Abstract
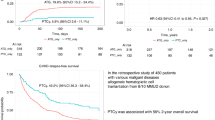
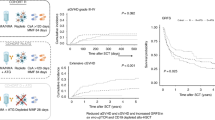
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) utilizing mismatched unrelated donors (MMUD) present a vital option for patients with hematologic malignancies without human leukocyte antigen (HLA)-matched donors. This multicenter retrospective study encompassed 211 adults with hematological malignancies receiving allo-HSCT with antithymocyte globulin (ATG) from ≥1 HLA locus MMUD. The findings revealed cumulative incidences of II-IV acute graft-versus-host disease (GVHD) at 180 days at 26.5%, and III-IV acute GVHD at 12.3%, with 3-year cumulative incidences for total and moderate-severe chronic GVHD at 37.0% and 21.0%. The 3-year non-relapse mortality (NRM) and relapse rates were 19.7% and 25.8%. The study reported a 3-year overall survival (OS) rate of 63.1%, a disease-free survival (DFS) rate of 54.5%, and a GVHD-free, relapse-free survival (GRFS) rate of 40.8%. Administration of a lower-dose ATG-Genzyme (ATG-G, ≤ 6 mg/kg) correlated with improved engraftment without significantly affecting survival, relapse, or viral reactivation rates. The quantity of HLA mismatches did not impact engraftment, GVHD, viral reactivation, OS, DFS, GRFS, relapse, or NRM. In conclusion, MMUD allo-HSCT with ATG demonstrates favorable outcomes for patients with hematological malignancies, with no evident correlation between the degree of mismatch and post-transplantation results. Utilizing a lower dose of ATG-G ( ≤ 6 mg/kg) proved efficacious, delivering comparable clinical advantage.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data available on request from the authors.
References
Shouval R, Fein JA, Labopin M, Kröger N, Duarte RF, Bader P, et al. Outcomes of allogeneic haematopoietic stem cell transplantation from HLA-matched and alternative donors: a European Society for Blood and Marrow Transplantation registry retrospective analysis. Lancet Haematol. 2019;6:e573–e584. https://doi.org/10.1016/s2352-3026(19)30158-9. e-pub ahead of print 2019/09/04
Petersdorf EW. Mismatched unrelated donor transplantation. Semin Hematol. 2016;53:230–6. https://doi.org/10.1053/j.seminhematol.2016.07.003. e-pub ahead of print 2016/10/30
Hwang WY, Kongtim P, Majhail NS, Yao M. Alternate Donor Transplantation. Blood cell Ther. 2022;5:S6–s14. https://doi.org/10.31547/bct-2022-012. e-pub ahead of print 2023/05/23
Mushtaq MU, Shahzad M, Tariq E, Iqbal Q, Chaudhary SG, Zafar MU, et al. Outcomes with mismatched unrelated donor allogeneic hematopoietic stem cell transplantation in adults: A systematic review and meta-analysis. Front Oncol. 2022;12:1005042. https://doi.org/10.3389/fonc.2022.1005042. e-pub ahead of print 2022/10/25
Nagler A, Dholaria B, Labopin M, Bruno B, Rambaldi A, Pioltelli P, et al. The outcome of two or more HLA loci mismatched unrelated donor hematopoietic cell transplantation for acute leukemia: an ALWP of the EBMT study. Bone Marrow Transpl. 2021;56:20–29. https://doi.org/10.1038/s41409-020-0974-6. e-pub ahead of print 2020/06/21
Kato I, Sakaguchi H, Kato S, Sato M, Noguchi M, Yoshida N, et al. Impact of human leukocyte antigen mismatch on outcomes after unrelated bone marrow transplantation in paediatric patients: A retrospective analysis by the JSTCT HLA working group. Br J Haematol. 2022;199:392–400. https://doi.org/10.1111/bjh.18425. e-pub ahead of print 2022/08/28
