corporation, Ionis Pharmaceuticals, Takeda Pharmaceutical Company, GlaxoSmithKline plc, Novartis. MH: Research Support/Funding: ADC Therapeutics; Spectrum Pharmaceuticals; Astellas Pharma. Consultancy: ADC Therapeutics, Omeros, CRISPR, BMS, Kite, Abbvie, Caribou, Genmab. Speaker’s Bureau: Sanofi Genzyme., ADC Therapeutics, AstraZeneca, BeiGene, Kite. DMC: Inc, Genentech, Myeloid Therapeutics, CRISPR. All other authors report no relevant conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chhabra, S., Jerkins, J.H., Monahan, K. et al. Severity and organ distribution of chronic graft-versus-host disease with posttransplant cyclophosphamide-based versus methotrexate/calcineurin inhibitor-based allogeneic hematopoietic cell transplantation. Bone Marrow Transplant 59, 373–379 (2024). https://doi.org/10.1038/s41409-023-02178-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-023-02178-y
This article is cited by
-
Current therapeutics for sclerotic and fibrotic manifestations of chronic graft-versus-host disease
Bone Marrow Transplantation (2025)