Abstract
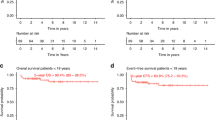
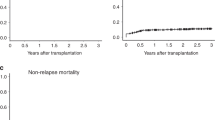
Prognosis for patients undergoing hematopoietic cell transplantation (HCT) has been improving. Short-term survival information, such as crude survival rates that consider deaths immediately after the transplantation, may not be sufficiently useful for assessing long-term survival. Using the data of the Japanese HCT registry, the net survival rate of patients who survived for a given period was determined according to age, disease, and type of transplant. We included a total of 41,716 patients who received their first allogeneic hematopoietic cell transplantation between 1991 and 2015. For each disease, age group, graft source subcategory, net survival was calculated using the Pohar-Perme method, and 5-year conditional net survival (CS) was calculated. Ten-year net survivals of total patient cohort were 41.5% and 47.4% for males and females, respectively. Except for myelodysplastic syndrome, multiple myeloma, and adult T-cell leukemia/lymphoma, 5-year CS for 5-year transplant survivors exceeded 90%. CS was especially high for aplastic anemia, of which was over 100% for children and younger adults receiving cord blood, suggesting that these patients have similar longevity to an equivalent group from the general population. These findings provide useful information for long-term survival, and can serve as benchmark for comparisons among registries, including other cancers.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to ethical restrictions that it exceeds the scope of the recipient/donor’s consent for research use in the registry but are available from the corresponding author on reasonable request and with permission of the JSTCT/JDCHCT.
References
Bhatia S, Dai C, Landier W, Hageman L, Wu J, Schlichting E, et al. Trends in late mortality and life expectancy after allogeneic blood or marrow transplantation over 4 decades: a blood or marrow transplant survivor study report. JAMA Oncol. 2021;7:1626–34.
Tanaka Y, Kurosawa S, Tajima K, Tanaka T, Ito R, Inoue Y, et al. Analysis of non-relapse mortality and causes of death over 15 years following allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2016;51:553–9.
Konuma T, Mizuno S, Kondo T, Arai Y, Uchida N, Takahashi S, et al. Improved trends in survival and engraftment after single cord blood transplantation for adult acute myeloid leukemia. Blood Cancer J. 2022;12:81.
Yanada M, Masuko M, Mori J, Aoki J, Mizuno S, Fukuda T, et al. Patients with acute myeloid leukemia undergoing allogeneic hematopoietic cell transplantation: trends in survival during the past two decades. Bone Marrow Transplant. 2019;54:578–86.
Konuma T, Itonaga H, Ishiyama K, Hamamura A, Uchida N, Ozawa Y, et al. Progress in survival following three decades of allogeneic hematopoietic cell transplantation for myelodysplastic syndrome: a real-world registry study in Japan. Am J Hematol. 2023;98:E68–71.
Shouval R, Fein JA, Labopin M, Kroger N, Duarte RF, Bader P, et al. Outcomes of allogeneic haematopoietic stem cell transplantation from HLA-matched and alternative donors: a European Society for Blood and Marrow Transplantation registry retrospective analysis. Lancet Haematol. 2019;6:e573–84.
Ohbiki M, Ito Y, Inamoto Y, Miyamura K, Uchida N, Fukuda T, et al. Improved long-term net survival after allogeneic hematopoietic cell transplantation in patients with hematologic malignancies over two decades. Transpl Cell Ther. 2023;29:768.e761–10.
Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med. 2006;354:1813–26.
Hori M, Matsuda T, Shibata A, Katanoda K, Sobue T, Nishimoto H, et al. Cancer incidence and incidence rates in Japan in 2009: a study of 32 population-based cancer registries for the Monitoring of Cancer Incidence in Japan (MCIJ) project. Jpn J Clin Oncol. 2015;45:884–91.
Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Niksic M, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–75.
Ito Y, Miyashiro I, Ito H, Hosono S, Chihara D, Nakata-Yamada K, et al. Long-term survival and conditional survival of cancer patients in Japan using population-based cancer registry data. Cancer Sci. 2014;105:1480–6.
