Abstract
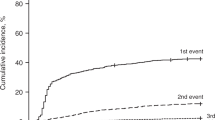
Bacterial bloodstream infections (BSI) can be a substantial contributor to complications of GVHD treatment. The aim of this study was to determine the risk for BSI from neutrophil engraftment through day 100 post transplant in patients with acute GVHD (AGVHD) based on organ involvement and severity. Patients (n = 4064) who underwent an allogeneic hematopoietic stem cell transplant (HCT) reported to the CIBMTR registry were analyzed. Grade II-IV AGVHD occurred in 1607 (39.5%) patients and was associated with a greater day-100 incidence of post engraftment BSI than with grade 0/I (24.9 vs. 15.3%). Patients with grade III/IV AGVHD had the highest BSI risk (HR 2.45; 95% CI 1.99–3.0; p < 0.0001). Lower GI involvement increased BSI risk (HR 1.54; 95% CI 1.17–2.02; p = 0.0019). BSI post-engraftment through day 100 was associated with worse survival (HR 1.64, 95% CI 1.43–1.87; p < 0.001) and higher non-relapse mortality (NRM), (HR 2.22; 95% CI 1.91–2.59; p < 0.001). Those with stage III/IV GI involvement are at highest risk for BSI. Future studies evaluating novel methods for preventing BSI in these high risk populations are needed to reduce mortality associated with AGVHD.
Highlights
-
Bacterial blood stream infections are more common in patients with Grade II-IV AGVHD with roughly 25% of these patients developing at least one BSI by day-100.
-
Patients with grade III/IV AGVHD and those with lower gastrointestinal involvement are at the highest risk for BSI.
-
Patients who experience a BSI by day 100 have worse survival and over a two-fold higher probability for non-relapse mortality.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The final analysis dataset will be posted to the CIBMTR website at: https://cibmtr.org/CIBMTR/Resources/Publicly-Available-Datasets#.
References
Cusatis R, Litovich C, Feng Z, Allbee-Johnson M, Kapfhammer M, Mattila D, et al. Current trends and outcomes in cellular therapy activity in the United States, including prospective Patient Reported Outcomes data collection within the CIBMTR registry. Transplant Cell Ther. 2024;24:S2666–6367.
Daly A, McAfee S, Dey B, Colby C, Schulte L, Yeap B, et al. Nonmyeloablative bone marrow transplantation: Infectious complications in 65 recipients of HLA-identical and mismatched transplants. Biol Blood Marrow Transpl. 2003;9:373–82.
Cappellano P, Viscoli C, Bruzzi P, Van Lint MT, Pereira CAP, Bacigalupo A. Epidemiology and risk factors for bloodstream infections after allogeneic hematopoietic stem cell transplantion. N Microbiol. 2007;30:89–99.
Miller HK, Braun TM, Stillwell T, Harris AC, Choi S, Connelly J, et al. Infectious risk after allogeneic hematopoietic cell transplantation complicated by acute graft-versus-host disease. Biol Blood Marrow Transpl. 2017;23:522–8.
Tomblyn M, Chiller T, Einsele H, Gress R, Sepkowitz K, Storek J. et al. Guidelines for preventing infectious complications among hematopoietic cell transplant recipients: a global perspective. Preface Bone Marrow Transpl. 2009;44:453–5.
Mori Y, Yoshimoto G, Nishida R, Sugio T, Miyawaki K, Shima T, et al. Gastrointestinal graft-versus-host disease is a risk factor for postengraftment bloodstream infection in allogeneic hematopoietic stem cell transplant recipients. Biol Blood Marrow Transpl. 2018;24:2302–9.
Inoue Y, Okinaka K, Fuji S, Inamoto Y, Uchida N, Toya T, et al. Severe acute graft-versus-host disease increases the incidence of blood stream infection and mortality after allogeneic hematopoietic cell transplantation: Japanese transplant registry study. Bone Marrow Transpl. 2021;56:2125–36.
Modi A, Rybicki L, Majhail NS, Mossad SB. Severity of acute gastrointestinal graft-vs-host disease is associated with incidence of bloodstream infection after adult allogeneic hematopoietic stem cell transplantation. Transpl Infect Dis. 2020;22:e13217.
Levinson A, Pinkney K, Jin Z, Bhatia M, Kung AL, Foca MD, et al. Acute gastrointestinal graft-vs-host disease is associated with increased enteric bacterial bloodstream infection density in pediatric allogeneic hematopoietic cell transplant recipients. Clin Infect Dis. 2015;61:350–7.