Crocchiolo R, Rombolà G. Human Leucocyte Antigen System and Selection of Unrelated Hematopoietic Stem Cell Donors: Impact of Patient-Donor (Mis)matching and New Challenges with the Current Technologies. J Clin Med 2023;12. https://doi.org/10.3390/jcm12020646. e-pub ahead of print 2023/01/22
Arslan S, Al Malki MM. New strategies for mismatched unrelated donor (MMUD) hematopoietic cell transplant (HCT). Hematol Am Soc Hematol Educ Program. 2022;2022:74–82. https://doi.org/10.1182/hematology.2022000398. e-pub ahead of print 2022/12/10
Kawamura K. Effect of antithymocyte globulin on HLA-mismatched unrelated transplantation. Int J Hematol. 2019;110:22–9. https://doi.org/10.1007/s12185-019-02597-y. e-pub ahead of print 2019/01/27
Shaw BE, Jimenez-Jimenez AM, Burns LJ, Logan BR, Khimani F, Shaffer BC, et al. National Marrow Donor Program-Sponsored Multicenter, Phase II Trial of HLA-Mismatched Unrelated Donor Bone Marrow Transplantation Using Post-Transplant Cyclophosphamide. J Clin Oncol: Off J Am Soc Clin Oncol. 2021;39:1971–82. https://doi.org/10.1200/jco.20.03502. e-pub ahead of print 2021/04/28
Jimenez Jimenez A, Komanduri K, Brown S, Wang T, Pereira D, Goodman M, et al. Improved GRFS after posttransplant cyclophosphamide-based vs ATG-based HLA-mismatched unrelated donor transplant. Blood Adv. 2022;6:4491–500. https://doi.org/10.1182/bloodadvances.2022007596. e-pub ahead of print 2022/07/07
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transpl: J Am Soc Blood Marrow Transplant. 2009;15:1628–33. https://doi.org/10.1016/j.bbmt.2009.07.004. e-pub ahead of print 2009/11/10
Chang YJ, Pei XY, Huang XJ. Haematopoietic stem-cell transplantation in China in the era of targeted therapies: current advances, challenges, and future directions. Lancet Haematol. 2022;9:e919–e929. https://doi.org/10.1016/s2352-3026(22)00293-9. e-pub ahead of print 2022/12/02
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: I. The 2014 Diagnosis and Staging Working Group report. Biol Blood Marrow Transpl: J Am Soc Blood Marrow Transplant. 2015;21:389–401.e381. https://doi.org/10.1016/j.bbmt.2014.12.001. e-pub ahead of print 2014/12/23
Verneris MR, Lee SJ, Ahn KW, Wang HL, Battiwalla M, Inamoto Y, et al. HLA Mismatch Is Associated with Worse Outcomes after Unrelated Donor Reduced-Intensity Conditioning Hematopoietic Cell Transplantation: An Analysis from the Center for International Blood and Marrow Transplant Research. Biol Blood Marrow Transpl: J Am Soc Blood Marrow Transplant. 2015;21:1783–9. https://doi.org/10.1016/j.bbmt.2015.05.028. e-pub ahead of print 2015/06/10
Jo T, Arai Y, Kondo T, Mizuno S, Hirabayashi S, Inamoto Y, et al. Advantages of peripheral blood stem cells from unrelated donors versus bone marrow transplants in outcomes of adult acute myeloid leukemia patients. Cytotherapy. 2022;24:1013–25. https://doi.org/10.1016/j.jcyt.2022.05.009. e-pub ahead of print 2022/06/22
Arcuri LJ, Hamerschlak N, Rocha V, Bonfim C, Kerbauy MN. Outcomes after Haploidentical Hematopoietic Cell Transplantation with Post-Transplantation Cyclophosphamide: A Systematic Review and Meta-Analysis Comparing Myeloablative with Reduced-Intensity Conditioning Regimens and Bone Marrow with Peripheral Blood Stem Cell Grafts. Transpl Cell Ther. 2021;27:782.e781–782.e787. https://doi.org/10.1016/j.jtct.2021.06.011. e-pub ahead of print 2021/06/20