Okuyama A, Shibata A, Nishimoto H. Critical points for interpreting patients’ survival rate using cancer registries: a literature review. J Epidemiol. 2018;28:61–6.
Pohar Perme M, Esteve J, Rachet B. Analysing population-based cancer survival—settling the controversies. BMC Cancer. 2016;16:933.
Roche L, Danieli C, Belot A, Grosclaude P, Bouvier AM, Velten M, et al. Cancer net survival on registry data: use of the new unbiased Pohar-Perme estimator and magnitude of the bias with the classical methods. Int J Cancer. 2013;132:2359–69.
Atsuta Y, Hirakawa A, Nakasone H, Kurosawa S, Oshima K, Sakai R, et al. Late mortality and causes of death among long-term survivors after allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2016;22:1702–9.
Kliman D, Nivison-Smith I, Gottlieb D, Hamad N, Kerridge I, Purtill D, et al. Hematopoietic stem cell transplant recipients surviving at least 2 years from transplant have survival rates approaching population levels in the modern era of transplantation. Biol Blood Marrow Transplant. 2020;26:1711–8.
Vanderwalde AM, Sun CL, Laddaran L, Francisco L, Armenian S, Berano-Teh J, et al. Conditional survival and cause-specific mortality after autologous hematopoietic cell transplantation for hematological malignancies. Leukemia. 2013;27:1139–45.
Smeland KB, Kiserud CE, Lauritzsen GF, Fagerli UM, Falk RS, Fluge O, et al. Conditional survival and excess mortality after high-dose therapy with autologous stem cell transplantation for adult refractory or relapsed Hodgkin lymphoma in Norway. Haematologica. 2015;100:e240–3.
Klein JP, Rizzo JD, Zhang MJ, Keiding N. Statistical methods for the analysis and presentation of the results of bone marrow transplants. Part I: unadjusted analysis. Bone Marrow Transplant. 2001;28:909–15.
Wingard JR, Majhail NS, Brazauskas R, Wang Z, Sobocinski KA, Jacobsohn D, et al. Long-term survival and late deaths after allogeneic hematopoietic cell transplantation. J Clin Oncol. 2011;29:2230–9.
Assouline S, Li S, Gisselbrecht C, Fogarty P, Hay A, van den Neste E, et al. The conditional survival analysis of relapsed DLBCL after autologous transplant: a subgroup analysis of LY.12 and CORAL. Blood Adv. 2020;4:2011–7.
Abdallah NH, Smith AN, Geyer S, Binder M, Greipp PT, Kapoor P, et al. Conditional survival in multiple myeloma and impact of prognostic factors over time. Blood Cancer J. 2023;13:78.
Anasetti C, Logan BR, Lee SJ, Waller EK, Weisdorf DJ, Wingard JR, et al. Peripheral-blood stem cells versus bone marrow from unrelated donors. N Engl J Med. 2012;367:1487–96.
Jo T, Arai Y, Kondo T, Mizuno S, Hirabayashi S, Inamoto Y, et al. Advantages of peripheral blood stem cells from unrelated donors versus bone marrow transplants in outcomes of adult acute myeloid leukemia patients. Cytotherapy. 2022;24:1013–25.
Kuwatsuka Y, Kanda J, Yamazaki H, Mori T, Miyamura K, Kako S, et al. A comparison of outcomes for cord blood transplantation and unrelated bone marrow transplantation in adult aplastic anemia. Biol Blood Marrow Transplant. 2016;22:1836–43.
Smith AR, Wagner JE. Alternative haematopoietic stem cell sources for transplantation: place of umbilical cord blood. Br J Haematol. 2009;147:246–61.
Nagamine CML, Goulart BNG, Ziegelmann PK. Net survival in survival analyses for patients with cancer: a scoping review. Cancers. 2022;14:3304.
Atsuta Y. Introduction of transplant registry unified management program 2 (TRUMP2): scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int J Hematol. 2016;103:3–10.
Kanda J. Scripts for TRUMP data analyses. Part II (HLA-related data): statistical analyses specific for hematopoietic stem cell transplantation. Int J Hematol. 2016;103:11–19.