Sepkowitz KA. Antibiotic prophylaxis in patients receiving hematopoietic stem cell transplant. Bone Marrow Transpl. 2002;29:367–71.
Averbuch D, Tridello G, Hoek J, Mikulska M, Akan H, Yanez San Segundo L, et al. Antimicrobial resistance in gram-negative rods causing bacteremia in hematopoietic stem cell transplant recipients: intercontinental prospective study of the infectious diseases working party of the European bone marrow transplantation group. Clin Infect Dis. 2017;65:1819–28.
Macesic N, Morrissey CO, Cheng AC, Spencer A, Peleg AY. Changing microbial epidemiology in hematopoietic stem cell transplant recipients: increasing resistance over a 9-year period. Transpl Infect Dis. 2014;16:887–96.
Hauck CG, Chong PP, Miller MB, Jamieson K, Fine JP, Foster MC, et al. Increasing rates of fluoroquinolone resistance in Escherichia coli isolated from the blood and urine of patients with hematologic malignancies and stem cell transplant recipients. Pathog Immun. 2016;1:234–42.
Jenq RR, Taur Y, Devlin SM, Ponce DM, Goldberg JD, Ahr KF, et al. Intestinal blautia is associated with reduced death from graft-versus-host disease. Biol Blood Marrow Transpl. 2015;21:1373–83.
Weber D, Hiergeist A, Weber M, Dettmer K, Wolff D, Hahn J, et al. Detrimental effect of broad-spectrum antibiotics on intestinal microbiome diversity in patients after allogeneic stem cell transplantation: lack of commensal sparing antibiotics. Clin Infect Dis. 2019;68:1303–10.
Weber D, Jenq RR, Peled JU, Taur Y, Hiergeist A, Koestler J, et al. Microbiota disruption induced by early use of broad-spectrum antibiotics is an independent risk factor of outcome after allogeneic stem cell transplantation. Biol Blood Marrow Transpl. 2017;23:845–52.
Lee S-E, Lim J-Y, Ryu D-B, Kim TW, Park SS, Jeon YW, et al. Alteration of the intestinal microbiota by broad-spectrum antibiotic use correlates with the occurrence of intestinal graft-versus-host disease. Biol Blood Marrow Transpl. 2019;25:1933–43.
Taur Y, Xavier JB, Lipuma L, Ubeda C, Goldberg J, Gobourne A, et al. Intestinal domination and the risk of bacteremia in patients undergoing allogeneic hematopoietic stem cell transplantation. Clin Infect Dis. 2012;55:905–14.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transpl. 1995;15:825–8.
Button JE, Autran CA, Reens AL, Cosetta CM, Smriga S, Ericson M, et al. Dosing a synbiotic of human milk lligosaccharides and B. infantis leads to reversible engraftment in healthy adult microbiomes without antibiotics. Cell Host Microbe. 2022;30:712–25.
Šuligoj T, Vigsnaes LK, Abbeele PVD, Apostolou A, Karalis K, Savva GM, et al. Effects of human milk oilgosaccarides on the adult gut microbiota and barrier function. effects of human milk oligosaccharides on the adult gut microbiota and barrier function. Nutrients. 2020;12:2808.