Gahrton G, Iacobelli S, Bandini G, Björkstrand B, Corradini P, Crawley C, et al. Peripheral blood or bone marrow cells in reduced-intensity or myeloablative conditioning allogeneic HLA identical sibling donor transplantation for multiple myeloma. Haematologica. 2007;92:1513–8. https://doi.org/10.3324/haematol.11353. e-pub ahead of print 2007/11/21
Petersdorf EW, Hansen JA, Martin PJ, Woolfrey A, Malkki M, Gooley T, et al. Major-histocompatibility-complex class I alleles and antigens in hematopoietic-cell transplantation. N. Engl J Med. 2001;345:1794–800. https://doi.org/10.1056/NEJMoa011826. e-pub ahead of print 2001/12/26
Matsuno N, Wake A, Uchida N, Ishiwata K, Araoka H, Takagi S, et al. Impact of HLA disparity in the graft-versus-host direction on engraftment in adult patients receiving reduced-intensity cord blood transplantation. Blood. 2009;114:1689–95. https://doi.org/10.1182/blood-2008-12-194696. e-pub ahead of print 2009/06/19
Finke J, Schmoor C, Lang H, Potthoff K, Bertz H. Matched and mismatched allogeneic stem-cell transplantation from unrelated donors using combined graft-versus-host disease prophylaxis including rabbit anti-T lymphocyte globulin. J Clin Oncol: Off J Am Soc Clin Oncol. 2003;21:506–13. https://doi.org/10.1200/jco.2003.03.129. e-pub ahead of print 2003/02/01
Metheny L, de Lima M. Hematopoietic stem cell transplant with HLA-mismatched grafts: impact of donor, source, conditioning, and graft versus host disease prophylaxis. Expert Rev Hematol. 2019;12:47–60. https://doi.org/10.1080/17474086.2019.1562331. e-pub ahead of print 2018/12/26
Ruutu T, Gratwohl A, de Witte T, Afanasyev B, Apperley J, Bacigalupo A, et al. Prophylaxis and treatment of GVHD: EBMT-ELN working group recommendations for a standardized practice. Bone marrow Transplant. 2014;49:168–73. https://doi.org/10.1038/bmt.2013.107. e-pub ahead of print 2013/07/31
Wang Y, Liu QF, Lin R, Yang T, Xu YJ, Mo XD, et al. Optimizing antithymocyte globulin dosing in haploidentical hematopoietic cell transplantation: long-term follow-up of a multicenter, randomized controlled trial. Sci Bull. 2021;66:2498–505. https://doi.org/10.1016/j.scib.2021.06.002. e-pub ahead of print 2021/12/30
Luo Y, Jin M, Tan Y, Zhao Y, Shi J, Zhu Y, et al. Antithymocyte globulin improves GVHD-free and relapse-free survival in unrelated hematopoietic stem cell transplantation. Bone marrow Transplant. 2019;54:1668–75. https://doi.org/10.1038/s41409-019-0502-8. e-pub ahead of print 2019/03/15
Kim HJ, Min WS, Cho BS, Eom KS, Kim YJ, Min CK, et al. Successful prevention of acute graft-versus-host disease using low-dose antithymocyte globulin after mismatched, unrelated, hematopoietic stem cell transplantation for acute myelogenous leukemia. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2009;15:704–17. https://doi.org/10.1016/j.bbmt.2009.02.010. e-pub ahead of print 2009/05/20
Kawamura K, Kanda J, Fuji S, Murata M, Ikegame K, Yoshioka K, et al. Impact of the presence of HLA 1-locus mismatch and the use of low-dose antithymocyte globulin in unrelated bone marrow transplantation. Bone marrow Transplant. 2017;52:1390–8. https://doi.org/10.1038/bmt.2017.153. e-pub ahead of print 2017/07/18