Kuwatsuka Y. Quality control and assurance in hematopoietic stem cell transplantation data registries in Japan and other countries. Int J Hematol. 2016;103:20–24.
Atsuta Y, Suzuki R, Yoshimi A, Gondo H, Tanaka J, Hiraoka A, et al. Unification of hematopoietic stem cell transplantation registries in Japan and establishment of the TRUMP System. Int J Hematol. 2007;86:269–74.
Atsuta Y. [The Japanese Transplant Registry Unified Management Program (TRUMP((R))): current issues and the future]. [Rinsho ketsueki] Jpn J Clin Hematol. 2020;61:387–91.
Ssenyonga, Stiller N, Nakata KC, Shalkow J, Redmond S, Bulliard JL, et al. Worldwide trends in population-based survival for children, adolescents, and young adults diagnosed with leukaemia, by subtype, during 2000-14 (CONCORD-3): analysis of individual data from 258 cancer registries in 61 countries. Lancet Child Adolesc Health. 2022;6:409–31.
Perme MP, Stare J, Esteve J. On estimation in relative survival. Biometrics. 2012;68:113–20.
National Cancer Center. Cancer Registry and Statistics, Cancer Information Service, National Cancer Center, Japan. Cohort Life Table. 2018. https://ganjoho.jp/reg_stat/statistics/qa_words/cohort01.html.
Clark TG, Altman DG, De Stavola BL. Quantification of the completeness of follow-up. Lancet. 2002;359:1309–10.
Snowden JA, Saccardi R, Orchard K, Ljungman P, Duarte RF, Labopin M, et al. Benchmarking of survival outcomes following haematopoietic stem cell transplantation: a review of existing processes and the introduction of an international system from the European Society for Blood and Marrow Transplantation (EBMT) and the Joint Accreditation Committee of ISCT and EBMT (JACIE). Bone Marrow Transplant. 2020;55:681–94.
Schrezenmeier H, Passweg JR, Marsh JC, Bacigalupo A, Bredeson CN, Bullorsky E, et al. Worse outcome and more chronic GVHD with peripheral blood progenitor cells than bone marrow in HLA-matched sibling donor transplants for young patients with severe acquired aplastic anemia. Blood. 2007;110:1397–400.
Bacigalupo A, Socie G, Schrezenmeier H, Tichelli A, Locasciulli A, Fuehrer M, et al. Bone marrow versus peripheral blood as the stem cell source for sibling transplants in acquired aplastic anemia: survival advantage for bone marrow in all age groups. Haematologica. 2012;97:1142–8.
Alousi A, Wang T, Hemmer MT, Spellman SR, Arora M, Couriel DR, et al. Peripheral blood versus bone marrow from unrelated donors: bone marrow allografts have improved long-term overall and graft-versus-host disease-free, relapse-free survival. Biol Blood Marrow Transplant. 2019;25:270–8.
Kanda J, Hayashi H, Ruggeri A, Kimura F, Volt F, Takahashi S, et al. The impact of GVHD on outcomes after adult single cord blood transplantation in European and Japanese populations. Bone Marrow Transplant. 2022;57:57–64.
Tsugane S. Why has Japan become the world’s most long-lived country: insights from a food and nutrition perspective. Eur J Clin Nutr. 2021;75:921–8.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128.
Acknowledgements
The authors thank the physicians and staff at the transplant centers for providing clinical data to the registry. They also thank the staff at the JDCHCT for data management. This study was funded in part by JSPS KAKENHI Grant Numbers 17K08911 and 22K10360 from the Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Contributions
YK, HI, KT, TK, FK, JK, YA and KM designed the research and contributed to critical review of the manuscript. YK, HI, YA and KM analyzed data, YK performed statistical analysis and wrote the first draft of the manuscript. All the other authors contributed to data collection. All authors approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kuwatsuka, Y., Ito, H., Tabuchi, K. et al. Trends in allogeneic hematopoietic cell transplantation survival using population-based descriptive epidemiology method: analysis of national transplant registry data. Bone Marrow Transplant 59, 1295–1301 (2024). https://doi.org/10.1038/s41409-024-02326-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-024-02326-y