Funding
The CIBMTR is supported primarily by the Public Health Service U24CA076518 from the National Cancer Institute (NCI), the National Heart, Lung and Blood Institute (NHLBI) and the National Institute of Allergy and Infectious Diseases (NIAID); 75R60222C00011 from the Health Resources and Services Administration (HRSA); N00014-23-1-2057 from the Office of Naval Research; Support is also provided by Be the Match Foundation, the Medical College of Wisconsin, the National Marrow Donor Program, Gateway for Cancer Research, Pediatric Transplantation and Cellular Therapy Consortium and from the following commercial entities: AbbVie; Actinium Pharmaceuticals, Inc.; Adaptive Biotechnologies Corporation; ADC Therapeutics; Adienne SA; Alexion; Allogene; AlloVir, Inc.; Amgen, Inc.; Astellas Pharma US; AstraZeneca; Atara Biotherapeutics; BeiGene; BioLineRX; Blue Spark Technologies; bluebird bio, inc.; Blueprint Medicines; Bristol Myers Squibb Co.; CareDx Inc.; CSL Behring; CytoSen Therapeutics, Inc.; DKMS; Eurofins Viracor, DBA Eurofins Transplant Diagnostics; Gamida-Cell, Ltd.; Gift of Life Biologics; Gift of Life Marrow Registry; GlaxoSmithKline; HistoGenetics; Incyte Corporation; Iovance; Janssen Research & Development, LLC; Janssen/Johnson & Johnson; Jasper Therapeutics; Jazz Pharmaceuticals, Inc.; Karius; Kashi Clinical Laboratories; Kiadis Pharma; Kite, a Gilead Company; Kyowa Kirin; Labcorp; Legend Biotech; Mallinckrodt Pharmaceuticals; Med Learning Group; Merck & Co.; Mesoblast; Millennium, the Takeda Oncology Co.; Miller Pharmacal Group, Inc.; Miltenyi Biotec, Inc.; MorphoSys; MSA-EDITLife; Neovii Pharmaceuticals AG; Novartis Pharmaceuticals Corporation; Omeros Corporation; OptumHealth; Orca Biosystems, Inc.; OriGen BioMedical; Ossium Health, Inc.; Pfizer, Inc.; Pharmacyclics, LLC, An AbbVie Company; PPD Development, LP; REGiMMUNE; Registry Partners; Rigel Pharmaceuticals; Sanofi; Sarah Cannon; Seagen Inc.; Sobi, Inc.; Stemcell Technologies; Stemline Technologies; STEMSOFT; Takeda Pharmaceuticals; Talaris Therapeutics; Vertex Pharmaceuticals; Vor Biopharma Inc.; WellSky; Xenikos BV.
Author information
Authors and Affiliations
Contributions
Conceptions and study design (WW, AMG, TW, SRS, AMA), Statistical analysis (TW), Drafting the manuscript (WW, AMA), Interpreting results and revising the manuscript (all authors).
Corresponding author
Ethics declarations
Competing interests
Dr. C Lee reports advisory board participation for Sanofi, Kite, Kadmon, BMS, and Incyte; research funding from Incyte; steering board committee participation for Incyte; speakers panel participation for Kite; and consulting for Fresenius Kabi, Sanofi, and Mallinckrodt. Dr. Sharma reports Grant funds from CRISPR Therapeutics; Consulting fees from Spotlight Therapeutics, Medexus Inc., Vertex Pharmaceuticals, Sangamo Therapeutics and Editas Medicine; and is the St. Jude Children’s Research Hospital site principal investigator of clinical trials for genome editing of sickle cell disease sponsored by Vertex Pharmaceuticals/CRISPR Therapeutics (NCT03745287), Novartis Pharmaceuticals (NCT04443907) and Beam Therapeutics (NCT05456880). The industry sponsors provide funding for the clinical trial, which includes salary support paid to Dr. Sharma’s institution. Dr. Sharma has no direct financial interest in these therapies. Dr. Nishihori reports significant payments (research support) to the institution for clinical trial (Novartis), research support (drug supply only) to the institution for clinical trial (Karyopharm) and advisory board participation for Medexus. Dr. Kitko reports compensation for ad board for Horizon Therapeutics and Incyte and compensation for participation in CME lectures about GVHD for Sanofi, Physicians Education Resource and i3Health. Dr. Pidala reports consulting and advisory board membership for Syndax, CTI Biopharma, Amgen, Regeneron, and Incyte; and clinical trial support for Novartis, Amgen, Takeda, Janssen, Johnson and Johnson, Pharmacyclics, Abbvie, CTI Biopharma, and BMS. Dr. S Lee reports compensation (research funding) from Amgen, AstraZeneca, Incyte, Kadmon, Pfizer, Syndax; steering committee participation for Incyte; drug supply for Janssen; consulting for Mallinckrodt, Equillium, Kadmon, Novartis and Sanofi; and National Marrow Donor Program Board of Directors (uncompensated). All other authors declare no competing interests.
Ethics approval and consent to participate
This study was approved the NMDP Institutional Review Board, registration number IRB00001253. All patients provided written informed consent for research participation and data submission, in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wallis, W., Gulbis, A.M., Wang, T. et al. Incidence of bacterial blood stream infections in patients with acute GVHD. Bone Marrow Transplant 60, 52–57 (2025). https://doi.org/10.1038/s41409-024-02426-9
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41409-024-02426-9