Oh H, Loberiza FR Jr, Zhang MJ, Ringdén O, Akiyama H, Asai T, et al. Comparison of graft-versus-host-disease and survival after HLA-identical sibling bone marrow transplantation in ethnic populations. Blood. 2005;105:1408–16. https://doi.org/10.1182/blood-2004-06-2385. e-pub ahead of print 2004/10/16
Kanda J, Brazauskas R, Hu ZH, Kuwatsuka Y, Nagafuji K, Kanamori H, et al. Graft-versus-Host Disease after HLA-Matched Sibling Bone Marrow or Peripheral Blood Stem Cell Transplantation: Comparison of North American Caucasian and Japanese Populations. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2016;22:744–51. https://doi.org/10.1016/j.bbmt.2015.12.027. e-pub ahead of print 2016/01/15
Wang L, Kong P, Zhang C, Gao L, Zhu L, Liu J, et al. Outcomes of patients with hematological malignancies who undergo unrelated donor hematopoietic stem cell transplantation with ATG-Fresenius versus ATG-Genzyme. Ann Hematol. 2023;102:1569–79. https://doi.org/10.1007/s00277-023-05220-7. e-pub ahead of print 2023/04/25
Bolaños-Meade J, Hamadani M, Wu J, Al Malki MM, Martens MJ, Runaas L, et al. Post-Transplantation Cyclophosphamide-Based Graft-versus-Host Disease Prophylaxis. N. Engl J Med. 2023;388:2338–48. https://doi.org/10.1056/NEJMoa2215943. e-pub ahead of print 2023/06/21
Nagler A, Labopin M, Swoboda R, Schroeder T, Hamladji RM, Griskevicius L, et al. Post-transplant cyclophosphamide, calcineurin inhibitor, and mycophenolate mofetil compared to anti-thymocyte globulin, calcineurin inhibitor, and methotrexate combinations as graft-versus-host disease prophylaxis post allogeneic stem cell transplantation from sibling and unrelated donors in patients with acute myeloid leukemia: a study on behalf of the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Bone marrow Transplant. 2024;59:1012–21. https://doi.org/10.1038/s41409-024-02284-5. e-pub ahead of print 2024/04/14
Rimando J, McCurdy SR, Luznik L. How I prevent GVHD in high-risk patients: posttransplant cyclophosphamide and beyond. Blood. 2023;141:49–59. https://doi.org/10.1182/blood.2021015129. e-pub ahead of print 2022/04/12
Al Malki MM, Tsai NC, Palmer J, Mokhtari S, Tsai W, Cao T, et al. Posttransplant cyclophosphamide as GVHD prophylaxis for peripheral blood stem cell HLA-mismatched unrelated donor transplant. Blood Adv. 2021;5:2650–9. https://doi.org/10.1182/bloodadvances.2021004192. e-pub ahead of print 2021/06/23
Mehta RS, Saliba RM, Chen J, Rondon G, Hammerstrom AE, Alousi A, et al. Post-transplantation cyclophosphamide versus conventional graft-versus-host disease prophylaxis in mismatched unrelated donor haematopoietic cell transplantation. Br J Haematol. 2016;173:444–55. https://doi.org/10.1111/bjh.13977. e-pub ahead of print 2016/03/08
Shaw BE, Jimenez-Jimenez AM, Burns LJ, Logan BR, Khimani F, Shaffer BC, et al. Three-Year Outcomes in Recipients of Mismatched Unrelated Bone Marrow Donor Transplants Using Post-Transplantation Cyclophosphamide: Follow-Up from a National Marrow Donor Program-Sponsored Prospective Clinical Trial. Transplant Cell Ther. 2023;29:208.e201–208.e206. https://doi.org/10.1016/j.jtct.2022.12.017. e-pub ahead of print 2022/12/31
Prem S, Atenafu EG, Al-Shaibani Z, Loach D, Law A, Lam W, et al. Low rates of acute and chronic GVHD with ATG and PTCy in matched and mismatched unrelated donor peripheral blood stem cell transplants. Eur J Haematol. 2019;102:486–93. https://doi.org/10.1111/ejh.13230. e-pub ahead of print 2019/03/30
Walker I, Panzarella T, Couban S, Couture F, Devins G, Elemary M, et al. Pretreatment with anti-thymocyte globulin versus no anti-thymocyte globulin in patients with haematological malignancies undergoing haemopoietic cell transplantation from unrelated donors: a randomised, controlled, open-label, phase 3, multicentre trial. Lancet Oncol. 2016;17:164–73. https://doi.org/10.1016/s1470-2045(15)00462-3. e-pub ahead of print 2016/01/03
Soiffer RJ, Kim HT, McGuirk J, Horwitz ME, Johnston L, Patnaik MM, et al. Prospective, Randomized, Double-Blind, Phase III Clinical Trial of Anti-T-Lymphocyte Globulin to Assess Impact on Chronic Graft-Versus-Host Disease-Free Survival in Patients Undergoing HLA-Matched Unrelated Myeloablative Hematopoietic Cell Transplantation. J Clin Oncol: Off J Am Soc Clin Oncol. 2017;35:4003–11. https://doi.org/10.1200/jco.2017.75.8177. e-pub ahead of print 2017/10/19
Nagler A, Labopin M, Kröger N, Schroeder T, Gedde-Dahl T, Eder M, et al. The role of anti-thymocyte globulin in allogeneic stem cell transplantation (HSCT) from HLA-matched unrelated donors (MUD) for secondary AML in remission: a study from the ALWP /EBMT. Bone marrow Transplant. 2023;58:1339–47. https://doi.org/10.1038/s41409-023-02095-0. e-pub ahead of print 2023/09/03
Ayuk FA, Atassi N, Schuch G, Mina S, Fang L, Bokemeyer C, et al. Complement-dependent and complement-independent cytotoxicity of polyclonal antithymocyte globulins in chronic lymphocytic leukemia. Leuk Res. 2008;32:1200–6. https://doi.org/10.1016/j.leukres.2007.12.011. e-pub ahead of print 2008/02/06
Grüllich C, Ziegler C, Finke J. Rabbit anti T-lymphocyte globulin induces apoptosis in peripheral blood mononuclear cell compartments and leukemia cells, while hematopoetic stem cells are apoptosis resistant. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2009;15:173–82. https://doi.org/10.1016/j.bbmt.2008.11.014. e-pub ahead of print 2009/01/27
Ayuk F, Maywald N, Hannemann S, Larsen U, Zander A, Kröger N. Comparison of the cytotoxicity of 4 preparations of anti-T-cell globulins in various hematological malignancies. Anticancer Res. 2009;29:1355–60. e-pub ahead of print 2009/05/06
Ljungman P, de la Camara R, Robin C, Crocchiolo R, Einsele H, Hill JA, et al. Guidelines for the management of cytomegalovirus infection in patients with haematological malignancies and after stem cell transplantation from the 2017 European Conference on Infections in Leukaemia (ECIL 7). Lancet Infect Dis. 2019;19:e260–e272. https://doi.org/10.1016/s1473-3099(19)30107-0. e-pub ahead of print 2019/06/04
Styczynski J, van der Velden W, Fox CP, Engelhard D, de la Camara R, Cordonnier C, et al. Management of Epstein-Barr Virus infections and post-transplant lymphoproliferative disorders in patients after allogeneic hematopoietic stem cell transplantation: Sixth European Conference on Infections in Leukemia (ECIL-6) guidelines. Haematologica. 2016;101:803–11. https://doi.org/10.3324/haematol.2016.144428. e-pub ahead of print 2016/07/02
Li SS, Zhang N, Jia M, Su M. Association Between Cytomegalovirus and Epstein-Barr Virus Co-Reactivation and Hematopoietic Stem Cell Transplantation. Front Cell Infect Microbiol. 2022;12:818167 https://doi.org/10.3389/fcimb.2022.818167. e-pub ahead of print 2022/04/12
Li W, Li C, Xia W, Li X. HLA-DQB1*06 and breadth of Nef core region-specific T-cell response are associated with slow disease progression in antiretroviral therapy-naive Chinese HIV-1 subtype B patients. Hum Vaccines immunotherapeutics. 2017;13:2341–7. https://doi.org/10.1080/21645515.2017.1340138. e-pub ahead of print 2017/08/05
Ou G, Xu H, Yu H, Liu X, Yang L, Ji X, et al. The roles of HLA-DQB1 gene polymorphisms in hepatitis B virus infection. J Transl Med. 2018;16:362 https://doi.org/10.1186/s12967-018-1716-z. e-pub ahead of print 2018/12/20
Odeberg J, Söderberg-Nauclér C. Reduced expression of HLA class II molecules and Iinterleukin-10- and transforming growth factor beta1-independent suppression of T-cell proliferation in human cytomegalovirus-infected macrophage cultures. J Virol. 2001;75:5174–81. https://doi.org/10.1128/jvi.75.11.5174-5181.2001. e-pub ahead of print 2001/05/03
Fleischhauer K, Beelen DW. HLA mismatching as a strategy to reduce relapse after alternative donor transplantation. Semin Hematol. 2016;53:57–64. https://doi.org/10.1053/j.seminhematol.2016.01.010. e-pub ahead of print 2016/03/24
Flomenberg N, Baxter-Lowe LA, Confer D, Fernandez-Vina M, Filipovich A, Horowitz M, et al. Impact of HLA class I and class II high-resolution matching on outcomes of unrelated donor bone marrow transplantation: HLA-C mismatching is associated with a strong adverse effect on transplantation outcome. Blood. 2004;104:1923–30. https://doi.org/10.1182/blood-2004-03-0803. e-pub ahead of print 2004/06/12
Lee SJ, Klein J, Haagenson M, Baxter-Lowe LA, Confer DL, Eapen M, et al. High-resolution donor-recipient HLA matching contributes to the success of unrelated donor marrow transplantation. Blood. 2007;110:4576–83. https://doi.org/10.1182/blood-2007-06-097386. e-pub ahead of print 2007/09/06
Pidala J, Lee SJ, Ahn KW, Spellman S, Wang HL, Aljurf M, et al. Nonpermissive HLA-DPB1 mismatch increases mortality after myeloablative unrelated allogeneic hematopoietic cell transplantation. Blood. 2014;124:2596–606. https://doi.org/10.1182/blood-2014-05-576041. e-pub ahead of print 2014/08/28
Acknowledgements
This research was supported by grants from the National Natural Science Foundation of China (Grant No. 82170205, 82300240).
Funding
This research was supported by grants from the National Natural Science Foundation of China (Grant No. 82170205, 82300240).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by Lin Li, Yi Chen, Ting Chen and Yajing Xu. The first draft was written by Lin Li and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval & consent to participate
All methods were performed in accordance with the relevant guidelines and regulations. Ethical approval was obtained from the Clinical Research Ethics Committee of the First Affiliated Hospital, Zhejiang University School of Medicine (No. IIT20230944A). Informed consent was obtained from all participants prior to their involvement in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, L., Chen, Y., Chen, T. et al. Mismatched unrelated donors allogeneic hematopoietic stem cell transplantation with antithymocyte globulin for hematological malignancies: a multicenter retrospective study in China. Bone Marrow Transplant 60, 201–210 (2025). https://doi.org/10.1038/s41409-024-02454-5
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41409-024-02454-5